Abstract
Background
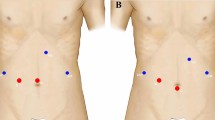
Minor liver resections of posterosuperior segments (1, 4A, 7, 8) are challenging to perform laparoscopically and are mainly performed using an open approach. We determined the feasibility of robotic resections of posterosuperior segments and compared short-term outcomes with the open approach.
Methods
Data on open and robotic minor (≤ 3 segments) liver resections including the posterosuperior segments, performed between 2009 and 2016, were collected retrospectively from four hospitals. Robotic and open liver resections were compared, before and after propensity score matching.
Results
In total, 51 robotic and 145 open resections were included. After matching, 31 robotic resections were compared with 31 open resections. Median hospital stay was 4 days (interquartile range [IQR] 3–7) for the robotic group, versus 8 days (IQR 6–10) for the open group (p < 0.001). Median operative time was 222 min (IQR 164–505) for robotic cases versus 231 min (IQR 190–301) for open cases (p = 0.668). Median estimated blood loss was 200 mL (IQR 100–400) versus 300 mL (IQR 125–750), respectively (p = 0.212). In the robotic group, one patient (3%) had a major complication, versus three patients (10%) in the open group (p = 0.612). Readmissions were similar—10% in the robotic group versus 6% in the open group (p > 0.99). There was no mortality in either group.
Conclusion
Minor robotic liver resections of the posterosuperior segments are safe and feasible and display a shorter length of stay than open resections in selected patients at expert centers.

Similar content being viewed by others
References
Jin S, Fu Q, Wuyun G, et al. Management of post-hepatectomy complications. World J Gastroenterol. 2013;19(44):7983–91.
Ciria R, Cherqui D, Geller DA, et al. Comparative Short-term Benefits of Laparoscopic Liver Resection: 9000 Cases and Climbing. Ann Surg. 2016; 263(4):761–77.
Fretland AA, Dagenborg VJ, Bjornelv GMW, et al. Laparoscopic versus open resection for colorectal liver metastases: the OSLO-COMET randomized controlled trial. Ann Surg. 2018; 267(2):199–207.
Buell JF, Cherqui D, Geller DA, et al. The international position on laparoscopic liver surgery: the Louisville statement, 2008. Ann Surg. 2009; 250(5):825–30.
Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015; 261(4):619–29.
Ishizawa T, Gumbs AA, Kokudo N, et al. Laparoscopic segmentectomy of the liver: from segment I to VIII. Ann Surg. 2012; 256(6):959–64.
Herman P, Krüger JAP, Perini MV, et al. Laparoscopic hepatic posterior sectionectomy: a hand-assisted approach. Ann Surg Oncol. 2013; 20(4):1266.
Ogiso S, Conrad C, Araki K, et al. Laparoscopic transabdominal with transdiaphragmatic access improves resection of difficult posterosuperior liver lesions. Ann Surg. 2015; 262(2):358–65.
Okuno M, Goumard C, Mizuno T, et al. Operative and short-term oncologic outcomes of laparoscopic versus open liver resection for colorectal liver metastases located in the posterosuperior liver: a propensity score matching analysis. Surg Endosc. 2018; 32(4):1776–86.
Nota C, Molenaar IQ, van Hillegersberg R, et al. Robotic liver resection including the posterosuperior segments: initial experience. J Surg Res. 2016; 206(1):133–8.
Leung U, Fong Y. Robotic liver surgery. Hepatobiliary Surg Nutr. 2014; 3(5):288–94.
Barbash GI, Glied SA. New technology and health care costs: the case of robot-assisted surgery. N Engl J Med. 2010; 363(8):701–4.
Melstrom LG, Warner SG, Woo Y, et al. Selecting incision-dominant cases for robotic liver resection: towards outpatient hepatectomy with rapid recovery. Hepatobiliary Surg Nutr. 2018;7(2):77–84.
Nota CL, Rinkes IHB, Molenaar IQ, et al. Robot-assisted laparoscopic liver resection: a systematic review and pooled analysis of minor and major hepatectomies. HPB (Oxford). 2016; 18(2):113–20.
von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014; 12(12):1495–9.
Reddy SK, Barbas AS, Turley RS, et al. A standard definition of major hepatectomy: resection of four or more liver segments. HPB (Oxford) 2011; 13(7):494–502.
Couinaud C. Liver lobes and segments: notes on the anatomical architecture and surgery of the liver. Presse Med. 1954; 62(33):709–12 (in French).
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240(2):205–13.
Garrido MM, Kelley AS, Paris J, et al. Methods for constructing and assessing propensity scores. Health Serv Res. 2014; 49(5):1701–20.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011; 46(3):399–424.
Cluver L, Boyes M, Orkin M, et al. Child-focused state cash transfers and adolescent risk of HIV infection in South Africa: a propensity-score-matched case-control study. Lancet Glob Health. 2013; 1(6):e362–70.
Cameron AC, Trivedi PK. Regression analysis of count data. Cambridge: Cambridge University Press; 1998.
Cho JY, Han HS, Yoon YS, et al. Feasibility of laparoscopic liver resection for tumors located in the posterosuperior segments of the liver, with a special reference to overcoming current limitations on tumor location. Surgery. 2008; 144(1):32–8.
Troisi RI, Montalti R, Van Limmen JG, et al. Risk factors and management of conversions to an open approach in laparoscopic liver resection: analysis of 265 consecutive cases. HPB (Oxford). 2014; 16(1):75–82.
Halls MC, Cipriani F, Berardi G, et al. Conversion for unfavorable intraoperative events results in significantly worst outcomes during laparoscopic liver resection: lessons learned from a multicenter review of 2861 cases. Ann Surg. 2017. https://doi.org/10.1097/SLA.0000000000002332.
Patriti A, Cipriani F, Ratti F, et al. Robot-assisted versus open liver resection in the right posterior section. JSLS. 2014; 18(3):e2014.00040. https://doi.org/10.4293/JSLS.2014.00040.
Peters B, Armijo P, Krause C, Choudhury S, Oleynikov D. Review of emerging surgical robotic technology. Surg Endosc. 2018;32:1636–55.
Acknowledgments
The authors thank F.J. Smits, MD, Department of Surgery, University Medical Center Utrecht, The Netherlands, and R. Nelson, Ph.D., Department of Information Sciences, City of Hope National Medical Center, Duarte, CA, USA, for support during statistical analyses. The authors thank I.M. Newman, Ph.D., Department of Surgery, City of Hope National Medical Center, Duarte, CA, USA, for scientific editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under award number P30CA033572. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest
Yanghee Woo is a consultant for Ethicon and Verb Surgical. Yuman Fong is a scientific consultant to Medtronics Inc. Carolijn L. Nota, Mustafa Raoof, Thomas Boerner, I. Quintus Molenaar, Gi Hong Choi, T. Peter Kingham, Karen Latorre, Inne H. M. Borel Rinkes and Jeroen Hagendoorn have declared no conflicts of interest.
Rights and permissions
About this article
Cite this article
Nota, C.L., Woo, Y., Raoof, M. et al. Robotic Versus Open Minor Liver Resections of the Posterosuperior Segments: A Multinational, Propensity Score-Matched Study. Ann Surg Oncol 26, 583–590 (2019). https://doi.org/10.1245/s10434-018-6928-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-6928-1