Abstract
Background
Multiple recent reports have documented significant variability of reoperation rates after initial lumpectomy for breast cancer. To address this issue, a multidisciplinary consensus conference was convened during the American Society of Breast Surgeons 2015 annual meeting.
Methods
The conference mission statement was to “reduce the national reoperation rate in patients undergoing breast conserving surgery for cancer, without increasing mastectomy rates or adversely affecting cosmetic outcome, thereby improving value of care.” The goal was to develop a toolbox of recommendations to reduce the variability of reoperation rates and improve cosmetic outcomes. Conference participants included providers from multiple disciplines involved with breast cancer care, as well as a patient representative. Updated systematic reviews of the literature and invited presentations were sent to participants in advance. After topic presentations, voting occurred for choice of tools, level of evidence, and strength of recommendation.
Results
The following tools were recommended with varied levels of evidence and strength of recommendation: compliance with the SSO-ASTRO Margin Guideline; needle biopsy for diagnosis before surgical excision of breast cancer; full-field digital diagnostic mammography with ultrasound as needed; use of oncoplastic techniques; image-guided lesion localization; specimen imaging for nonpalpable cancers; use of specialized techniques for intraoperative management, including excisional cavity shave biopsies and intraoperative pathology assessment; formal pre- and postoperative planning strategies; and patient-reported outcome measurement.
Conclusions
A practical approach to performance improvement was used by the American Society of Breast Surgeons to create a toolbox of options to reduce lumpectomy reoperations and improve cosmetic outcomes.
Similar content being viewed by others
A gap in quality of healthcare exists whenever variability of care coexists with evidence that high performance is achievable.1,2 Multiple, recent reports have documented significant variability of care for oncologic reoperation after initial lumpectomy for breast cancer.3–6 Rates of reoperation vary from less than 10 % to more than 50 %. This variability is not accounted for by patient or disease characteristics. Therefore, the American Society of Breast Surgeons (ASBrS) convened a multidisciplinary consensus conference entitled a “Collaborative Attempt to Lower Lumpectomy Reoperation rates” (CALLER).
The CALLER conference mission statement was defined as: “Reduce the national reoperation rate in patients undergoing breast-conserving surgery for cancer, without increasing mastectomy rates or adversely affecting cosmetic outcome, thereby improving value of care.”
The purpose of the consensus conference was to develop a practical toolbox of recommendations to help providers reduce lumpectomy reoperations to the best achievable level based on available evidence and expert opinion. The target goal is not zero, and to attempt this would be expected to impact cosmetic outcome and lower the breast-conserving therapy rate. The group identified and considered concurrent efforts to reduce reoperation variability, including the meta-analysis that resulted in the SSO-ASTRO margin statement and an updated systematic review of the literature performed by the American College of Surgeons for their new “Operative Standards for Cancer” manual.7–9
Methods
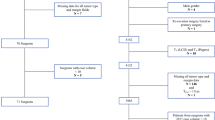
Consensus conference participants included experts in breast cancer care from multiple disciplines (surgery, radiology, pathology, plastic surgery, and radiation and medical oncology). A statistician and a patient representative with patient advocacy experience were included. Participants with expertise in quality measurement, patient-reported outcomes, guideline development, and clinical trials were present. There was diversity across breast surgeon practice type, including community and academic surgeons.
Toolbox development followed to the extent possible the standards of the Institute of Medicine for guideline development.10 Multiple recent systematic literature reviews were referenced by participants.7,9,11–21 Before the conference, all participants were provided with key topics, references, speaker presentations, and potential “tools” for the toolbox. After topic presentation, an interactive discussion occurred followed by voting. Conference participants and the ASBrS Board of Directors approved toolbox recommendations.
Results
The proposed conference tools, references, level of evidence, consensus, and strength of recommendation are described in Tables 1 and 2. Recognizing the impact of reoperations on patient care, cost, and outcomes, the conference participants had uniform agreement to set a 5-year target goal for a national average reoperation rate in the year 2020. However, there was lack of uniformity for the actual target number. Two-thirds (10/15) of participants recommended a goal of less than 20 %.
Tool 1: Preoperative Diagnostic Imaging Should Include Full-Field Digital Mammography and Supplementary Imaging to Include Ultrasound as Needed
All participants agreed that high-quality, meticulous, preoperative, diagnostic mammography was necessary preoperatively. “Selective” use of ipsilateral ultrasound (US) was recommended. US may be of less benefit when screening mammography identifies calcifications without mass. Despite near routine actual use of US by conference participants, they concluded that the level of evidence did not support a recommendation for “routine” US. Breast tomography was discussed and judged to have future applications but was not yet included in the toolbox due to insufficient evidence. Routine use of MRI was not recommended based on meta-analyses that show its use does not affect the rate of reexcision or local recurrence. Selective use of MRI is described in position statements from other groups.22–24
Tool 2: Minimally Invasive Breast Biopsy (MIBB) for Breast Cancer Diagnosis
Some studies demonstrate lower reoperation rates when a diagnosis of malignancy is known before surgical excision. MIBB provides opportunity for preoperative treatment planning to include genetic risk assessment, medical oncology, and plastic surgery consultation and axillary evaluation.
Tool 3: Multidisciplinary Discussions to Include Radiology, Pathology, Surgery, and Radiation and Medical Oncology
Optimizing reoperation rates requires preoperative collaboration between radiologists, surgeons, and pathologists. In patients considered for neoadjuvant therapy, medical oncology consultation also is necessary. Preoperative knowledge of number of lesions, geometry, distance to skin and chest wall, and possible extension towards the nipple may all facilitate negative margins. Information technology that enhances communication and provides intraoperative archived images can aid lesion review and communication. Postoperative discussion with all specialties aids decision making regarding reoperation.
