Abstract
Background
The prognostic factors for patients with colorectal cancer liver metastasis (L-Mets) have not been fully described.
Methods
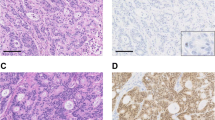
Resected specimens were obtained surgically from 1998 to 2008 at our university hospital. We investigated whether the status of two primary lesion cancer stem biomarkers, CD44 and CD133, were maintained in L-Mets and whether these markers were L-Mets prognostic factors. To investigate the CD133 and CD44 status, proliferation, invasiveness, and chemoresistance were examined immunohistochemically by using MIB-1, E-cadherin, and ABC-G2.
Results
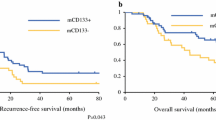
The CD44-positive rate in primary lesions and L-Mets was 41.4 and 58.7 %, respectively. There was no correlation of CD44 expression between primary lesions and L-Mets (r = 0.250, p = 0.071). The CD133-positive rate in primary lesions and L-Mets was 53.6 and 44.6 %, respectively. There was no correlation of CD133 expression between primary lesions and L-Mets (r = 0.219, p = 0.135). In the CD133-negative group, the MIB-1 index was significantly higher than in the CD133-positive group (61.6 vs. 46.3 %, p = 0.003), and E-cadherin expression was significantly lower in the CD133-negative group compared with the CD133-positive group (29.3 vs. 46.8 %, p = 0.001). Absence of CD133 expression in L-Mets correlated with poor overall survival (p = 0.006), and multivariate regression analysis showed that it was an independent marker for poor survival (hazard ratio 0.320, p = 0.0016).
Conclusions
The absence of CD133 expression in L-Mets was an independent marker and a poor prognostic factor, possibly because of increased proliferation and invasiveness.




Similar content being viewed by others
References
Cunningham D, Atkin W, Lenz HJ, et al. Colorectal cancer. Lancet. 2010;375:1030–47.
Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
Tanaka K, Ichikawa Y, Endo I. Liver resection for advanced or aggressive colorectal cancer metastases in the era of effective chemotherapy: a review. Int J Clin Oncol. 2011;16:452–63.
Schmoll HJ, Van Cutsem E, Stein A, et al. ESMO Consensus Guidelines for management of patients with colon and rectal cancer: a personalized approach to clinical decision making. Ann Oncol. 2012;23:2479–516.
Folprecht G, Gruenberger T, Bechstein WO, et al. Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: the CELIM randomised phase 2 trial. Lancet Oncol. 2010;11:38–47.
Vermaat JS, Nijman IJ, Koudijs MJ, et al. Primary colorectal cancers and their subsequent hepatic metastases are genetically different: implications for selection of patients for targeted treatment. Clin Cancer Res. 2012;18:688–99.
Thompson AM, Jordan LB, Quinlan P, et al. Prospective comparison of switches in biomarker status between primary and recurrent breast cancer: the Breast Recurrence in Tissues Study (BRITS). Breast Cancer Res. 2010;12:R92.
Kobayashi H, Sugihara K, Uetake H, et al. Messenger RNA expression of COX-2 and angiogenic factors in primary colorectal cancer and corresponding liver metastasis. Int J Oncol. 2009;34:1147–53.
Reya T, Morrison SJ, Clarke MF, Weissman IL. Stem cells, cancer, and cancer stem cells. Nature. 2001;414:105–11.
Nadal R, Ortega FG, Salido M, et al. CD133 expression in circulating tumor cells from breast cancer patients: potential role in resistance to chemotherapy. Int J Cancer. 2013;133:2398–407.
Tanaka K, Shimada H, Ueda M, et al. Long-term characteristics of 5-year survivors after liver resection for colorectal metastases. Ann Surg Oncol. 2007;14:1336–46.
Tanaka K, Shimada H, Miura M, et al. Metastatic tumor doubling time: most important prehepatectomy predictor of survival and nonrecurrence of hepatic colorectal cancer metastasis. World J Surg. 2004;28:263–70.
Wang Q, Chen ZG, Du CZ, et al. Cancer stem cell marker CD133+ tumour cells and clinical outcome in rectal cancer. Histopathology. 2009;55:284–93.
Wakamatsu Y, Sakamoto N, Oo HZ, et al. Expression of cancer stem cell markers ALDH1, CD44 and CD133 in primary tumor and lymph node metastasis of gastric cancer. Pathol Int. 2012;62:112–9.
Fan L, He F, Liu H, et al. CD133: a potential indicator for differentiation and prognosis of human cholangiocarcinoma. BMC Cancer. 2011;11:320.
Kopetz S, Chang GJ, Overman MJ, et al. Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol. 2009;27:3677–83.
Kobayashi S, Yamada-Okabe H, Suzuki M, et al. LGR5-positive colon cancer stem cells interconvert with drug-resistant LGR5-negative cells and are capable of tumor reconstitution. Stem Cells. 2012;30:2631–44.
