Abstract
Background
The influence of social determinants of health (SDH) on participation in clinical trials for pancreatic cancer is not well understood. In this study, we describe trends and identify disparities in pancreatic cancer clinical trial enrollment.
Patients and Methods
This is a retrospective study of stage I–IV pancreatic cancer patients in the 2004–2016 National Cancer Database. Cohort was stratified into those enrolled in clinical trials during first course of treatment versus not enrolled. Bivariate analysis and logistic regression were used to understand the relationship between SDH and clinical trial participation.
Results
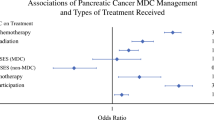
A total of 1127 patients (0.4%) enrolled in clinical trials versus 301,340 (99.6%) did not enroll. Enrollment increased over the study period (p < 0.001), but not for Black patients or patients on Medicaid. The majority enrolled had metastatic disease (65.8%). On multivariate analysis, in addition to year of diagnosis (p < 0.001), stage (p < 0.001), and Charlson score (p < 0.001), increasing age [odds ratio (OR) 0.96, 95% confidence interval (CI) 0.96–0.97], non-white race (OR 0.54, CI 0.44–0.66), living in the South (OR 0.42, CI 0.35–0.51), and Medicaid, lack of insurance, or unknown insurance (0.41, CI 0.31–0.53) were predictors of lack of participation. Conversely, treatment at an academic center (OR 6.36, CI 5.4–7.4) and higher neighborhood education predicted enrollment (OR 2.0, CI 1.55–2.67 for < 7% with no high school degree versus > 21%).
Discussion
Age, race, insurance, and geography are barriers to clinical trial enrollment for pancreatic cancer patients. While overall enrollment increased, Black patients and patients on Medicaid remain underrepresented. After adjusting for cancer-specific factors, SDH are still associated with clinical trial enrollment, suggesting need for targeted interventions.

Similar content being viewed by others
References
Thornton RL, Glover CM, Cené CW, Glik DC, Henderson JA, Williams DR. Evaluating strategies for reducing health disparities by addressing the social determinants of health. Health Affairs (Project Hope). 2016;35(8):1416-23. doi:https://doi.org/10.1377/hlthaff.2015.1357.
Albano JD, Ward E, Jemal A, et al. Cancer mortality in the United States by education level and race. J Natl Cancer Inst. 2007;99(18):1384-94. doi:https://doi.org/10.1093/jnci/djm127.
Kurani SS, McCoy RG, Lampman MA, et al. Association of neighborhood measures of social determinants of health with breast, cervical, and colorectal cancer screening rates in the US Midwest. JAMA Netw Open. 2020;3(3):e200618. doi:https://doi.org/10.1001/jamanetworkopen.2020.0618.
Hernandez ND, Durant R, Lisovicz N, et al. African American cancer survivors' perspectives on cancer clinical trial participation in a safety-net hospital: considering the role of the social determinants of health. J Cancer Educ. 2021;doi:https://doi.org/10.1007/s13187-021-01994-4.
Health NIo. NIH Policy and Guidelines on The Inclusion of Women and Minorities as Subjects in Clinical Research. 2001.
Duma N, Vera Aguilera J, Paludo J, et al. Representation of minorities and women in oncology clinical trials: review of the past 14 years. J Oncol Pract. 2018;14(1):e1-e10. doi:https://doi.org/10.1200/jop.2017.025288.
Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA. 2004;291(22):2720-6. doi:https://doi.org/10.1001/jama.291.22.2720.
Wei K, Hackert T. Surgical treatment of pancreatic ductal adenocarcinoma. Cancers. 2021;13(8)doi:https://doi.org/10.3390/cancers13081971.
Matrisian LM, Berlin JD. The past, present, and future of pancreatic cancer clinical trials. Am Soc Clin Oncol Educ Book. 2016;35:e205-15. doi:https://doi.org/10.1200/edbk_159117.
Bilimoria KY, Stewart AK, Winchester DP, Ko CY. The National Cancer Data Base: a powerful initiative to improve cancer care in the United States. Ann Surg Oncol. 2008;15(3):683-90. doi:https://doi.org/10.1245/s10434-007-9747-3.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613-9. doi:https://doi.org/10.1016/0895-4356(92)90133-8.
Chen MS, Jr., Lara PN, Dang JH, Paterniti DA, Kelly K. Twenty years post-NIH Revitalization Act: enhancing minority participation in clinical trials (EMPaCT): laying the groundwork for improving minority clinical trial accrual: renewing the case for enhancing minority participation in cancer clinical trials. Cancer. 2014;120 Suppl 7(0 7):1091-6. doi:https://doi.org/10.1002/cncr.28575.
Vose J. Minority enrollment to clinical trials: road to increased access. Oncology (Williston Park, NY). 2021;35(3):107. doi:https://doi.org/10.46883/onc.2021.3503.0107.
