Abstract
Background
Limiting surgical morbidity while maintaining staging adequacy is a primary concern in obese patients with uterine malignancy. The goal of this study was to compare the surgical adequacy and postoperative morbidity of three surgical approaches to staging the disease of obese women with uterine cancer.
Methods
The records of all patients with a body mass index (BMI) of ≥35 undergoing primary surgery for uterine corpus cancer at our institution from January 1993 to May 2006 were reviewed. Patients were assigned to three groups on the basis of planned surgical approach—standard laparotomy, laparoscopy, or laparotomy with panniculectomy. Standard statistical tests appropriate to group size were used to compare the three groups.
Results
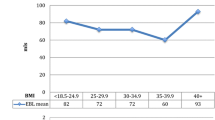
In all, 206 patients with a BMI of ≥35 were grouped as follows: laparotomy, 154 patients; laparoscopy, 25 patients; and laparotomy with panniculectomy, 27 patients. Median BMI was 41 (range, 35–84). Regional lymph nodes were removed in 45% of the laparotomy patients, 40% of the laparoscopy patients, and 70% of the panniculectomy patients (P = .04). Compared with laparotomy, both laparoscopy and panniculectomy yielded higher median pelvic and total lymph node counts (P = .001). Operative time was shortest after standard laparotomy, and blood loss was greatest after panniculectomy. The incidence of all incisional complications was lower for panniculectomy (11%) and laparoscopy (8%) compared with standard laparotomy (35%) (P = .002). On multivariate analysis, a significantly lower risk of total incisional complications was seen for patients undergoing panniculectomy (risk ratio, .25; 95% confidence interval, .071–.88) and laparoscopy (risk ratio, .19; 95% confidence interval, .04–.94).
Conclusions
Both laparoscopic staging and panniculectomy in a standardized fashion were associated with an improved lymph node count and a lower rate of incisional complications than laparotomy alone. Although definitive conclusions are limited by low patient numbers, the substantial decrease in wound complications suggests that these two approaches should be considered for obese patients undergoing uterine cancer staging.
Similar content being viewed by others
References
Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin 2007;57:43–66
Tretli S, Magnus K. Height and weight in relation to uterine corpus cancer morbidity and mortality. A follow-up study of 570,000 women in Norway. Int J Cancer 1990;46:165–72
Tornberg SA, Carstensen JM. Relationship between Quetelet’s index and cancer of breast and female genital tract in 47,000 women followed for 25 years. Br J Cancer 1994;69:358–61
Parazzini F, La Vecchia C, Bocciolone L, Franceschi S. The epidemiology of endometrial cancer. Gynecol Oncol 1991;41:1–16
Executive summary of the clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. Arch Intern Med 1998;158:1855–67
Creasman WT, Morrow CP, Bundy BN, Homesley HD, Graham JE, Heller PB. Surgical pathologic spread patterns of endometrial cancer. A Gynecologic Oncology Group study. Cancer 1987;60(8 Suppl):2035–41
Morrow CP, Bundy BN, Kurman RJ, et al. Relationship between surgical-pathological risk factors and outcome in clinical stage I and II carcinoma of the endometrium: a Gynecologic Oncology Group study. Gynecol Oncol 1991;40:55–65
Boronow RC, Morrow CP, Creasman WT, et al. Surgical staging in endometrial cancer: clinical-pathologic findings of a prospective study. Obstet Gynecol 1984;63:825–32
Homesley HD, Kadar N, Barrett RJ, Lentz SS. Selective pelvic and periaortic lymphadenectomy does not increase morbidity in surgical staging of endometrial carcinoma. Am J Obstet Gynecol 1992;167:1225–30
Larson DM, Johnson K, Olson KA. Pelvic and para-aortic lymphadenectomy for surgical staging of endometrial cancer: morbidity and mortality. Obstet Gynecol 1992;79:998–1001
Girardi F, Petru E, Heydarfadai M, Haas J, Winter R. Pelvic lymphadenectomy in the surgical treatment of endometrial cancer. Gynecol Oncol 1993;49:177–80
Kilgore LC, Partridge EE, Alvarez RD, et al. Adenocarcinoma of the endometrium: survival comparisons of patients with and without pelvic node sampling. Gynecol Oncol 1995;56:29–33
Mohan DS, Samuels MA, Selim MA, et al. Long-term outcomes of therapeutic pelvic lymphadenectomy for stage I endometrial adenocarcinoma. Gynecol Oncol 1998;70:165–71
Everett E, Tamimi H, Greer B, et al. The effect of body mass index on clinical/pathologic features, surgical morbidity, and outcome in patients with endometrial cancer. Gynecol Oncol 2003;90:150–7
