Abstract
Background
Routine use of intraoperative parathyroid hormone (IOPTH) has been challenged in both unilateral/limited (LE) and bilateral exploration (BE). To investigate this, we assessed the usefulness of IOPTH in surgical management of primary hyperparathyroidism and parathyroid carcinoma (PC).
Methods
Between 1998 and 2006, 1133 patients were explored for hyperparathyroidism: 185 LE, 743 BE with IOPTH, 95 BE without IOPTH, 110 reoperations, and 4 PCs. IOPTH patterns were correlated with parathyroid pathology (single adenoma [SA] or multigland disease [MGD]) and operative success.
Results
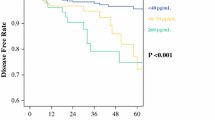
In LE, IOPTH returned to normal in 78% of patients; all patients had SA, and 99% were cured at a mean ± SEM of 1.2 ± .24 years; 22% of LE patients (n = 41) whose IOPTH did not return to normal were converted to BE, and all had MGD. BE with and without IOPTH was equally successful 97% and 98% (P = NS) of the time, respectively. In BE in which IOPTH did not return to normal, 9% of patients remained hypercalcemic; tumor distribution mirrored other BE patients (75% SA, 25% MGD). In reoperations, a normal final IOPTH correlated with cure in 99%; otherwise, 59% had persistent disease. Differential bilateral internal jugular vein IOPTH sampling lateralized disease in 77% of reoperations.
Conclusions
IOPTH is an important adjunct for successful LE by identifying the presence of MGD and avoiding operative failure. IOPTH adds little to BE; however, final IOPTH values may predict persistent disease in BE, reoperations, and PCs.



Similar content being viewed by others
References
Udelsman R, Donovan PI, Sokoll LJ. One hundred consecutive minimally invasive parathyroid explorations. Ann Surg 2000;232:331–9
Duh QY. What’s new in general surgery: endocrine surgery. J Am Coll Surg 2005;201:747–53
Siperstein A, Berber E, Mackey R, Alghoul M, Wagner K, Milas M. Prospective evaluation of sestamibi scan, ultrasonography, and rapid PTH to predict the success of limited exploration for sporadic primary hyperparathyroidism. Surgery 2004;136:872–80
Irvin GL III, Solorzano CC, Carneiro DM. Quick intraoperative parathyroid hormone assay; surgical adjunct to allow limited parathyroidectomy, improve success rate, and predict outcome. World J Surg 2004;28:1287–92
Clark OH. What is new in endocrine surgery. J Am Coll Surg 1998;123:709–11
Grant C, Thompson G, Farley D, Heerden JV. Primary hyperparathyroidism surgical management since the introduction of minimally invasive parathyroidectomy. Arch Surg 2005;140:472–9
Chen H, Eberhard M, Starling J. A comprehensive evaluation of perioperative adjuncts during minimally invasive parathyroidectomy: which is the most reliable? Ann Surg 2005;242:375–83
Stalberg P, Sidhu S, Delbridge L. Intraoperative parathyroid hormone measurement during minimally invasive parathyroidectomy: does it “value-add” to decision making? J Am Coll Surg 2006;203:1–6
Inabnet W. Intraoperative parathyroid hormone monitoring. World J Surg 2004;28:1212–5
Miuria D, Wada N, Arici C, Morita E, Duh Q, Clark OH. Does intraoperative quick parathyroid hormone assay improve the results of parathyroidectomy? World J Surg 2002;26:926–30
Milas M, Weber CJ. Near-total parathyroidectomy is beneficial for patients with secondary and tertiary hyperparathyroidism. Surgery 2004;136:1252–60
Udelsman R, Donovan P. Remedial parathyroid surgery—changing trends in 130 consecutive cases. Ann Surg 2006;244:471–9
Kebebew E, Hwang J, Reiff E, Duh Q, Clark O. Predictors of single gland vs. multigland parathyroid disease in primary hyperparathyroidism. Arch Surg 2006;141:777–82
Sharma J, Mazzaglia P, Milas M, et al. Radionuclide for hyperparathyroidism: which is the best technetium-99m sestamibi modality? Surgery 2006;140:856–65
Carneiro-Pla DM, Solorzano C, Irvin GL. Consequences of targeted parathyroidectomy guided localization studies without intraoperative parathyroid hormone monitoring. J Am Coll Surg 2006;202:715–22
Irvin GL 3rd, Molinari AS, Figueroa C, Carneiro DM. Improved success rate in reoperative parathyroidectomy with intraoperative PTH assay. Ann Surg 1999;229:874–8
Snell SB, Gaar EE, Stevens SP, Flynn MB. Parathyroid cancer, a continued diagnostic and therapeutic dilemma: report of four cases and review of the literature. Am Surg 2003;69:711–6
Busaidy NL, Jimenez C, Habra MA, et al. Parathyroid carcinoma: a 22 year experience. Head Neck 2004;26:716–26
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sharma, J., Milas, M., Berber, E. et al. Value of Intraoperative Parathyroid Hormone Monitoring. Ann Surg Oncol 15, 493–498 (2008). https://doi.org/10.1245/s10434-007-9683-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-007-9683-2