Tool 4: For Nonpalpable Breast Lesions, the Use of Radioactive Seeds, Intraoperative US, or Wire Localization to Direct Lesion Excision is Recommended
A localization method should be used for resection of all nonpalpable cancers. Although some studies have indicated superiority of one technique compared with another, the conference concluded that evidence to recommend a single technique was not definitive. Surgeon use of US also can be used to aid targeting and decide volume of resection in both palpable and nonpalpable lesions. Placement of multiple localizing wires or seeds (bracketing) may be useful for larger lesions, multifocal tumors, or extensive ductal carcinoma in situ (DCIS).
Tool 5: Oncoplastic Techniques can Reduce the Need for Reoperation in Anatomically Suitable Patients
Oncoplastic techniques have the potential to decrease positive margins at initial lumpectomy by allowing resection of a larger volume of tissue. They also may improve ipsilateral breast appearance and contralateral breast symmetry. There was uniform agreement for their potential benefit. The conference recommends applying these techniques only in a selective group of patients. Small primary cancers can be excised with acceptable cosmetic results without oncoplastic techniques. For all procedures, marker clips or other marking modality should be considered for application to cavity side walls to aid radiation planning.
Tool 6: Specimen Orientation of 3 or More Margins
When the breast cancer is excised, markers or ink should be placed on the specimen for orientation to ensure which margin edge(s) is/are positive to guide focused reexcision of the correct tissue, if necessary. There are limited data linking orientation directly to reoperation rates, but the conference concluded the benefit/burden ratio of orientation was high. All excisions should be oriented. Orientation is associated with better cosmetic outcomes by avoiding “entire cavity” reexcision in patients with nonoriented positive margins. The consensus was that orientation of at least three sides was superior to two sides. Some participants favored intraoperative six-sided inking as best practice, but there was no consensus on orientation methodology beyond labeling at least three margins.
Tool 7: Specimen Radiograph with Surgeon Intraoperative Review
The primary role of specimen imaging is to document removal of the targeted nonpalpable lesion before the patient leaves the operating room. Lower-level evidence supports specimen radiography as a method to assess distance of lesion to margin and therefore direct and potentially reduce reoperation. Specimens should not undergo compression during imaging, because it may cause specimen fracture that allows ink to enter the crevasse and a false-positive margin. Some participants supplement specimen radiography with US. Surgeons should review the specimen imaging before the operation has been completed, ideally with surgeon-radiology communication. Real-time review may avoid a complete “miss” of the lesion or direct the surgeon to perform an additional cavity shave for a “close” margin. Specimen imaging may not be universally available. If not, the conference strongly encourages systems to develop necessary resources for specimen imaging with immediate image review. Two views at orthogonal angles may identify close or positive margins not seen on a single view. Intraoperative imaging with other modalities to include tomograms, MRI, CT, and other imaging are being investigated.
Tool 8: Consider Cavity Shave Margins in Patients with T2 or Greater Tumor Size or TI with Extensive Intraductal Carcinoma (EIC)
There are moderate levels of evidence that cavity side wall excisions correlate with lower reoperation rate. Shave size should provide adequate sampling of the residual wall. “Tiny shaves” representing only a small portion of a “wall” were discouraged. If shaves are performed, the “final” edge should be marked; i.e., nonoriented shave with even a small amount of tumor on the surface would constitute a final ink positive margin status requiring reexcision. Some surgeons routinely perform shaves of all cavity side walls regardless of tumor type or size. Others perform selective shaves directed by palpation, imaging, or pathologic specimen examination. There has been one recently published, randomized, controlled trial of cavity shave versus no-shave margins, which demonstrated a statistically significant decrease in the reoperation rate for patients undergoing breast conservation surgery.25
Tool 9: Intraoperative Pathology Assessment of Lumpectomy Margins may Help Decrease Reexcision When Feasible
A systematic literature review demonstrates that intraoperative margin assessment with frozen histologic section or imprint cytology are associated with lower reoperation rates by allowing intraoperative reexcision of positive margins.13 There is lower-level evidence to support only gross specimen examination. Resources and expertise may limit the feasibility of routine intraoperative pathology assessment. Several institutions report low reoperation rates without intraoperative margin assessment.
Tool 10: Compliance with the SSO-ASTRO Margin Guideline to Not Routinely Reoperate for Close Margins with no Tumor on Ink in Patients with Invasive Cancer
Compliance with this guideline has the potential to reduce reoperations by 40 %.6 The remaining tools are targeted towards reducing ink positive margins at the initial lumpectomy. By meta-analysis, recurrence risk doubles when ink positive margins are not excised. Recurrence is not improved by reoperation if the margin is negative. If ink positive margins occur, the need for reoperation should be evaluated by the treating team in collaboration with the patient (“shared decision making”), providing patients with recurrence risks in absolute percentages for the choices of reoperation or not. As a consequence, some patients may choose not to have reoperation. The margin guideline is applicable to subsets of patients with “bad tumor biology” (triple negative, Her 2 positive, high grade), young age, lobular cancer, EIC, or not receiving systemic treatment. There is no proven benefit for reoperation in these patients if they have ink negative margins. Some patients with negative margins may still be considered for reoperation, if clinical and/or imaging findings suggest residual persistent adjacent disease. The margin meta-analysis did not include patients with neoadjuvant therapy or pure DCIS. Given the lack of consensus regarding acceptable margin width for DCIS, decisions regarding reoperation in these patients optimally involves multidisciplinary input and shared decision making with the patient. Until new evidence is available for DCIS, the conference supports NCCN guidelines for reoperation if the margin is ink positive or <1 mm.26
Tool 11: Routine Breast-Specific Patient Reported Outcome (PRO) Measurement may Help to Assess Cosmetic Outcomes When Feasible
There is limited reporting in the literature of cosmetic and functional outcomes from the patient perspective. Validated PRO tools, such as BREAST-Q©, should be more widely adopted and may aid improvement. New tools need to be developed that decrease the burdens for both providers and patients for reporting.