Hussain-Gambles M, Atkin K, Leese B. Why ethnic minority groups are under-represented in clinical trials: a review of the literature. Health Soc Care Community. 2004;12(5):382-8. doi:https://doi.org/10.1111/j.1365-2524.2004.00507.x.
van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians' perceptions of patients. Soc Sci Med (1982). 2000;50(6):813-28. doi:https://doi.org/10.1016/s0277-9536(99)00338-x.
Hughson JA, Woodward-Kron R, Parker A, et al. A review of approaches to improve participation of culturally and linguistically diverse populations in clinical trials. Trials. 2016;17(1):263. doi:https://doi.org/10.1186/s13063-016-1384-3.
Kronenfeld JP, Graves KD, Penedo FJ, Yanez B. Overcoming disparities in cancer: a need for meaningful reform for Hispanic and Latino cancer survivors. Oncologist. 2021;doi:https://doi.org/10.1002/onco.13729.
Evans KR, Lewis MJ, Hudson SV. The role of health literacy on African American and Hispanic/Latino perspectives on cancer clinical trials. J Cancer Educ. 2012;27(2):299-305. doi:https://doi.org/10.1007/s13187-011-0300-5.
Montalvo W, Larson E. Participant comprehension of research for which they volunteer: a systematic review. J Nurs Scholarsh. 2014;46(6):423-31. doi:https://doi.org/10.1111/jnu.12097.
Obeng-Gyasi S, Kircher SM, Lipking KP, et al. Oncology clinical trials and insurance coverage: an update in a tenuous insurance landscape. Cancer. 2019;125(20):3488-3493. doi:https://doi.org/10.1002/cncr.32360.
Hoos WA, James PM, Rahib L, Talley AW, Fleshman JM, Matrisian LM. Pancreatic cancer clinical trials and accrual in the United States. J Clin Oncol. 2013;31(27):3432-8. doi:https://doi.org/10.1200/jco.2013.49.4823.
Lara PN, Jr., Higdon R, Lim N, et al. Prospective evaluation of cancer clinical trial accrual patterns: identifying potential barriers to enrollment. J Clin Oncol. 2001;19(6):1728-33. doi:https://doi.org/10.1200/jco.2001.19.6.1728.
Backen A, Lamarca A, Hubner RA, McNamara MG, Valle JW. HPB cancers in older patients | inclusion of older/senior patients in clinical trials. Eur J Surg Oncol. 2021;47(3 Pt A):597-602. doi:https://doi.org/10.1016/j.ejso.2020.11.002.
Baimas-George M, Watson M, Thompson K, et al. Prehabilitation for Hepatopancreatobiliary surgical patients: interim analysis demonstrates a protective effect from neoadjuvant chemotherapy and improvement in the frailty phenotype. Am Surg. 2021;87(5):714-724. doi:https://doi.org/10.1177/0003134820952378.
Bongers BC, Dejong CHC, den Dulk M. Enhanced recovery after surgery programmes in older patients undergoing hepatopancreatobiliary surgery: what benefits might prehabilitation have? Eur J Surg Oncol. 2021;47(3 Pt A):551-559. doi:https://doi.org/10.1016/j.ejso.2020.03.211.
Chow CJ, Habermann EB, Abraham A, et al. Does enrollment in cancer trials improve survival? J Am Coll Surg. 2013;216(4):774-80; discussion 780-1. doi:https://doi.org/10.1016/j.jamcollsurg.2012.12.036.
Paez JG, Jänne PA, Lee JC, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science (New York, NY). 2004;304(5676):1497-500. doi:https://doi.org/10.1126/science.1099314.
Loree JM, Anand S, Dasari A, et al. Disparity of race reporting and representation in clinical trials leading to cancer drug approvals from 2008 to 2018. JAMA Oncol. 2019;5(10):e191870. doi:https://doi.org/10.1001/jamaoncol.2019.1870.
Unger JM, Hershman DL, Albain KS, et al. Patient income level and cancer clinical trial participation. J Clin Oncol. 2013;31(5):536-42. doi:https://doi.org/10.1200/jco.2012.45.4553.
Azap RA, Diaz A, Hyer JM, et al. Impact of race/ethnicity and county-level vulnerability on receipt of surgery among older medicare beneficiaries with the diagnosis of early pancreatic cancer. Ann Surg Oncol. 2021;doi:https://doi.org/10.1245/s10434-021-09911-1.
Nickell A, Stewart SL, Burke NJ, et al. Engaging limited English proficient and ethnically diverse low-income women in health research: a randomized trial of a patient navigator intervention. Patient Educ Couns. 2019;102(7):1313-1323. doi:https://doi.org/10.1016/j.pec.2019.02.013.
Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;22(6):882-7. doi:https://doi.org/10.1007/s11606-007-0160-1.
Paskett ED, Katz ML, DeGraffinreid CR, Tatum CM. Participation in cancer trials: recruitment of underserved populations. Clin Adv Hematol Oncol. 2003;1(10):607-13.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Eskander, M.F., Gil, L., Beal, E.W. et al. Access Denied: Inequities in Clinical Trial Enrollment for Pancreatic Cancer. Ann Surg Oncol 29, 1271–1277 (2022). https://doi.org/10.1245/s10434-021-10868-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10868-4