Abstract
Background
Multifocality in breast carcinoma is associated with an increased propensity to metastasis. However, it is not clear whether this propensity manifests in the form of macrometastases or as presumably less-significant low-volume metastatic disease.
Methods
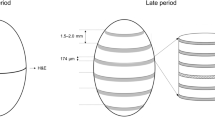
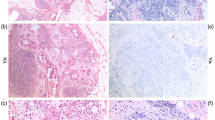
A total of 948 cases of invasive breast carcinoma documented in large-format histology sections and assessed with detailed radiologic–pathologic correlation were categorized as unifocal, multifocal, or diffuse on the basis of the subgross distribution of the invasive component. Rates of macrometastases (>2 mm), micrometastases (0.2–2 mm), and isolated tumor cells (<0.2 mm) in these categories were compared. The influence of tumor size and histology grade on lymph node positivity rates was also tested.
Results
Macrometastases were present in 20.4 % (112 of 550) of unifocal, 48.3 % (172 of 356) of multifocal, and 61.9 % (26 of 42) of diffuse cases (P < 0.0001). Among the macrometastatic cases, more than three nodes were involved in 18.9 % (21 of 112) of unifocal, 35.5 % (61 of 172) of multifocal, and 50.0 % (13 of 26) of diffuse cases. The rates of micrometastases (5.1, 5.1, and 2.4 % unifocal, multifocal, and diffuse, respectively) and isolated tumor cells (4.5, 3.7, and 2.4 % unifocal, multifocal, and diffuse, respectively) were low and similar in all examined categories. The relative risk (RR) of having macrometastatic disease was approximately doubled (RR 2.3726, P < 0.0001) in multifocal and tripled (RR 3.0562, P < 0.0001) in diffuse compared to unifocal cases. The findings were similar for all size categories, tumor grade categories, and sentinel lymph nodes, as well as all examined lymph nodes.
Conclusions
The significantly increased lymph node positivity rates in multifocal and diffuse invasive breast carcinomas results from large-volume macrometastatic disease.

Similar content being viewed by others
References
Gallager HS, Martin JE. The study of mammary carcinoma by mammography and whole organ sectioning. Cancer. 1969;23:855–73.
Egan RI. Multicentric breast carcinomas: clinical–radiographic–pathologic whole organ studies and 10-year survival. Cancer. 1982;49:1123–30.
Holland R, Veling SH, Mravunac M, et al. Histologic multifocality of Tis, T1–2 breast carcinomas. Implications for clinical trials of breast-conserving surgery. Cancer. 1985;56:979–90.
Connolly JL, Harris JR, Schnitt SJ. Understanding the distribution of cancer within the breast is important for optimizing breast-conserving treatment (editorial). Cancer. 1995;76:1–3.
Cabioglu N, Ozmen V, Kaya H, et al. Increased lymph node positivity in multifocal and multicentric breast cancer. J Am Coll Surg. 2009;208:67–74.
Yerushalmi R, Kennecke H, Woods E, et al. Does multicentric/multifocal breast cancer differ from unifocal breast cancer? An analysis of survival and contralateral breast cancer incidence. Breast Cancer Res Treat. 2009;117:365–70.
Jackson PA, Merchant W, McCormick CJ, et al. A comparison of large block macrosectioning and conventional techniques in breast pathology. Virchows Arch. 1994;425:243–8.
Biesemier KW, Alexander CM. Enhancement of mammographic–pathologic correlation utilizing large format histology for malignant breast diseases. Semin Breast Dis. 2005;8:152–62.
Tot T, Tabár L. The role of radiologic–pathologic correlation in diagnosing early breast cancer: the pathologist’s perspective. Virchows Arch. 2011;458:125–31.
Tot T. Clinical relevance of the distribution of the lesions in 500 consecutive breast cancer cases documented in large-format histological sections. Cancer. 2007;110:2551–60.
Tot T. The metastastic capacity of multifocal breast carcinomas: extensive tumors versus tumors of limited extent. Hum Pathol. 2009;40:199–205.
Tot T, Pekár Gy, Hofmeyer S, et al. The distribution of the lesions in 1–14-mm invasive breast carcinomas and its relation to metastatic potential. Virchows Arch. 2009;445:109–15.
Tot T, Gere M, Pekár Gy, et al. Breast cancer multifocality, disease extent and survival. Hum Pathol. 2011: 42:1761–9.
Tot T. The diffuse type of invasive lobular carcinoma of the breast: morphology and prognosis. Virchows Arch. 2003;443:718–24.
Tavassoli FA, Devilee P, eds. Tumors of the breast and female genital organs. In: World Health Organization classification of tumours: pathology and genetics. Lyon: IARC Press; 2003. p. 49.
Weissenbacher TM, Zschage M, Janni W, et al. Multicentric and multifocal versus unifocal breast cancer: is the tumor–node–metastasis classification justified? Breast Cancer Res Treat. 2010;122:27–34.
Andea AA, Wallis T, Newman LA, et al. Pathologic analysis of tumor size and lymph node status in multifocal/multicentric breast carcinoma. Cancer. 2002;94:1383–90.
Andea AA, Bouwman D, Wallis T, et al. Correlation of tumor volume and surface area with lymph node status in patients with multifocal/multicentric breast carcinoma. Cancer. 2004;100:20–7.
Coombs NJ, Boyages J. Multifocal and multicentric breast cancer: does each focus matter? J Clin Oncol. 2005;23:7497–502.
Pedersen L, Gunnarsdottir KA, Rasmussen BB, et al. The prognostic influence of multifocality in breast cancer patients. Breast. 2004;13:188–93.
Patani N, Mokbel K. Clinical significance of sentinel lymph node isolated tumor cells in breast cancer. Breast Cancer Res Treat. 2011;127:325–34.
Tot T, Tabár L, Dean PB. Practical breast pathology. Stuttgart, New York: Thieme; 2002. pp. 116–23.
AJCC staging handbook. 6th ed. New York: Springer; 2002.
Elston CW, Ellis IO. Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large series with long-term follow-up. Histopathology. 1991;19:403–10.
Luttges J, Kalbfleisch H, Prinz P. Nipple involvement and multicentricity in breast cancer. A study of whole organ sections. J Cancer Res Clin Oncol. 1987;113:481–7.
Saha S, Sirop S, Korant A, et al. Nodal positivity in breast cancer correlated with the number of lesions detected by magnetic resonance imaging versus mammogram. Am J Surg. 2011;201:290–5.
Haussami N, Ciatto S, Macaskill P, et al. Accuracy and surgical impact of magnetic resonance imaging in breast cancer staging: systemic review and meta-analysis in detection of multifocal and multicentric cancer. J Clin Oncol. 2008;26:3248–68.
Boyages J, Jajashinghe UW, Coombs N. Multifocal breast cancer and survival: each focus does matter particularly for larger tumours. Eur J Cancer. 2010;46:1990–6.
Spillane AJ, Brennan ME. Accuracy of sentinel lymph node biopsy in large and multifocal/multicentric breast carcinoma—a systematic review. EJCO. 2011;37:371–85.
Giuliani AE, Hunt KK, Ballman KV, et al. Axillary dissection vs. no axillary dissection in women with invasive breast cancer and sentinel node metastasis. JAMA. 2011;305:569–75.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tot, T. Axillary Lymph Node Status in Unifocal, Multifocal, and Diffuse Breast Carcinomas: Differences Are Related to Macrometastatic Disease. Ann Surg Oncol 19, 3395–3401 (2012). https://doi.org/10.1245/s10434-012-2346-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-012-2346-y