Abstract
Background
We evaluated the long-term natural history of gastric cancer after radical gastrectomy and adjuvant chemotherapy through a 15-year follow-up study at a single institute.
Methods
Five hundred patients with advanced gastric adenocarcinoma who received radical gastrectomy and adjuvant chemotherapy were included in this long-term follow-up study. Patients were evaluated by imaging studies and upper gastrointestinal series or endoscopy every 6 months until the 10th year after surgery. Since then, the patients have been followed yearly in the same manner.
Results
The median follow-up period was 190.5 months. The recurrence rate in 5-year survivors was 10.8%. The dominant recurrence pattern was peritoneal carcinomatosis within 5 years and distant metastasis after 5 years post gastrectomy. Tumor stage was a clear-cut prognosticator within 5 years post gastrectomy, but was no longer informative in 5–10 years. At this period, only stage IV (IB–IIIB vs IVM0) was a significantly poor prognosticator. After 10 years, second primary cancer (seven cases) became as important an issue as recurrence of primary gastric cancer (six cases).
Conclusions
In patients with gastric carcinoma treated with radical gastrectomy and adjuvant chemotherapy, late recurrence after 5 years post gastrectomy was not rare. Prognosticators were varied depending on the length of time after surgery. Tumor factors including stage were prognosticators within 5 years post gastrectomy, but tumor factors except stage IV had no prognostic value after 5 years. In the 5–10 years post gastrectomy, only stage IV (IB–IIIB vs IVM0) was a poor prognosticator. Also, after 10 years, there were no prognosticators.
Similar content being viewed by others
Gastric cancer is the most common cancer and is the leading cause of cancer-related death in Korea.1 About half the patients with resected advanced gastric cancer survive more than 5 years.2,3 However, compared with a number of studies concerning the results within 5 years post gastrectomy, there are nearly no data on recurrence or death in gastric cancer patients surviving longer than 5 years post gastrectomy.
The most effective treatment strategy for resectable gastric cancer is radical gastrectomy with or without adjuvant treatment. Since the 1980s, our institution has been treating resectable advanced gastric carcinoma by radical gastrectomy with D2 or more lymph node dissection followed by adjuvant chemotherapy with 5-fluorouracil (5-FU) plus adriamycin, if indicated. In 2001, we reported the results of a 5-year follow-up from this protocol (5-year overall survival, 62.1%; 5-year disease-free survival, 58.4%).3 These results are similar to those of other Asian gastric cancer trials.4,5 This relatively high disease-free survival rate at 5 years means that a worrisome number of patients could be at risk of recurrence after 5 years post gastrectomy.
Understanding and predicting the pattern and timing of recurrence for long-term survivors from gastric cancer are critical for determining successful adjuvant treatment and follow-up program. To identify the long-term natural history of resected advanced gastric carcinoma, we performed a 15-year follow-up study of gastric carcinoma patients who were treated by radical gastrectomy and adjuvant chemotherapy with the same regimen at a single institute.
PATIENTS AND METHODS
Patients
In this long-term follow-up study, we included 500 advanced gastric adenocarcinoma patients who underwent radical gastrectomy and adjuvant chemotherapy with 5-FU plus adriamycin (FA) between 1984 and 1996. At that time, adjuvant chemotherapy was delivered to patients with pathologic stages II–III or IVM0 [American Joint Cancer Committee (AJCC) 1984]. Patients were restaged using the AJCC staging system revised in 20026 to compare the data with survivals reported in recent trials. Analyses in this study were performed based on this staging system revised in 2002.
Radical gastrectomy was performed according to the following standardized operative protocol: i) a total or subtotal gastrectomy depending on the location of the gastric cancer, ii) an en bloc resection of the greater and lesser omentum, and iii) extended lymphadenectomy (D2 or more lymph node dissection, according to the Japanese classification, 1981). Patients with pathologic stage IVM0 were included if en bloc resection of the T4b lesion was guaranteed. Patients were excluded if there was any evidence of peritoneal seeding or tumor at the line of resection. Adjuvant chemotherapy consisted of 5-FU (400 mg/m2 i.v. bolus on days 1, 8, and 15) and adriamycin (40 mg/m2 i.v. bolus on day 1) every 3 weeks for 12 cycles. After this, 5-FU 400 mg/m2 alone was administered weekly for 24 weeks.
