Abstract
In response to an urgent need for advanced formulations for the delivery of anti-retrovirals, a stimuli-sensitive hydrogel formulation that intravaginally delivers HIV-1 entry inhibitor upon being exposed to a specific protease was developed. The hydrogel formulation consists of PEG-azide and PEG-DBCO covalently linked to the entry inhibitor peptide, enfuvirtide, via substrate linker that is designed to undergo proteolysis by prostate specific antigen (PSA) present in seminal fluid and release innate enfuvirtide. Of the tested PSA substrate linkers (HSSKLQYY, GISSFYSSK, AYLMYY, and AYLMGRR), HSSKLQ was found to be an optimal candidate for PEG-based hydrogel with kcat/KM of 2.2 M−1 s−1. The PEG-based hydrogel displayed a pseudoplastic, thixotropic behavior with overall viscosity varying between 1516 and 2.2 Pa.s, within the biologically relevant shear rates of 0.01–100 s−1. It also exhibited viscoelastic properties appropriate for uniform spreading and being retained in vagina. PEG-based hydrogels were loaded with N3-HSSKLQ-enfuvirtide (HF42) that is customarily synthesized enfuvirtide prodrug with its N-terminus connected to HSSKLQ linker. The stimuli-sensitive PEG-based hydrogel formulations upon being exposed to PSA released 36.5 ± 4.8% of enfuvirtide over 24 h in human ejaculate mimic of vaginal simulant fluid and seminal simulant fluid mixed in 1:3 ratio, which is significantly greater than its IC50. The PEG-based hydrogel was non-cytotoxic to both vaginal epithelial cells (VK2/E6E7) and murine macrophages (RAW 264.7) and did not significantly induce the production of nitric oxide, an inflammatory mediator. The PEG-based hydrogel is found to have suitable physicochemical properties for an intravaginal formulation of the PSA substrate–linked anti-retrovirals and is safe towards vaginal epithelium. It is capable of delivering enfuvirtide with effective concentrations to prevent women from HIV-1 infection.








Similar content being viewed by others
Data Availability
The authors confirm that the data supporting the findings of this study are available on request. Raw data were generated at UMKC. Derived data supporting the findings of this study are available from the corresponding author [C Lee] on request.
References
Global HIV & AIDS statistics — 2020 fact sheet [Internet]. [cited 2021 Jan 3]. Available from: https://www.unaids.org/en/resources/fact-sheet. Accessed 16 Aug 2022
20.1 million girls and women living with HIV [Internet]. [cited 2021 Jan 3]. Available from: https://www.unaids.org/en/resources/infographics/girls-and-women-living-with-HIV. Accessed 16 Aug 2022
AIDSinfo | UNAIDS [Internet]. [cited 2020 Apr 8]. Available from: https://aidsinfo.unaids.org/. Accessed 16 Aug 2022
Abbas UL, Hood G, Wetzel AW, Mellors JW. Factors influencing the emergence and spread of HIV drug resistance arising from rollout of antiretroviral pre-exposure prophylaxis (PrEP). PLoS ONE. 2011;6(4): e18165.
Lehman DA, Baeten JM, McCoy CO, Weis JF, Peterson D, Mbara G, et al. Risk of drug resistance among persons acquiring HIV within a randomized clinical trial of single-or dual-agent preexposure prophylaxis. J Infect Dis. 2015;211(8):1211–8.
Barreto-de-Souza V, Arakelyan A, Margolis L, Vanpouille C. HIV-1 Vaginal transmission: cell-free or cell-associated virus? Am J Reprod Immunol. 2014 Jun;71(6):589–99.
Aaron E, Blum C, Seidman D, Hoyt MJ, Simone J, Sullivan M, et al. Optimizing delivery of HIV preexposure prophylaxis for women in the United States. AIDS Patient Care STDS. 2018;32(1):16–23.