Discussion
The goal of the consensus conference was to provide practitioners with a variety of tools that can be adapted to help lower rates of reoperation following lumpectomy. While these recommendations are not meant to serve as guidelines or standard of care, conference leaders complied with most principles for guideline development as defined by the IOM.10 Updated systematic reviews were referenced and the group included multiple disciplines and stakeholders.7,9,11–21 The group did not provide a period for public comment, request for other society endorsement, or commission new systematic literature reviews. For expediency, recommendations were provided that could be implemented into clinical practice quickly. “Standard of care” is a legal term, and our toolbox does not establish a new legal “standard of care.” It also is important to recognize that performing reoperation does not mean poor quality care. Particularly, omission of reoperation for positive margins is not recommended. Reoperation of a positive margin is good quality care and results in lower risk of cancer recurrence. All tools in the toolbox earned endorsement by a majority vote. It does not follow that all tools are recommended for every patient.
At least three factors should be considered for selection. The first is resource availability. For example, one tool is the use of intraoperative frozen section (FS) for margin assessment, a tool associated with very low rates of reoperation.27 This service may not be available in all settings, and there should be no inference of “poor quality” for lack of access to it. In contrast, multidisciplinary preoperative planning—in person or virtual—can be implemented widely.
The second consideration for tool selection is baseline reoperation rate. The average reoperation rate in four national databases ranges from 20 to 24 %.3–6 For surgeons and institutions with average or higher rates, a trial of previously unused or underutilized tools should be considered, followed by tracking of outcomes. For those with rates already in the best tiers of performance, there can be attempts to improve even further by testing different or additional tools, but performance tracking will still be necessary.
The last consideration for number of tools is “redundancy.” For example, if circumferential lumpectomy FS is used and negative, then the benefit of additional shaving of cavity side walls is low. If complete cavity side wall shavings are performed, then the benefit of lumpectomy margin FS is low too. Some participants recommended using more tools when operating on patients with known factors associated with positive margins, such as larger size, invasive lobular type, low-grade noncalcified DCIS, and EIC status. All tools in the toolbox can be applied for patients with DCIS and invasive cancer except the SSO-ASTRO margin statement, which was specific for invasive cancer and did not include patients with pure DCIS.
Intraoperative devices to assess margin status were discussed as potential tools to decrease reoperation. A recent, randomized trial concluded that the MarginProbe™ device was associated with fewer reoperations.28 The conference majority vote was to omit these devices from the toolbox until further investigation.28–36
Measurement of both individual surgeon and institutional outcomes are essential prerequisites during attempts to reduce reoperation after initial lumpectomy. Measurement assesses the impact of these initiatives. If resources are available, a comprehensive audit that tracks intended and unintended outcomes is recommended (Table 3). If resources are limited, then minimal tracking would include reoperation, positive margin, and breast-conserving therapy (BCT) rates. Reoperation rates and BCT rates can be reported in the ASBrS Mastery database, the National Consortium of Breast Centers Quality Measurement Program, and “in-house” registries.37,38 All breast cancer quality-measurement programs were recently summarized.39
Increased mastectomy rates and poor cosmetic outcomes are potential unintended adverse outcomes of efforts to lower reoperation rates and therefore should be monitored.40–42 These risks were recognized but were felt to be balanced by the potential to improve overall patient care by following conference recommendations. There is evidence that both reoperation rate and cosmetic outcome can improve by adoption of oncoplastic techniques.43–48
The conference process and work product is not without limitations. We did not follow strict guideline development standards and did not use a formal Delphi process in arriving at consensus. Furthermore, most of the tools are not based on high-level evidence. The strength of the conference is its recognition that unacceptable variability occurs in the care of patients undergoing lumpectomy. As a consequence, multiple stakeholders accepted ownership and then developed recommendations to improve care, cost, and outcomes by using “best available” evidence and expert opinion.
Conclusions
Recognition of the gap between actual and achievable care led to development of a toolbox of recommendations to reduce the proven variability of reoperation and the suspected variability of cosmetic outcome after initial lumpectomy for breast cancer. A list of other ASBrS initiatives to reduce reoperation and improve cosmesis is described in Table 4. Tracking of outcomes is recommended for all initiatives. Next steps include: (1) dissemination and implementation strategies; (2) comparative effectiveness research to determine which tools or collection of tools are most strongly associated with reoperation rates, cosmetic outcome, and value; and (3) collaboration with industry, payer, and government stakeholders to provide better support for performance reporting that is funded, incentivized, and less burdensome for providers.
References
National Quality Forum: Measure evaluation criteria. http://www.qualityforum.org/docs/measure_evaluation_criteria.aspx#importance. Accessed 20 May 2015.
Hassett MJ, Hughes ME, Niland JC, et al. Selecting high priority quality measures for breast cancer quality improvement. Med Care. 2008;46:762–70.
McCahill LE, Single RM, Aiello Bowles EJ, et al. Variability in reexcision following breast conservation surgery. JAMA. 2012;307:467–75.
Wilke LG, Czechura T, Wang C, Lapin B, Liederbach E, Winchester DP, Yao K. Repeat surgery after breast conservation for the treatment of stage 0 to II breast carcinoma: a report from the National Cancer Data Base, 2004-2010. JAMA Surg. 2014;149:1296–305.
Jeevan R, Cromwell DA, Trivella M, et al. Reoperation rates after breast conserving surgery for breast cancer among women in England: retrospective study of hospital episode statistics. BMJ. 2012;345:e4505.
Landercasper J, Whitacre E, Degnim AC, Al-Hamadani M. Reasons for re-excision after lumpectomy for breast cancer: insight from the American Society of Breast Surgeons Mastery(SM) database. Ann Surg Oncol. 2014;21:3185–91.
