Abstract
Introduction
Sentinel lymph node mapping (SLNM) with multilevel sections (MLS) and cytokeratin immunohistochemistry (CK-IHC) of sentinel lymph nodes (SLNs) upstages 15–20% of patients (pts). False-positive SLNs occur in breast cancer due to mechanical transport of cells during mapping procedures, or to pre-existing benign cellular inclusions. Our prospective study evaluated whether colorectal mapping procedures alone caused false positives.
Methods
A total of 314 pts underwent SLNM with blue dye. Ninety of the pts underwent a second mapping in normal bowel away from the primary tumor. The first 1–5 blue nodes near the primary tumor were marked as SLNs; those near the second injection site were marked as nontumor SLNs (nt-SLNs). All SLNs and nt-SLNs were evaluated by MLS and CK-IHC.
Results
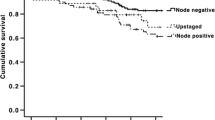
Of 314 pts, 30 had benign tumor and 284 had invasive cancer. SLNM was successful in 274/284 (96.5%) invasive cancer pts, with 728 SLNs identified. Forty-six of the 274 pts (16.8%) had low-volume metastasis in 57 SLNs: 31 pts (11.3%) had 38 SLNs with micrometastasis (>0.2 mm, ≤2 mm), while 15 pts (5.5%) had 19 SLNs with isolated tumor cells (≤0.2 mm). For 100 pts with second SLNM (70/90 pts successfully mapped with 102 nt-SLNs), or with SLNM of benign pathology (30/30 pts successfully mapped with 88 SLNs), there were no false positives in any of 190 nodes (P < 0.001).
Conclusion
No false positives due to mechanical transport of cells or to benign cellular inclusions were identified in 190 lymph nodes from 100 patients with SLNM in benign bowel.
Similar content being viewed by others
References
Saha S, Dan A, Viehl C, Zuber M, Wiese D. Sentinel lymph node mapping in colon and rectal cancer: its impact on staging, limitations, and pitfalls. Cancer Treat Res. 2005;127:105–22.
Greene F, Page D, Fleming I, Fritz A, Balch C, Haller D, Morrow M. AJCC cancer staging manual, 6th ed. New York: Springer-Verlag; 2002.
Carter B, Jensen R, Simpson J, Page D. Benign transport of breast epithelium into axillary lymph nodes after biopsy. Am J Clin Pathol. 2000;113:259–65.
Diaz N, Cox C, Ebert M, Clark J, Vrcel V, Stowell N, et al. Benign mechanical transport of breast epithelial cells to sentinel lymph nodes. Am J Surg Pathol. 2005;28:1641–5.
Diaz N, Vrcel V, Centeno B, Muro-Cacho C. Modes of benign mechanical transport of breast epithelial cells to axillary lymph nodes. Adv Anat Pathol. 2005;12:7–9.
Diaz N, Mayes J, Vrcel V. Breast epithelial cells in dermal angiolymphatic spaces: a manifestation of benign mechanical transport. Hum Pathol. 2005;36:310–3.
Tamhane R, Dahlstrom J, McCallum D, Buckingham M. The clinical significance of cytokeratin-positive cells in lymph nodes at the time of mastectomy from patients with ductal carcinoma-in-situ. Ann Surg Oncol. 2002;9:999–1003.
King T, Ganaraj A, Fey J, et al. Cytokeratin-positive cells in sentinel lymph nodes in breast cancer are not random events: experience in patients undergoing prophylactic mastectomy. Cancer. 2004;101:926–33.
Saha S, Dan A, Viehl C, Zuber M, Wiese D. Sentinel lymph node mapping in colon and rectal cancer: its impact on staging, limitations and pitfalls. In: Leong S, Kitagawa Y, Kitajima M, editors. Selective sentinel lymphadenectomy for human solid cancer. New York: Springer-Verlag; 2005. p. 105-22.
Rao R, Taylor J, Palmer J, Jennings W. Breast cancer pseudometastasis in a sentinel lymph node with cytokeratin-positive debris. Breast J. 2005;11:134–7.
Rosenberg R, Hoos A, Mueller J, et al. Prognostic significance of cytokeratin-20 reverse transcriptase polymerase chain reaction in lymph nodes of node-negative colorectal cancer patients. J Clin Oncol. 2002;20:1049–1055.
Davies M, Arumugam PJ, Shah VI, Watkins A, Roger Morgan A, Carr ND, et al. The clinical significance of lymph node micrometastasis in stage I and stage II colorectal cancer. Clin Transl Oncol. 2008;10:175–9.
Bianchi M, Tono L. Contribution to the study of epithelial inclusions of the lymph nodes. Anatomo-clinical considerations on a case of glandular inclusions of the axillary lymph nodes. Arch De Vecchi Anat Patol. 1950, 30:307–19.
Fragetta F, Vasquez E. Epithelial inclusion in axillary lymph node associated with a breast carcinoma: report of a case with a review of the literature. Pathol Res Pract. 1999;195:263–6.
Schneider, V. Benign glandular lymph node inclusions. Diagn Gynecol Obstet. 1980;2:313–20.
Brooks J, LiVolsi V, Pietra G. Mesothelial inclusions in mediastinal lymph nodes mimicking metastatic carcinoma. Am J Clin Pathol. 1990;93:741–8.
Yakoushina T, Morotti R, Strauchen J, Unger P. Renal benign epithelial nodal inclusions. Ann Diagn Pathol. 2008;12:181–6.
Marques B, Gay G, Jozan S, Mirouze A, David J. Embryologic origin of salivary inclusions in the parotid lymph nodes. Bull Assoc Anat (Nancy). 1983;67:219–28.
Peng Y, Ashfaq R, Ewing G, Leitch A, Mohlberg K. False-positive sentinel lymph nodes in breast cancer patients caused by benign glandular inclusions: report of three cases and review of the literature. Am J Clin Pathol. 2008;130:21–7.
Turner R, Nora D, Trocha S, Bilchik A. Colorectal carcinoma staging. Frequency and nature of cytokeratin positive cells in sentinel and non-sentinel lymph nodes. Arch Pathol Lab Med. 2003;127:673–9.
Redston M, Compton C, Miedema B, Niedzwiecki B, et al. Analysis of micrometastatic disease in sentinel lymph nodes from resectable colon cancer: results of Cancer and Leukemia Group B Trial 80001. J Clin Oncol. 2006;24:878–83.
Wong JH, Johnson DS, Namiki T, Tauchi-Nishi P. Validation of ex vivo lymphatic mapping in hematoxylin-eosin node-negative carcinoma of the colon and rectum. Ann Surg Oncol. 2004;11:772–7.
van Schaik PM, van der Linden JC, Ernst MF, Gelderman WA, Bosscha K. Ex vivo sentinel lymph node “mapping” in colorectal cancer. Eur J Surg Oncol. 2007;33:1177–82.
Acknowledgment
The authors thank Drs. Julio Badin, Peter Ng, Nader Bassily, Weimin Liu, Ernesto Quiachon, and Aamir Ahsan for their participation in the pathologic evaluation of the cases.
DISCLOSURES
No commercial or other disclosures are reported by the authors of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wiese, D., Saha, S., Yestrepsky, B. et al. A Prospective Study of False-Positive Diagnosis of Micrometastatic Cells in the Sentinel Lymph Nodes in Colorectal Cancer. Ann Surg Oncol 16, 2166–2169 (2009). https://doi.org/10.1245/s10434-009-0497-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-009-0497-2