Follow-up Evaluation
At the end of the planned adjuvant therapy, a restaging workup was performed with chest x-ray, abdominopelvic computed tomography, radionuclide bone scan, and upper gastrointestinal series (UGI) or esophagogastroduodenoscopy. Patients were evaluated by imaging studies and UGI or endoscopy every 6 months until the 10th year after surgery. Since then, the patients have been followed yearly in the same manner. Recurrences were categorized as locoregional recurrence, peritoneal carcinomatosis, or distant metastasis. Locoregional recurrence was defined as recurrence in the gastric bed, anastomotic site, regional lymph nodes including the para-aortic lymph nodes, or an adjacent structure by direct extension. Peritoneal carcinomatosis was documented based on positive cytology in ascitic fluid or visualization of peritoneal nodules by CT scan. Tumors involving ovaries (Krukenberg’s tumor) were considered to be peritoneal carcinomatosis. Distant metastasis was defined as specific organ involvement via systemic metastasis. Periumbilical nodules and extra-abdominal lymph nodes were considered to be distant metastases. Newly developed tumors in the stomach remnant except for the anastomotic site, were defined as second primary gastric cancer, which was not included in the definition of recurrence.
We evaluated the difference between early recurrence and late recurrence with the cutoff time of 5 years post gastrectomy, based on high recurrence-free survival rate at 5 years.
Analysis of End Points and Statistical Considerations
Recurrence-free survival (RFS) duration was defined as the time from curative surgery to gastric cancer recurrence or the last date at which the patient was known to be free of recurrence (censoring time). Disease-specific survival (DSS) duration was defined as the time from curative surgery to gastric-cancer-specific death that was due to recurrence or adverse events of treatment or the date at which the patient was last confirmed to be alive (censoring time). Nongastric cancer deaths were considered to be censored data in the statistical analysis.
All statistical calculations were carried out using SPSS Windows version 11.0 (SPSS Inc., USA). All P-values were two-sided, and the α-value was set at 0.05. Survival was calculated using the Kaplan–Meier method. A log-rank test was used to compare survival between groups. Prognostic variables that were found by univariate analysis were submitted to multivariate analysis using the Cox’s proportional hazard regression model.
RESULTS
Patient Characteristics and Treatment
The median number of total resected lymph nodes of the enrolled 500 patients was 38 (range 8–144) in D2 or more lymph node dissection. Three hundred eleven patients (62.2%) finished more than 80% of the planned cycles of 5-FU and adriamycin (≥10 cycles) and 5-FU maintenance (≥20 weeks) (chemotherapy completion group). Incomplete chemotherapy (184 of 500, 36.8%) was due to patients’ refusal during the FA cycle (94 of 500, 18.8%) and the 5-FU maintenance (46 of 500, 9.2%) or recurrence during chemotherapy (44 of 500, 8.8%). For the remaining five patients, we could not know if the chemotherapy was completed or not. The median relative dose intensities of 5-FU and adriamycin were 0.94 (range 0.78–1.00) and 0.87 (range 0.15–1.00), respectively. Other characteristics for all 500 patients are summarized in Table 1.
Long-Term Natural History of Gastric Cancer after Gastrectomy and Adjuvant Chemotherapy
The median follow-up duration was 190.5 months (range 17–264). Fourteen patients (2.8%) were lost to follow-up with the median follow-up duration of 39.5 months (range 17–144).
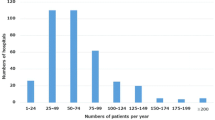
The recurrence pattern analysis is shown in Table 2. Within 5 years post gastrectomy, 205 patients (41.0%) relapsed. During this period, the predominant recurrence pattern was peritoneal carcinomatosis (106 of 205, 51.7%). Among the 295 patients without recurrence at 5 years post gastrectomy, 8.8% of patients (26 of 295) relapsed with the predominant pattern of distant metastasis (34.6%) during the 5–10 years post gastrectomy. After 10 years post gastrectomy, 2.0% of patients (6 of 295) experienced recurrences. The predominant recurrence pattern in this period was also distant metastasis (49.9%). Late recurrences after 5 years post gastrectomy occurred from the 6th to 14th year post gastrectomy (Fig. 1). Nineteen of the 32 late recurrences (59.4%) occurred between the 6th and 7th postsurgical years. Ten-year and 15-year RFS rates were 52.6 and 50.5%, respectively (Table 3).