Houssami N, Macaskill P, Marinovich ML, Morrow M. The association of surgical margins and local recurrence in women with early-stage invasive breast cancer treated with breast-conserving therapy: a meta-analysis. Ann Surg Oncol. 2014;21:717–30.
Moran MS, Schnitt SJ, Giuliano AE, et al. Society of Surgical Oncology-American Society for Radiation Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. Ann Surg Oncol. 2014;21:704–16.
American College of Surgeons Clinical Research Program, Alliance for Clinical Trials in Oncology, Nelson HD, Hunt KK. Partial mastectomy. In: Blair S, El Tamer M, Khan S, et al. (eds). Operative standards cancer surg. Vol. 1. Wolters Kluwer Health, Philadelphia, 2015.
Graham R, Mancher M, Wolman DM, et al. Clinical practice guidelines we can trust. National Academies of Press, Washington, DC, 2011. https://www.iom.edu/~/media/Files/Report%20Files/2011/Clinical-Practice-Guidelines-We-Can-Trust/Clinical%20Practice%20Guidelines%202011%20Insert.pdf. Accessed 20 May 2015.
Houssami N, Turner R, Morrow M. Preoperative magnetic resonance imaging in breast cancer: meta-analysis of surgical outcomes. Ann Surg. 2013;257:249–55.
Dahabreh IJ, Wieland LS, Adam GP, Halladay C, Lau J, Trikalinos TA. Core needle and open surgical biopsy for diagnosis of breast lesions: an update to the 2009 report [Internet]. Comparative effectiveness reviews. Agency for Healthcare Research and Quality, Rockville, MD, 2014, p. 139. http://www.ncbi.nlm.nih.gov/books/NBK246878/. Accessed 21 May 2015.
Esbona K, Li Z, Wilke LG. Intraoperative imprint cytology and frozen section pathology for margin assessment in breast conservation surgery: a systematic review. Ann Surg Oncol. 2012;19:3236–45.
Coates AS, Winer EP, Goldhirsch A, et al. Tailoring therapies—improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann Oncol. 2015;26(8):1533–46. doi:10.1093/annouc/mdv221.
Bruening W, Schoelles K, Treadwell J, Launders J, Fontanarosa J, Tipton K. Comparative effectiveness of core-needle and open surgical biopsy for the diagnosis of breast lesions [internet]. Comparative effectiveness reviews. Agency for Healthcare Research and Quality, Rockville, MD, 2009, p. 19. http://www.ncbi.nlm.nih.gov/books/NBK45220/. Accessed 21 May 2015.
Fancellu A, Turner RM, Dixon JM, Pinna A, Cottu P, Houssami N. Meta-analysis of the effect of preoperative breast MRI on the surgical management of ductal carcinoma in situ. Br J Surg. 2015;102(8):883–93. doi:10.1002/bjs.9797.
Losken A, Dugal CS, Styblo TM, Carlson GW. A meta-analysis comparing breast conservation therapy alone to the oncoplastic technique. Ann Plast Surg. 2014;72:145–9.
Pouw B, de Wit-van der Veen LJ, Stokkel MP, Loo CE, Vrancken Peeters MJ, Valdes Olmos RA. Heading toward radioactive seed localization in non-palpable breast cancer surgery? A meta-analysis. J Surg Oncol. 2015;111:185–91.
Ahmed M, Douek M. Radioactive seed localisation (RSL) in the treatment of non-palpable breast cancers: systematic review and meta-analysis. Breast. 2013;22:383–8.
Ahmed M, van Hemelrijck M, Douek M. Systematic review of radioguided vs wire localization in the treatment of non-palpable breast cancers. Breast Cancer Res Treat. 2013;140:214–52.
Butler-Henderson K, Lee AH, Price RI, Waring K. Intraoperative assessment of margins in breast conserving therapy: a systematic review. Breast. 2014;23:112–9.
American Society of Breast Surgeons Consensus Statements. Use of magnetic resonance imaging in breast oncology. https://www.breastsurgeons.org/statements/index.php. Accessed 20 May 2015.
National Comprehensive Cancer Network. 2015 NCCN guidelines for breast cancer. Use of breast MRI in patients with breast cancer. https://www.nccn.org/store/login/login.aspx?, http://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed 20 May 2015.
American College of Radiology. ACR practice parameter for the performance of contrast-enhanced magnetic resonance imaging (MRI) of the breast. http://www.acr.org/quality-safety/standards-guidelines/practice-guidelines-by-modality/breast-imaging. Accessed 20 May 2015.
Chagpar AB, Killelea BK, Tsangaris TN, et al. A randomized, controlled trial of cavity shave margins in breast cancer. N Engl J Med. 2015.
National Comprehensive Cancer Network. 2015 NCCN guidelines for breast cancer. Margin status in DCIS. https://www.nccn.org/store/login/login.aspx?, http://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed 15 May 2015.
Boughey JC, Hieken TJ, Jakub JW, et al. Impact of analysis of frozen-section margin on reoperation rates in women undergoing lumpectomy for breast cancer: evaluation of the National Surgical Quality Improvement Program data. Surgery. 2014;156:190–7.
Schnabel F, Boolbol SK, Gittleman M, et al. A randomized prospective study of lumpectomy margin assessment with use of MarginProbe in patients with nonpalpable breast malignancies. Ann Surg Oncol. 2014;21:1589–95.
Sebastian M, Akbari S, Anglin B, Lin EH, Police AM. The impact of use of an intraoperative margin assessment device on re-excision rates. SpringerPlus. 2015;4:198.
Tummers QR, Verbeek FP, Schaafsma BE, et al. Real-time intraoperative detection of breast cancer using near-infrared fluorescence imaging and Methylene Blue. Eur J Surg Oncol. 2014;40:850–8.
