Abstract
Background
The aim of this study was to determine the influence of the different histological subtypes (serous versus non-serous) on the location of nodal metastases in patients undergoing pelvic and para-aortic lymphadenectomies during the initial management of epithelial ovarian tumors.
Methods
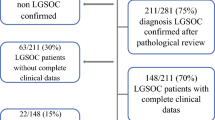
We carried out a retrospective analysis of data concerning patients fulfilling the following inclusion criteria: (1) an epithelial ovarian tumor; (2) a complete pelvic and bilateral para-aortic lymphadenectomy up to the level of the left renal vein; (3) surgical procedures including lymphadenectomies performed before adjuvant chemotherapy; and (4) a description of the distribution of positive nodes removed between pelvic and para-aortic areas. Patients were classified into two groups according to the histological subtypes: serous (group 1) and non-serous (group 2) tumors.
Results
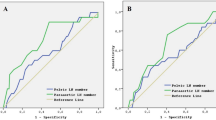
Of patients treated between 1989 and 2005, 148 fulfilled the inclusion criteria: 73 had a serous tumor and 75 a non-serous tumor. Positive nodes were observed in 70 (47%) patients—47 (64%) in group 1 and 23 (31%) in group 2 (P < 0.05). But the distribution of involved nodes between pelvic and para-aortic areas in patients with positive nodes was not statistically different between the two groups. In both groups, the most common site for positive nodes in the para-aortic area was the left para-aortic group: 74% in group 1 and 61% in group 2 (NS).
Conclusions
This series suggests that the histological subtype has no impact on the distribution of positive nodes in pelvic and para-aortic areas in patients with epithelial ovarian tumors.
Similar content being viewed by others
References
Maggioni A, Benedetti Panici PL, Dell’Anna T, et al. Randomised study of systematic lymphadenectomy in patients with epithelial ovarian cancer macroscopically confined to the pelvis. Br J Cancer 2006; 95:699–704
Benedetti-Panici P, Maggioni A, Hacker N, et al. Systematic aortic and pelvic lymphadenectomy versus resection of bulky nodes in optimally debulked advanced ovarian cancer: a randomized clinical trial. J Natl Cancer Inst 2005; 97:560–6
Wu PC, Qu JY, Lang JH, Huang RL, Tang MY, Lian LJ. Lymph node metastasis of ovarian cancer: a preliminary survey of 74 cases of lymphadenectomy. Am J Obstet Gynecol 1986; 155:1103–8
Di Re F, Fontanelli R, Raspagliesi F, Di Re E. Pelvic and para-aortic lymphadenectomy in cancer of the ovary. Baillieres Clin Obstet Gynaecol 1989; 3:131–42
Benedetti-Panici P, Greggi S, et al. Anatomical and pathological study of retroperitoneal nodes in epithelial ovarian cancer. Gynecol Oncol 1993; 51:150–4
Di Re F, Baiocchi G. Value of lymph node assessment in ovarian cancer : Status of the art at the end of second millenium. Int J Gynecol Cancer 2000; 6:435–42
Burghardt E, Pickel H, Lahousen M, Stettner H. Pelvic lymphadenectomy in operative treatment of ovarian cancer. Am J Obstet Gynecol 1986; 155:315–9
Tsumura N, Sakuragi N, Hareyama H, et al. Distribution pattern and risk factors of pelvic and para-aortic lymph node metastasis in epithelial ovarian carcinoma. Int J Cancer 1998; 23:526–30
Morice P, Joulie F, Camatte S, et al. Lymph node involvement in epithelial ovarian cancer: analysis of 276 pelvic and para-aortic lymphadenectomies and surgical implications. J Am Coll Surg 2003; 197:198–205
Meier WJ. Lymphadenectomy in stage I ovarian cancer. Proc ASCO 2000; 19:1541
Takeshima N, Hirai Y, Umayahara K, Fujiwara K, Takizawa, Hasumi K. Lymph node metastasis in ovarian cancer: difference between serous and non-serous primary tumors. Gynecol Oncol 2005; 99:427–31
Chambers SK. Systematic lymphadenectomy in advanced epithelial ovarian cancer: two decades of uncertainty resolved. J Natl Cancer Inst 2005; 97:548–9
Morice P, Pautier P, Lhommé C, Castaigne D. Systematic lymphadenectomy in advanced stage ovarian cancer: is discussion closed? J Natl Cancer Inst 2005; 97:1620–1
Acknowledgements
We would like to acknowledge Lorna Saint Ange for editing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roger, N., Zafrani, Y., Uzan, C. et al. Should Pelvic and Para-aortic Lymphadenectomy Be Different Depending on Histological Subtype in Epithelial Ovarian Cancer?. Ann Surg Oncol 15, 333–338 (2008). https://doi.org/10.1245/s10434-007-9639-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-007-9639-6