When considering patients from the same follow-up duration, 269 (53.8%) of 500 patients died. Of the 269 patients who died, 222 (82.5%) died from gastric cancer recurrence, 10 (3.7%) from second primary cancer, 2 (0.7%) from sepsis during chemotherapy, 9 (3.3%) from cerebrovascular accidents, 5 (1.9%) from heart diseases, 6 (2.2%) from traffic accidents, and 15 (5.7%) from other causes. Ten-year and 15-year DSS rates were 54.8 and 53.1%, respectively (Table 3). Overall survival rates including death from any cause were 50.3 and 44.4% at 10 and 15 years, respectively.
Changes of Early and Late Prognosticators During Long-Term Follow-up Periods after Gastrectomy
The changing patterns of early and late prognosticators after gastrectomy are shown in Table 4. Within 5 years post gastrectomy, prognosticators for RFS and DSS were analyzed in all the patients. Significant factors identified by univariate analysis (Table 4) were put into multivariate analysis, and the independent prognosticators for RFS were as follows: completion of chemotherapy (P = .002), stage (P < 0.001), and histology (P < 0.001). The independent prognosticators for DSS were also completion of chemotherapy (P = .002), stage (P < 0.001), and histology (P < 0.001). T stage (T1–3 vs 4) and N stage (N0–2 vs 3) were not included in multivariate analysis because these were linearly dependent covariates of stage (I–III vs IVM0).
For the patients who were recurrence-free at 5 years post gastrectomy, we analyzed risk factors for recurrence or disease-specific death for the 5- to 10-year and more than 10-year post gastrectomy period. Although tumor stage (IB vs II vs IIIA vs IIIB vs IVM0) was a clear-cut prognosticator for both recurrence (P < 0.001; Fig. 2A) and disease-specific death (P < 0.001; Fig. 3A) within 5 years post gastrectomy. Tumor stage itself (IB vs II vs IIIA vs IIIB) was no longer a prognosticator for recurrence (P = .426; Fig. 2B) or disease-specific death (P = .592; Fig. 3B) after 5 years post gastrectomy. In the period of 5–10 years post gastrectomy, we found that only stage IV (IB–IIIB vs IVM0) was a poor prognosticator for recurrence (P < 0.001; Fig. 2B) and disease-specific death (P < 0.001; Fig. 3B). However, stage did not represent any prognostic significance for either recurrence or disease-specific death after 10 years post gastrectomy. During this period, we could not find any prognosticators.
Second Primary Cancer
During the 15-year follow-up period, a total of 19 second primary cancers (SPCs) occurred: seven SPCs within 5 years post gastrectomy, five SPCs in 5–10 years, and seven SPCs after 10 years. Colorectal carcinoma was detected most frequently (8 of 19, 42.1%), followed by second primary gastric carcinoma (5 of 19, 26.3%).
DISCUSSION
The clinical outcomes of resected advanced gastric carcinoma regarding recurrence or survival during long-term follow-up for more than 5 years post gastrectomy have not been well studied. Long-term survival rates, such as the 7- to 15-year survival rate have been reported in only a few studies.7,8 However, the reported survival rates in those studies may have been slightly overestimated because the median follow-up duration was not long enough. In our study, which had a median follow-up duration of 15.9 years, the 10- and 15-year DSS rates were 54.8 and 53.1%, respectively, and the 10- and 15-year RFS rates were 52.6 and 50.5%, respectively. In patients with the stages IB to IVM0, the 15-year survival rates widely ranged from 13.7 to 86.5% in DSS and 13.4 to 84.3% in RFS. As we reported in our previous study,3 based on the favorable results of 5-FU plus adriamycin in advanced gastric cancer,9,10 we treated gastric cancer patients with 5-FU plus adriamycin as an adjuvant chemotherapy from the early 1980s to the late 1990s. Since the late 1990s, we have used 5-FU plus cisplatin as an adjuvant regimen in gastric cancer, as adopted in many institutions. Because our patients were treated with the standardized, extended (D2 or more) gastrectomy and the same adjuvant treatment protocol at a single institute and because of the long, 15.9-year follow-up duration, our long-term survival data represent the natural history of gastric cancer after D2 or more gastrectomy and adriamycin-based adjuvant chemotherapy.
We found that within 5 years post gastrectomy, peritoneal carcinomatosis was the dominant recurrence pattern. This finding is consistent with that of other studies.11,12 In contrast, distant metastasis was the main relapse pattern in the period of 5–10 years and after 10 years post gastrectomy. Recurrences during the early post gastrectomy period may result from infiltrative growth and lymphatic invasion of the tumor.11,12 However, recurrences many years after the treatment may be related to long-lasting tumor dormancy being turned on, especially in distant organs.13,14 The mechanisms behind transition from a dormant to active state remain to be clarified.