Keller MD, Majumder SK, Kelley MC, et al. Autofluorescence and diffuse reflectance spectroscopy and spectral imaging for breast surgical margin analysis. Lasers Surg Med. 2010;42:15–23.
Keller MD, Vargis E, de Matos Granja N, et al. Development of a spatially offset Raman spectroscopy probe for breast tumor surgical margin evaluation. J Biomed Opt. 2011;16:077006.
Martin DT, Sandoval S, Ta CN, et al. Quantitative automated image analysis system with automated debris filtering for the detection of breast carcinoma cells. Acta Cytol. 2011;55:271–80.
Nguyen FT, Zysk AM, Chaney EJ, et al. Intraoperative evaluation of breast tumor margins with optical coherence tomography. Cancer Res. 2009;69:8790–6.
Allweis TM, Kaufman Z, Lelcuk S, et al. A prospective, randomized, controlled, multicenter study of a real-time, intraoperative probe for positive margin detection in breast-conserving surgery. Am J Surg. 2008;196:483–9.
Karni T, Pappo I, Sandbank J, et al. A device for real-time, intraoperative margin assessment in breast-conservation surgery. Am J Surg. 2007;194:467–73.
The American Society of Breast Surgeons. Mastery program. https://www.breastsurgeons.org/new_layout/programs/mastery/. Accessed 20 May 2015.
National Quality Measures for Breast Centers. http://www2.nqmbc.org/about-us/. Accessed 20 May 2015.
Edge SB. Quality measurement in breast cancer. J Surg Oncol. 2014;110:509–17.
Morrow M, Harris JR, Schnitt SJ. Surgical margins in lumpectomy for breast cancer. N Engl J Med. 2012;367:1269–70.
Morrow M, Katz SJ. The challenge of developing quality measures for breast cancer surgery. JAMA. 2012;307:509–10.
Schwartz T, Degnim AC, Landercasper J. Should re-excision lumpectomy rates be a quality measure in breast-conserving surgery? Ann Surg Oncol. 2013;20:3180–3.
Mook J, Klein R, Kobbermann A, et al. Volume of excision and cosmesis with routine cavity shave margins technique. Ann Surg Oncol. 2012;19:886–91.
Silverstein MJ, Savalia N, Khan S, Ryan J. Extreme oncoplasty: breast conservation for patients who need mastectomy. Breast J. 2015;21:52–9.
Silverstein MJ, Mai T, Savalia N, Vaince F, Guerra L. Oncoplastic breast conservation surgery: the new paradigm. J Surg Oncol. 2014;110:82–9.
Clough KB, Benyahi D, Nos C, Charles C, Sarfati I. Oncoplastic surgery: pushing the limits of breast-conserving surgery. Breast J. 2015;21:140–6.
Rezai M, Knispel S, Kellersmann S, Lax H, Kimmig R, Kern P. Systematization of oncoplastic surgery: selection of surgical techniques and patient-reported outcome in a cohort of 1035 patients. Ann Surg Oncol. 2015. doi:10.1245/s10434-015-4396-4.
Losken A, Pinell-White X, Hart AM, Freitas AM, Carlson GW, Styblo TM. The oncoplastic reduction approach to breast conservation therapy: benefits for margin control. Aesthet Surg J. 2014;34:1185–91.
Silverstein MJ, Lagios MD, Recht A, et al. International consensus conference II. J Am Coll Surg. 2005;201:586–97.
Silverstein MJ, Recht A., Lagios MD, et al. Consensus conference III. Image-detected breast cancer: state-of-the-art diagnosis and treatment. J Am Coll Surg. 2009;209:504–20.
American College of Radiology. Appropriateness criteria for palpable breast masses. https://acsearch.acr.org/list. Accessed 20 May 2015.
American College of Radiology. Appropriateness criteria for Stage I breast cancer: initial workup and surveillance for local recurrence and distant metastases in asymptomatic women. https://acsearch.acr.org/list. Accessed 20 May 2015.
Fisher CS, Mushawah FA, Cyr AE, Gao F, Margenthaler JA. Ultrasound-guided lumpectomy for palpable breast cancers. Ann Surg Oncol. 2011;18:3198–203.
Davis KM, Hsu CH, Bouton ME, Wilhelmson KL, Komenaka IK. Intraoperative ultrasound can decrease the re-excision lumpectomy rate in patients with palpable breast cancers. Am Surg. 2011;77:720–5.
Pezner RD, Tan MC, Clancy SL, Chen YJ, Joseph T, Vora NL. Radiation therapy for breast cancer patients who undergo oncoplastic surgery: localization of the tumor bed for the local boost. Am J Clin Oncol. 2013;36:535–9.
Down SK, Jha PK, Burger A, Hussien MI. Oncological advantages of oncoplastic breast-conserving surgery in treatment of early breast cancer. Breast J. 2013;19:56–63.
Rahusen FD, Bremers AJ, Fabry HF, van Amerongen AH, Boom RP, Meijer S. Ultrasound-guided lumpectomy of nonpalpable breast cancer versus wire-guided resection: a randomized clinical trial. Ann Surg Oncol. 2002;9:994–8.
Krekel NM, Haloua MH, Lopes Cardozo AM, et al. Intraoperative ultrasound guidance for palpable breast cancer excision (COBALT trial): a multicentre, randomised controlled trial. Lancet Oncol. 2013;14:48–54.
Moore MM, Whitney LA, Cerilli L, Imbrie JZ, Bunch M, Simpson VB, Hanks JB. Intraoperative ultrasound is associated with clear lumpectomy margins for palpable infiltrating ductal breast cancer. Ann Surg. 2001;233:761–8.
Ahmed M, Douek M. Intra-operative ultrasound vs wire localization in the surgical management of non-palpable breast cancer: a systemic review and meta-analysis. Breast Cancer Res Treat. 2014;140:435–46.
