Abstract
Background
There are not many publications on the prognostic implications of nodal disease in patients with papillary thyroid cancers (PTC). This study explored the distribution of nodes with respect to the levels, optimal management of the neck for patients with PTC, and its survival advantages.
Methods
Followup of 79 patients with thyroid cancer (59 with PTC) at the National Cancer Institute, Maharagama, Sri Lanka, was analyzed.
Results
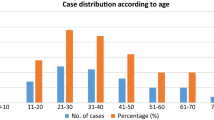
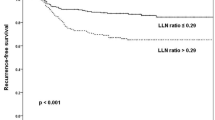
The most common histologic type of all thyroid cancers presenting to the Institute was differentiated PTC which affected 59 patients (74.7%). Of them, 29 (50.0%) had positive lymph node metastases in the neck these nodes were found on clinical examination and confirmed by ultrasound in all. Therfore necessitating a comprehensive neck dissection. Among the patients with nodal disease, 5 had nodes in Level 1 at the time of presentation. All patients in this group had multiple levels of positive nodes. Metachronous nodal disease was found in 9 (31.4%) patients, with a disease-free period ranging from 2 months to 37 years. Among the patients with nodal disease, 13 had a single nodal group involvement and the majority of these were Level 4 nodes (46.2%). Central node (Level 6) involvement was found in nine (15.3%) patients. Multiple nodal group involvement indicating multifocal disease was present in 16 (27.6%) patients. Extracapsular nodal spread at presentation and extracapsular thyroid disease at presentation was 10 (16.9%) and 17 (28.8%), respectively. Nodal neck recurrences during followup were present in 2 patients.
Conclusions
Level 1 nodal metastases was present if 5 (8.5%) patients in our group. It is recommended that Level 1 nodes be explored during neck resection for PTC. Because 27.6% of the patients had multifocal disease, it may be important to recommend inclusion of a Level 1 clearance in the presence of multiple nodal involvement. There is a subgroup of patients who had highly aggressive nodes, indicated by extracapsular penetration, which even after radical clearance and external beam radiotherapy have a tendency to recur locally. This indicates an important prognostic feature of the nodal disease in PTC. Because 27.6% of the patients studies had multifocal nodal disease, we consider a comprehensive nodal clearance is necessary for patients with clinically positive nodes.
Similar content being viewed by others
References
Clark OH. Total thyroidectomy: the treatment of choice for patients with differentiated thyroid cancer. Ann Surg 1982; 196:361–370
Cohn KH, Bäckdahl M, Forsslund G, et al. Biologic considerations and operative strategy in papillary thyroid carcinoma: arguments against the routine performance of total thyroidectomy. Surgery 1984; 96:957–971
DeGroot LJ, Kaplan EL, Straus FH, Shukla MS. Does the method of management of papillary thyroid carcinoma make a difference in outcome? World J Surg 1994; 18:123–130
National Cancer Control Programme of Sri Lanka. Cancer Registry 2000; 10:58–64
Shah JP. Patterns of lymph node metastases from squamous carcinoma of the upper aerodigestive tract. Am J Surg 1990; 160:405–409
Sivanandan R, Soo KC. Pattern of cervical lymph node metastases from papillary thyroid carcinoma. Br J Surg 2001; 99:1241-1244
Gimm O, Rath FW, Dralle H. Pattern of lymph node metastases in papillary thyroid carcinoma. Br J Surg 1997; 85:252-254
Kumar A, Bal CS. Differentiated thyroid cancer. Indian J Pediatr 2003; 70(9):707–713
Simpson WJ, McKinney SE, Carruthers JS, Gospodaarowiccz MK, Sutcliffe SB, Panzarella T. Papillary and follicular cancer. Prognostic factors in 1578 patients. Am J Med 1987; 83: 479–488
Ozaki O, Ito K, Kobayashi K, Suzuki A, Manabe Y. Modified neck dissection for patients with non-advanced, differentiated carcinoma of the thyroid. World J Surg 1988; 12:825–829
Clark OH, Duh QY. Thyroid cancer. Med Clin North Am 1991; 75:211–234
Lee KY, Lore JM Jr. The treatment of metastatic thyroid disease. Otolaryngol Clin North Am 1990; 23:475–493
Ducci M, Appetecchia M, Marzetti M. Neck dissection for surgical treatment of lymphnode metastasis in papillary thyroid carcinoma. J Exp Clin Cancer Res 1997; 16(3):333–335
Gemsenjager E, Perren A, Seifert B, Schuler G, Schweizer I, Heitz PU. Lymph node surgery in papillary thyroid carcinoma. J Am Coll Surg 2003; 197(2):182–190
Khoo ML, Freeman JL. Transcervical superior mediastinal lymphadenectomy in the management of papillary thyroid carcinoma. Head Neck 2003; 25(1):10–14
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Amarasinghe, I.Y., Perera, N.M.A., Bahinathan, N. et al. Review of Distribution of Nodal Disease in Differentiated Thyroid Cancers in an Oncosurgical Center in Sri Lanka. Ann Surg Oncol 14, 1560–1564 (2007). https://doi.org/10.1245/s10434-006-9202-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-006-9202-x