Krebs HB, Helmkamp BF. Transverse periumbilical incision in the massively obese patient. Obstet Gynecol 1984;63:241–5
Greer BE, Cain JM, Figge DC, Shy KK, Tamimi HK. Supraumbilical upper abdominal midline incision for pelvic surgery in the morbidly obese patient. Obstet Gynecol 1990;76(3 Pt 1):471–3
Voss SC, Sharp HC, Scott JR. Abdominoplasty combined with gynecologic surgical procedures. Obstet Gynecol 1986;67:181–5
Wright JD, Powell MA, Herzog TJ, et al. Panniculectomy: improving lymph node yield in morbidly obese patients with endometrial neoplasms. Gynecol Oncol 2004;94:436–41
Eltabbakh GH, Shamonki MI, Moody JM, Garafano LL. Hysterectomy for obese women with endometrial cancer: laparoscopy or laparotomy? Gynecol Oncol 2000;78(3 Pt 1):329–35
Scribner DR Jr, Walker JL, Johnson GA, McMeekin DS, Gold MA, Mannel RS. Laparoscopic pelvic and paraaortic lymph node dissection in the obese. Gynecol Oncol 2002;84:426–30
Obermair A, Manolitsas TP, Leung Y, Hammond IG, McCartney AJ. Total laparoscopic hysterectomy versus total abdominal hysterectomy for obese women with endometrial cancer. Int J Gynecol Cancer 2005;15:319–24
Gemignani ML, Curtin JP, Zelmanovich J, Patel DA, Venkatraman E, Barakat RR. Laparoscopic-assisted vaginal hysterectomy for endometrial cancer: clinical outcomes and hospital charges. Gynecol Oncol 1999;73:5–11
Tozzi R, Malur S, Koehler C, Schneider A. Analysis of morbidity in patients with endometrial cancer: is there a commitment to offer laparoscopy? Gynecol Oncol 2005;97:4–9
Abu-Rustum NR, Gemignani ML, Moore K, et al. Total laparoscopic radical hysterectomy with pelvic lymphadenectomy using the argon-beam coagulator: pilot data and comparison to laparotomy. Gynecol Oncol 2003;91:402–9
Martin RC 2nd, Brennan MF, Jaques DP. Quality of complication reporting in the surgical literature. Ann Surg 2002;235:803–13
Hosmer DW, Lemeshow S. A goodness-of-fit test for the multiple regression model. Commun Stat 1980;A10:1043–69
Walker J, Mannel R, Piedmonte M, Schlaerth J, Spirtos N, Speigel G. Phase III trial of laparoscopy (scope) vs laparotomy (open) for surgical resection and comprehensive surgical staging of uterine cancer: a Gynecologic Oncology Group study (abstract). Gynecol Oncol 2006;101:S11–2
Foley K, Lee RB. Surgical complications of obese patients with endometrial carcinoma. Gynecol Oncol 1990;39:171–4
Pavelka JC, Ben-Shachar I, Fowler JM, et al. Morbid obesity and endometrial cancer: surgical, clinical, and pathologic outcomes in surgically managed patients. Gynecol Oncol 2004;95:588–92
Cosin JA, Powell JL, Donovan JT, Stueber K. The safety and efficacy of extensive abdominal panniculectomy at the time of pelvic surgery. Gynecol Oncol 1994;55:36–40
Blomfield PI, Le T, Allen DG, Planner RS. Panniculectomy: a useful technique for the obese patient undergoing gynecological surgery. Gynecol Oncol 1998;70:80–6
Micha JP, Rettenmaier MA, Francis L, Willenberg R, Brown JV. “Medically necessary” panniculectomy to facilitate gynecologic cancer surgery in morbidly obese patients. Gynecol Oncol 1998;69:237–42
Pearl ML, Valea FA, Chalas E. Panniculectomy and supraumbilical vertical midline incisions in morbidly obese gynecologic oncology patients. J Am Coll Surg 1998;186:649–53
Powell JL, Kasparek DK, Connor GP. Panniculectomy to facilitate gynecologic surgery in morbidly obese women. Obstet Gynecol 1999;94:528–31
Hopkins MP, Shriner AM, Parker MG, Scott L. Panniculectomy at the time of gynecologic surgery in morbidly obese patients. Am J Obstet Gynecol 2000;182:1502–5
Tillmanns TD, Kamelle SA, Abudayyeh I, et al. Panniculectomy with simultaneous gynecologic oncology surgery. Gynecol Oncol 2001;83:518–22
Lutman CV, Havrilesky LJ, Cragun JM, et al. Pelvic lymph node count is an important prognostic variable for FIGO stage I and II endometrial carcinoma with high-risk histology. Gynecol Oncol 2006;102:92–7
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented in part at the Society of Gynecologic Oncologists Winter Meeting; Beaver Creek, CO; February 1–3, 2007.
Rights and permissions
About this article
Cite this article
Eisenhauer, E.L., Wypych, K.A., Mehrara, B.J. et al. Comparing Surgical Outcomes in Obese Women Undergoing Laparotomy, Laparoscopy, or Laparotomy With Panniculectomy for the Staging of Uterine Malignancy. Ann Surg Oncol 14, 2384–2391 (2007). https://doi.org/10.1245/s10434-007-9440-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-007-9440-6