Gray RJ, Salud C, Nguyen K, et al. Randomized prospective evaluation of a novel technique for biopsy or lumpectomy of nonpalpable breast lesions: radioactive seed versus wire localization. Ann Surg Oncol. 2001;8:711–5.
Lovrics PJ, Goldsmith CH, Hodgson N, et al. A multicentered, randomized, controlled trial comparing radioguided seed localization to standard wire localization for nonpalpable, invasive and in situ breast carcinomas. Ann Surg Oncol. 2011;18:3407–14.
Murphy JO, Moo TA, King TA, et al. Radioactive seed localization compared to wire localization in breast-conserving surgery: initial 6-month experience. Ann Surg Oncol. 2013;20:4121–7.
Postma EL, Koffijberg H, Verkooijen HM, Witkamp AJ, van den Bosch MA, van Hillegersberg R. Cost-effectiveness of radioguided occult lesion localization (ROLL) versus wire-guided localization (WGL) in breast conserving surgery for nonpalpable breast cancer: results from a randomized controlled multicenter trial. Ann Surg Oncol. 2013;20:2219–26.
Medina-Franco H, Abarca-Perez L, Garcia-Alvarez MN, Ulloa-Gomez JL, Romero-Trejo C, Sepulveda-Mendez J. Radioguided occult lesion localization (ROLL) versus wire-guided lumpectomy for non-palpable breast lesions: a randomized prospective evaluation. J Surg Oncol. 2008;97:108–11.
Sajid MS, Parampalli U, Haider Z, Bonomi R. Comparison of radioguided occult lesion localization (ROLL) and wire localization for non-palpable breast cancers: a meta-analysis. J Surg Oncol. 2012;105:852–8.
Landheer ML, Veltman J, van Eekeren R, Zeillemaker AM, Boetes C, Wobbes T. MRI-guided preoperative wire localization of nonpalpable breast lesions. Clin Imaging. 2006;30:229–33.
van der Ploeg IM, Hobbelink M, van den Bosch MA, Mali WP, Borel Rinkes IH, van Hillegersberg R. Radioguided occult lesion localisation’ (ROLL) for non-palpable breast lesions: a review of the relevant literature. Eur J Surg Oncol. 2008;34:1–5.
Barentsz MW, van Dalen T, Gobardhan PD, et al. Intraoperative ultrasound guidance for excision of non-palpable invasive breast cancer: a hospital-based series and an overview of the literature. Breast Cancer Res Treat. 2012;135:209–19.
Fortunato L, Penteriani R, Farina M, Vitelli CE, Piro FR. Intraoperative ultrasound is an effective and preferable technique to localize non-palpable breast tumors. Eur J Surg Oncol. 2008;34:1289–92.
Lovrics PJ, Cornacchi SD, Vora R, Goldsmith CH, Kahnamoui K. Systematic review of radioguided surgery for non-palpable breast cancer. Eur J Surg Oncol. 2011;37:388–97.
Olsha O, Shemesh D, Carmon M, et al. Resection margins in ultrasound-guided breast-conserving surgery. Ann Surg Oncol. 2011;18:447–52.
Cox CE, Furman B, Stowell N, et al. Radioactive seed localization breast biopsy and lumpectomy: can specimen radiographs be eliminated? Ann Surg Oncol. 2003;10:1039–47.
Jakub JW, Gray RJ, Degnim AC, Boughey JC, Gardner M, Cox CE. Current status of radioactive seed for localization of non palpable breast lesions. Am J Surg. 2010;199:522–8.
Fine RE, Schwalke MA, Pellicane JV, Attai DJ. A novel ultrasound-guided electrosurgical loop device for intra-operative excision of breast lesions; an improvement in surgical technique. Am J Surg. 2009;198:283–6.
Eichler C, Hubbel A, Zarghooni V, Thomas A, Gluz O, Stoff-Khalili M, Warm M. Intraoperative ultrasound: improved resection rates in breast-conserving surgery. Anticancer Res. 2012;32:1051–6.
Barentsz MW, van den Bosch MA, Veldhuis WB, et al. Radioactive seed localization for non-palpable breast cancer. Br J Surg. 2013;100:582–8.
Gobardhan PD, de Wall LL, van der Laan L, et al. The role of radioactive iodine-125 seed localization in breast-conserving therapy following neoadjuvant chemotherapy. Ann Oncol. 2013;24:668–73.
Hughes JH, Mason MC, Gray RJ, et al. A multi-site validation trial of radioactive seed localization as an alternative to wire localization. Breast J. 2008;14:153–7.
Donker M, Drukker CA, Valdes Olmos RA, et al. Guiding breast-conserving surgery in patients after neoadjuvant systemic therapy for breast cancer: a comparison of radioactive seed localization with the ROLL technique. Ann Surg Oncol. 2013;20:2569–75.
Belloni E, Canevari C, Panizza P, et al. Nonpalpable breast lesions: preoperative radiological guidance in radioguided occult lesion localisation (ROLL). Radiol Med. 2011;116:564–74.
Duarte GM, Cabello C, Torresan RZ, et al. Radioguided intraoperative margins evaluation (RIME): preliminary results of a new technique to aid breast cancer resection. Eur J Surg Oncol. 2007;33:1150–7.
Lavoue V, Nos C, Clough KB, et al. Simplified technique of radioguided occult lesion localization (ROLL) plus sentinel lymph node biopsy (SNOLL) in breast carcinoma. Ann Surg Oncol. 2008;15:2556–61.
Nadeem R, Chagla LS, Harris O, Desmond S, Thind R, Titterrell C, Audisio RA. Occult breast lesions: a comparison between radioguided occult lesion localisation (ROLL) vs. wire-guided lumpectomy (WGL). Breast. 2005;14:283–9.