After 5 years post gastrectomy, late recurrences (10.8%) in long-term survivors were not rare and occurred even 14 years after gastrectomy. As more than 50% of late recurrences happened in the 6th and 7th year after surgery, a close follow-up may be necessary especially until 7 years after surgery and a follow-up is still necessary even after 10 years. We recommend that patients be evaluated by imaging studies (chest x-ray, abdominopelvic computed tomography, and radionuclide bone scan) and UGI or endoscopy every 6 months until the 10th year after surgery and then followed yearly in the same manner. However, due to interests in cost effectiveness, determining the optimal length of follow-up study remains a controversial issue. From this standpoint, risk factors for late recurrence need to be identified to determine a personalized follow-up schedule for each long-term survivor.
Few studies have reported the characteristics of patients who survived for more than 10 years post gastrectomy.15,16 However, these studies only compared the characteristics between long-term survivors and patients who died from recurrence anytime after surgery, including even early recurrences within 2 years after surgery. As a result, the clinicopathological factors associated with early recurrence in these studies were accentuated rather than the factors associated with true long-term survival. For this reason, we were motivated to identify the true risk factors for late recurrence or death after 5 years post gastrectomy. Therefore, a prognostic analysis in patients surviving 5 years after gastrectomy was performed, after excluding recurrence and death within 5 years post gastrectomy. As reported in many studies,15–18 within 5 years post surgery, various factors such as stage, histology, and the completion of chemotherapy were identified as prognosticators for recurrence or death. However, in long-term survivors who lived more than 5 years post gastrectomy, most prognosticators informative within 5 years post gastrectomy lost their prognostic significance with time. A prognosticator for 5–10 years post gastrectomy was only stage IV (IB–IIIB vs IVM0) for RFS and DSS. Remarkably, stage itself (IB vs II vs IIIA vs IIIB) was no longer a prognosticator for the period of 5–10 years post gastrectomy. More strikingly, stage grouping was not a prognosticator 10 years after surgery.
When we estimated survival (RFS or DSS) in all patients, including patients with recurrence or death within 5 years post gastrectomy, survival curves were well separated from stage IB to stage IVM0. These significant differences in survival were already set during the early postoperative period. These differences were consistent during the late follow-up period, except for patients with stage IVM0. This survival pattern suggests that the stage (IB vs II vs IIIA vs IIIB) cannot predict recurrence or death 5 years after surgery. This may be one of the reasons why researchers need to attempt to identify nomograms that include molecular prognosticators in long-term survivors from curatively resected gastric cancer as well as in patients at the risk of early recurrence.19
The incidence of SPCs (3.8%) in the current study was similar to that of SPC in previous gastric cancer studies.20,21 Colorectal and lung cancers were frequently detected as SPCs in those studies.20,21 In the current study, colorectal cancer also occurred most commonly, but lung cancer was rare (one case). Especially after 10 years post gastrectomy, SPCs (seven cases) became as important an issue as recurrence of primary gastric cancer (six cases), suggesting the prognosis of gastric cancer patients can be influenced by a SPC as well as a primary gastric cancer in this period.
In conclusion, in patients with gastric carcinoma treated with D2 or more gastrectomy and adriamycin-based adjuvant chemotherapy, late recurrence after 5 years post gastrectomy was not rare. Prognosticators were varied depending on the length of time after surgery. Tumor factors including stage were prognosticators within 5-years post gastrectomy, but tumor factors except stage IV had no prognostic value after 5 years. In the 5–10 years post gastrectomy, only stage IV (IB–IIIB vs IVM0) was a poor prognosticator. And after 10 years, there were no prognosticators.