Kim HJ, Kim MJ, Ahn SH, et al. Different prognostic significance of CD24 and CD44 expression in breast cancer according to hormone receptor status. Breast. 2011;20:78–85.
Yin S, Li J, Hu C, et al. CD133 positive hepatocellular carcinoma cells possess high capacity for tumorigenicity. Int J Cancer. 2007;120:1444–50.
Brescia P, Ortensi B, Fornasari L, et al. CD133 is essential for glioblastoma stem cell maintenance. Stem Cells. 2013;31:857–69.
Wen L, Chen XZ, Yang K, et al. Prognostic value of cancer stem cell marker CD133 expression in gastric cancer: a systematic review. PLoS One. 2013;8:e59154.
Mizugaki H, Sakakibara-Konishi J, Kikuchi J, et al. CD133 expression: a potential prognostic marker for non-small cell lung cancers. Int J Clin Oncol. 2013;39:1070–81.
Ahmed MA, Aleskandarany MA, Rakha EA, et al. A CD44(−)/CD24(+) phenotype is a poor prognostic marker in early invasive breast cancer. Breast Cancer Res Treat. 2012;133:979–95.
Poplawski AB, Jankowski M, Erickson SW, et al. Frequent genetic differences between matched primary and metastatic breast cancer provide an approach to identification of biomarkers for disease progression. Eur J Hum Genet. 2010;18:560–8.
Arapantoni-Dadioti P, Valavanis C, Gavressea T, et al. Discordant expression of hormone receptors and HER2 in breast cancer. A retrospective comparison of primary tumors with paired metachronous recurrences or metastases. J BUON. 2012;17:277–83.
Goranova TE, Ohue M, Shimoharu Y, Kato K. Dynamics of cancer cell subpopulations in primary and metastatic colorectal tumors. Clin Exp Metastasis. 2011;28:427–35.
Horst D, Kriegl L, Engel J, et al. CD133 expression is an independent prognostic marker for low survival in colorectal cancer. Br J Cancer. 2008;99:1285–9.
Shmelkov SV, Butler JM, Hooper AT, et al. CD133 expression is not restricted to stem cells, and both CD133+ and CD133− metastatic colon cancer cells initiate tumors. J Clin Invest. 2008;118:2111–20.
Zhao P, Li Y, Lu Y. Aberrant expression of CD133 protein correlates with Ki-67 expression and is a prognostic marker in gastric adenocarcinoma. BMC Cancer. 2010;10:218.
Hentic O, Couvelard A, Rebours V, et al. Ki-67 index, tumor differentiation, and extent of liver involvement are independent prognostic factors in patients with liver metastases of digestive endocrine carcinomas. Endocr Relat Cancer. 2011;18:51–9.
Yang J, Weinberg RA. Epithelial-mesenchymal transition: at the crossroads of development and tumor metastasis. Dev Cell. 2008;14:818–29.
Chen X, Wang Y, Xia H, et al. Loss of E-cadherin promotes the growth, invasion and drug resistance of colorectal cancer cells and is associated with liver metastasis. Mol Biol Rep. 2012;39:6707–14.
Wu Q, Guo R, Lin M, et al. MicroRNA-200a inhibits CD133/1+ ovarian cancer stem cells migration and invasion by targeting E-cadherin repressor ZEB2. Gynecol Oncol. 2011;122:149–54.
Liu HG, Pan YF, You J, et al. Expression of ABCG2 and its significance in colorectal cancer. Asian Pac J Cancer Prev. 2010;11:845–8.
Sodani K, Tiwari AK, Singh S, et al. GW583340 and GW2974, human EGFR and HER-2 inhibitors, reverse ABCG2- and ABCB1-mediated drug resistance. Biochem Pharmacol. 2012;83:1613–22.
Vasiliou V, Vasiliou K, Nebert DW. Human ATP-binding cassette (ABC) transporter family. Hum Genomics. 2009;3:281–90.
Mani SA, Guo W, Liao MJ, et al. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell. 2008;133:704–15.
Kong D, Li Y, Wang Z, Sarkar FH. Cancer stem cells and epithelial-to-mesenchymal transition (EMT)-phenotypic cells: are they cousins or twins? Cancers (Basel). 2011;3:716–29.
Ma XL, Xiao ZL, Liu L, et al. Meta-analysis of circulating tumor cells as a prognostic marker in lung cancer. Asian Pac J Cancer Prev. 2012;13:1137–44.
Pilati P, Mocellin S, Bertazza L, et al. Prognostic value of putative circulating cancer stem cells in patients undergoing hepatic resection for colorectal liver metastasis. Ann Surg Oncol. 2012;19:402–8.
Disclosure
None of the authors have any commercial interest associated with this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yamamoto, S., Tanaka, K., Takeda, K. et al. Patients with CD133-Negative Colorectal Liver Metastasis Have a Poor Prognosis After Hepatectomy. Ann Surg Oncol 21, 1853–1861 (2014). https://doi.org/10.1245/s10434-014-3549-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-3549-1