Kaufman CS, Jacobson L, Bachman B, Kaufman LB. Intraoperative ultrasonography guidance is accurate and efficient according to results in 100 breast cancer patients. Am J Surg. 2003;186:378–82.
Kaufman CS, Jacobson L, Bachman B, Kaufman L. Intraoperative ultrasound facilitates surgery for early breast cancer. Ann Surg Oncol. 2002;9:988–93.
Molina MA, Snell S, Franceschi D, et al. Breast specimen orientation. Ann Surg Oncol. 2009;16:285–8.
Singh M, Singh G, Hogan KT, Atkins KA, Schroen AT. The effect of intraoperative specimen inking on lumpectomy re-excision rates. World J Surg Oncol. 2010;8:4. doi:10.1186/1477-7819-8-4.
Moo TA, Choi L, Culpepper C, et al. Impact of margin assessment method on positive margin rate and total volume excised. Ann Surg Oncol. 2014;21:86–92.
Hequet D, Bricou A, Koual M, et al. Systematic cavity shaving: modifications of breast cancer management and long-term local recurrence, a multicentre study. Eur J Surg Oncol. 2013;39:899–905.
Camp ER, McAuliffe PF, Gilroy JS, Morris CG, Lind DS, Mendenhall NP, Copeland EM III. Minimizing local recurrence after breast conserving therapy using intraoperative shaved margins to determine pathologic tumor clearance. J Am Coll Surg. 2005;201:855–61.
Janes SE, Stankhe M, Singh S, Isgar B. Systematic cavity shaves reduces close margins and re-excision rates in breast conserving surgery. Breast. 2006;15:326–30.
Hewes JC, Imkampe A, Haji A, Bates T. Importance of routine cavity sampling in breast conservation surgery. Br J Surg. 2009;96:47–53.
Keskek M, Kothari M, Ardehali B, Betambeau N, Nasiri N, Gui GP. Factors predisposing to cavity margin positivity following conservation surgery for breast cancer. Eur J Surg Oncol. 2004;30:1058–64.
Kobbermann A, Unzeitig A, Xie XJ, et al. Impact of routine cavity shave margins on breast cancer re-excision rates. Ann Surg Oncol. 2011;18:1349–55.
Malik HZ, George WD, Mallon EA, Harnett AN, Macmillan RD, Purushotham AD. Margin assessment by cavity shaving after breast-conserving surgery: analysis and follow-up of 543 patients. Eur J Surg Oncol. 1999;25:464–9.
Rizzo M, Iyengar R, Gabram SG, Park J, Birdsong G, Chandler KL, Mosunjac MB. The effects of additional tumor cavity sampling at the time of breast-conserving surgery on final margin status, volume of resection, and pathologist workload. Ann Surg Oncol. 2010;17:228–34.
Britton PD, Sonoda LI, Yamamoto AK, Koo B, Soh E, Goud A. Breast surgical specimen radiographs: how reliable are they? Eur J Radiol. 2011;79:245–9.
Bathla L, Harris A, Davey M, Sharma P, Silva E. High resolution intra-operative two-dimensional specimen mammography and its impact on second operation for re-excision of positive margins at final pathology after breast conservation surgery. Am J Surg. 2011;202:387–94.
Ciccarelli G, Di Virgilio MR, Menna S, et al. Radiography of the surgical specimen in early stage breast lesions: diagnostic reliability in the analysis of the resection margins. Radiol Med. 2007;112:366–76.
Kim SH, Cornacchi SD, Heller B, Farrokhyar F, Babra M, Lovrics PJ. An evaluation of intraoperative digital specimen mammography versus conventional specimen radiography for the excision of nonpalpable breast lesions. Am J Surg. 2013;205:703–10.
Layfield DM, May DJ, Cutress RI, Richardson C, Agrawal A, Wise M, Yiangou C. The effect of introducing an in-theatre intra-operative specimen radiography (IOSR) system on the management of palpable breast cancer within a single unit. Breast. 2012;21:459–63.
McCormick JT, Keleher AJ, Tikhomirov VB, Budway RJ, Caushaj PF. Analysis of the use of specimen mammography in breast conservation therapy. Am J Surg. 2004;188:433–6.
Carmichael AR, Ninkovic G, Boparai R. The impact of intra-operative specimen radiographs on specimen weights for wide local excision of breast cancer. Breast. 2004;13:325–8.
Kaufman CS, Jacobson L, Bachman BA, et al. Intraoperative digital specimen mammography: rapid, accurate results expedite surgery. Ann Surg Oncol. 2007;14:1478–85.
Kaufman CS, Bachman BA, Jacobson L, Kaufman LB, Mahon C, Gambrell L. Intraoperative digital specimen mammography: prompt image review speeds surgery. Am J Surg. 2006;192:513–5.
Jorns JM, Visscher D, Sabel M, et al. Intraoperative frozen section analysis of margins in breast conserving surgery significantly decreases reoperative rates: one-year experience at an ambulatory surgical center. Am J Clin Pathol. 2012;138:657–69.
Olson TP, Harter J, Munoz A, Mahvi DM, Breslin T. Frozen section analysis for intraoperative margin assessment during breast-conserving surgery results in low rates of re-excision and local recurrence. Ann Surg Oncol. 2007;14:2953–60.
Osborn JB, Keeney GL, Jakub JW, Degnim AC, Boughey JC. Cost-effectiveness analysis of routine frozen-section analysis of breast margins compared with reoperation for positive margins. Ann Surg Oncol. 2011;18:3204–9.
Sable MS, Jorns JM, Wu A, Myers J, Newman LA, Breslin T. Development of an intraoperative pathology consultation service at a free-standing ambulatory surgical center: clinical and economic impact for patients undergoing breast cancer surgery. Am J Surg. 2012;204:66–77.