References
Shin HR, Jung KW, Won YJ, Park JG. 139 KCCR-affiliated Hospitals. 2002 Annual Report of the Korea Central Cancer Registry: Based on Registered Data from 139 Hospitals. Cancer Res Treat 2004; 36:103–14
Desai AM, Pareek M, Nightingale PG, Fielding JW. Improving outcomes in gastric cancer over 20 years. Gastric Cancer 2004; 7:196–201
Jeung HC, Rha SY, Noh SH, Min JS, Kim BS, Chung HC. Adjuvant 5-fluorouracil plus doxorubicin in D2-3 resected gastric carcinoma: 15-year experience at a single institute. Cancer 2001; 91:2016–25
Kim JP, Lee JH, Kim SJ, Yu HJ, Yang HK. Clinicopathologic characteristics and prognostic factors in 10783 patients with gastric cancer. Gastric Cancer 1998; 1:125–33
Moriwaki Y, Kunisaki C, Kobayashi S, Harada H, Imai S, Kido Y, Kasaoka C. Progressive improvement of prognosis for patients with gastric cancer (dynamic stage grouping) with increasing survival interval from initial staging: how much longer can a given survivor expect to live? Surgery 2003; 133:135–40
Greene FL, Balch CM, Page DL, et al. AJCC Cancer Staging Manual, 6th ed. (Springer-Verlag, New York, 2002)
Grau JJ, Martin M, Fuster J, et al. Impact of adjuvant chemotherapy in the long-term outcome of patients with resected gastric cancer. J Surg Oncol 2003; 82:234–40
Maehara Y, Moriguchi S, Sakaguchi Y, et al. Adjuvant chemotherapy enhances long-term survival of patients with advanced gastric cancer following curative resection. J Surg Oncol 1990; 45:169–72
Moertel CG, O’Connel M, Lavin PT. Chemotherapy of gastric cancer. 1979 AACR Annual Meeting Proceedings. 1979; 288:20
Brugarolas A, Garcia-Moran M, Lacave AJ. Chemotherapy in advanced gastric cancer: a controlled clinical study. 1975 AACR Annual Meeting Proceedings. 1975; 169:16
Yoo CH, Noh SH, Shin DW, Choi SH, Min JS. Recurrence following curative resection for gastric carcinoma. Br J Surg 2000; 87:236–42
Maehara Y, Hasuda S, Koga T, Tokunaga E, Kakeji Y, Sugimachi K. Postoperative outcome and sites of recurrence in patients following curative resection of gastric cancer. Br J Surg 2000; 87:353–7
Meltzer A. Dormancy and breast cancer. J Surg Oncol 1990; 43:181–8
Naumov GN, MacDonald IC, Weinmeister PM, et al. Persistence of solitary mammary carcinoma cells in a secondary site: a possible contributor to dormancy. Cancer Res 2002; 62:2162–8
Maehara Y, Okuyama T, Oshiro T, Baba H, Adachi Y, Sugimachi K. Analysis of 390 patients surviving 10 years or longer after curative resection for gastric cancer. Oncology 1994; 51:366–71
Adachi Y, Mori M, Maehara Y, Sugimachi K. Long-term survival after resection for advanced gastric carcinoma. J Clin Gastroenterol 1995; 21:208–10
Schlag P, Schreml W, Gaus W, Herfarth C, Linder MM, Queisser W, Trede M. Adjuvant 5-fluorouracil and BCNU chemotherapy in gastric cancer: 3-year results. Recent Results Cancer Res 1982;80: 277–83
Maehara Y, Emi Y, Baba H, Adachi Y, Akazawa K, Ichiyoshi Y, Sugimachi K. Recurrences and related characteristics of gastric cancer. Br J Cancer 1996; 74:975–9
Chen CN, Lin JJ, Chen JJ, et al. Gene expression profile predicts patient survival of gastric cancer after surgical resection. J Clin Oncol 2005; 23:7286–95
Ikeda Y, Saku M, Kishihara F, Maehara Y. Effective follow-up for recurrence or a second primary cancer in patients with early gastric cancer. Br J Surg 2005; 92:235–9
Ikeda Y, Saku M, Kawanaka H, Nonaka M, Yoshida K. Features of second primary cancer in patients with gastric cancer. Oncology 2003; 65:113–7
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented in part at the 42nd Annual Meeting of the American Society of Clinical Oncology, Atlanta, GA, USA. June 2–6, 2006 (abstract No. 4050).
Rights and permissions
About this article
Cite this article
Moon, Y.W., Jeung, HC., Rha, S.Y. et al. Changing Patterns of Prognosticators During 15-Year Follow-Up of Advanced Gastric Cancer after Radical Gastrectomy and Adjuvant Chemotherapy: A 15-Year Follow-Up Study at a Single Korean Institute. Ann Surg Oncol 14, 2730–2737 (2007). https://doi.org/10.1245/s10434-007-9479-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-007-9479-4