Cox CE, Pendas S, Ku NN, Reintgen DS, Greenberg HS, Nicosia SV. Local recurrence of breast cancer after cytological evaluation of lumpectomy margins. Am Surg. 1998;64:533–7; discussion 537–8.
D’Halluin F, Tas P, Rouquette S, et al. Intra-operative touch preparation cytology following lumpectomy for breast cancer: a series of 400 procedures. Breast. 2009;18:248–53.
Weinberg E, Cox C, Dupont E, et al. Local recurrence in lumpectomy patients after imprint cytology margin evaluation. Am J Surg. 2004;188:349–54.
Caruso F, Ferrara M, Castiglione G, et al. Therapeutic mammaplasties: full local control of breast cancer in one surgical stage with frozen section. Eur J Surg Oncol. 2011;37:871–5.
Cendan JC, Coco D, Copeland EM III. Accuracy of intraoperative frozen-section analysis of breast cancer lumpectomy-bed margins. J Am Coll Surg. 2005;201:194–8.
Chen K, Zeng Y, Jia H, et al. Clinical outcomes of breast-conserving surgery in patients using a modified method for cavity margin assessment. Ann Surg Oncol. 2012;19:3386–94.
Noguchi M, Minami M, Earashi M, Taniya T, Miyazaki I, Mizukami Y, Nonomura A. Intraoperative histologic assessment of surgical margins and lymph node metastasis in breast-conserving surgery. J Surg Oncol. 1995;60:185–90.
Riedl O, Fitzal F, Mader N, et al. Intraoperative frozen section analysis for breast-conserving therapy in 1016 patients with breast cancer. Eur J Surg Oncol. 2009;35:264–70.
Weber S, Storm FK, Stitt J, Mahvi DM. The role of frozen section analysis of margins during breast conservation surgery. Cancer J Sci Am. 1997;3:273–7.
Cox CE, Hyacinthe M, Gonzalez RJ, et al. Cytologic evaluation of lumpectomy margins in patients with ductal carcinoma in situ: clinical outcome. Ann Surg Oncol. 1997;4:644–9.
Creager AJ, Shaw JA, Young PR, Geisinger KR. Intraoperative evaluation of lumpectomy margins by imprint cytology with histologic correlation: a community hospital experience. Arch Pathol Lab Med. 2002;126:846–8.
Mannell A. Breast-conserving therapy in breast cancer patients: a 12-year experience. S Afr J Surg. 2005;43:28–30; discussion 30, 32.
Valdes EK, Boolbol SK, Cohen JM, Feldman SM. Intra-operative touch preparation cytology; does it have a role in re-excision lumpectomy? Ann Surg Oncol. 2007;14:1045–50.
Fukamachi K, Ishida T, Usami S, Takeda M, Watanabe M, Sasano H, Ohuchi N. Total-circumference intraoperative frozen section analysis reduces margin-positive rate in breast-conservation surgery. Jpn J Clin Oncol. 2010;40:513–20.
Landercasper J, Linebarger JH. Contemporary breast imaging and concordance assessment: a surgical perspective. Surg Clin North Am. 2011;91:33–58.
Kaufman CS. Breast care is a team sport. Breast J. 2004;10:469–72.
Jagsi R, Li Y, Morrow M, et al. Patient-reported quality of life and satisfaction with cosmetic outcomes after breast conservation and mastectomy with and without reconstruction: results of a survey of breast cancer survivors. Ann Surg. 2015;213(6):1198–206.
Atisha DM, Rushing CN, Samsa GP, et al. A national snapshot of satisfaction with breast cancer procedures. Ann Surg Oncol. 2015;22:361–9.
Waljee JF, Rogers MA, Alderman AK. Decision aids and breast cancer: do they influence choice for surgery and knowledge of treatment options? J Clin Oncol. 2007;25:1067–73.
Waljee JF, Hu ES, Newman LA, Alderman AK. Correlates of patient satisfaction and provider trust after breast-conserving surgery. Cancer. 2008;112:1679–87.
van der Steeg AF, De Vries J, Roukema JA. The value of quality of life and health status measurements in the evaluation of the well-being of breast cancer survivors. Eur J Surg Oncol. 2008;34:1225–30.
Sackey H, Sandelin K, Frisell J, Wickman M, Brandberg Y. Ductal carcinoma in situ of the breast. Long-term follow-up of health-related quality of life, emotional reactions and body image. Eur J Surg Oncol. 2010;36:756–62.
De Gournay E, Bonnetain F, Tixier H, Loustalot C, Dabakuyo S, Cuisenier J. Evaluation of quality of life after breast reconstruction using an autologous latissimus dorsi myocutaneous flap. Eur J Surg Oncol. 2010;36:520–7.
Waljee JF, Hawley S, Alderman AK, Morrow M, Katz SJ. Patient satisfaction with treatment of breast cancer: does surgeon specialization matter? J Clin Oncol. 2007;25:3694–8.
Chen CM, Cano SJ, Klassen AF, et al. Measuring quality of life in oncologic breast surgery: a systematic review of patient-reported outcome measures. Breast J. 2010;16:587–97.
Acknowledgments
The authors thank Sharon Grutman for conference planning; Choua Vang for assistance in manuscript preparation; Sarah Blair for assistance with bibliography; Gundersen Medical Foundation for unrestricted dollars to support the conference; and Dune Medical Devices for unrestricted dollars to support the conference
Conflict of Interest Statement
Unrestricted funds from Dune Medical Devices but no industry representative at CALLER conference and all participants and authors disclose no financial relationship with Dune Medical Devices.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Landercasper, J., Attai, D., Atisha, D. et al. Toolbox to Reduce Lumpectomy Reoperations and Improve Cosmetic Outcome in Breast Cancer Patients: The American Society of Breast Surgeons Consensus Conference. Ann Surg Oncol 22, 3174–3183 (2015). https://doi.org/10.1245/s10434-015-4759-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4759-x