Baeten JM, Hendrix CW, Hillier SL. Topical microbicides in HIV prevention: state of the promise. Annu Rev Med. 2020;71:361–77.
Musara P, Milford C, Shapley-Quinn MK, Weinrib R, Mutero P, Odoom E, et al. Preferences and acceptability of vaginal delivery forms for HIV prevention among women, male partners and key informants in South Africa and Zimbabwe: qualitative findings. AIDS Behavior. 2020;1–15.
Fang W, Mphoyi BI, Motake DR, Liu J, Li W, Mei F, et al. Efficacy, adherence and side effects of PrEP for HIV-1 prevention. IJB. 2019 Aug 29;11(4):80.
Nadendla K, Friedman SH. Light control of protein solubility through isoelectric point modulation. J Am Chem Soc. 2017 Dec 13;139(49):17861–9.
Nadendla K, Sarode BR, Friedman SH. Hydrophobic tags for highly efficient light-activated protein release. Mol Pharmaceutics. 2019 Jul 1;16(7):2922–8.
Nadendla K, Sarode B, Friedman SH. Chemical modification of proteins with photocleavable groups. In: Methods in enzymology. Elsevier; 2019. p. 113–28.
Aimetti AA, Machen AJ, Anseth KS. Poly (ethylene glycol) hydrogels formed by thiol-ene photopolymerization for enzyme-responsive protein delivery. Biomaterials. 2009;30(30):6048–54.
Azagarsamy MA, Anseth KS. Wavelength-controlled photocleavage for the orthogonal and sequential release of multiple proteins. Angew Chem. 2013;125(51):14048–52.
Wang TJ, Rittenhouse HG, Wolfert RL, Lynne CM, Brackett NL. PSA concentrations in seminal plasma. Clin Chem. 1998;44(4):895a–896.
Chan W, White P. Fmoc solid phase peptide synthesis: a practical approach. Oxford University Press; 1999. 371 p.
Nadendla VSK. Second Generation Photoactivated Insulins [Internet] [Ph.D.]. ProQuest dissertations and theses. [Ann Arbor]: University of Missouri - Kansas City; 2020. Available from: http://proxy.library.umkc.edu/login?url=https://www.proquest.com/dissertations-theses/second-generation-photoactivated-insulins/docview/2423778183/se-2?accountid=14589. Accessed 16 Aug 2022
Hakala TA, Yates EV, Challa PK, Toprakcioglu Z, Nadendla K, Matak-Vinkovic D, et al. Accelerating reaction rates of biomolecules by using shear stress in artificial capillary systems. J Am Chem Soc. 2021 Oct 13;143(40):16401–10.
Yeruva TK. Smart hydrogel for enzyme responsive vaginal delivery of anti-HIV peptide therapeutics [Internet] [Ph.D.]. ProQuest Dissertations and Theses. [Ann Arbor]: University of Missouri - Kansas City; 2021. Available from: https://www.proquest.com/dissertations-theses/smart-hydrogel-enzyme-responsive-vaginal-delivery/docview/2615117404/se-2?accountid=14696. Accessed 16 Aug 2022
Denmeade SR, Lou W, Lövgren J, Malm J, Lilja H, Isaacs JT. Specific and efficient peptide substrates for assaying the proteolytic activity of prostate-specific antigen. Can Res. 1997;57(21):4924–30.
Yu T, Malcolm K, Woolfson D, Jones DS, Andrews GP. Vaginal gel drug delivery systems: understanding rheological characteristics and performance. Expert Opin Drug Deliv. 2011;8(10):1309–22.
Zhang C, Zhang T, Oyler NA, Youan BBC. Direct and real-time quantification of tenofovir release from pH-sensitive microparticles into simulated biological fluids using 1H-NMR. J Pharm Sci. 2014 Apr;103(4):1170–7.
Owen DH, Katz DF. A vaginal fluid simulant. Contraception. 1999 Feb 1;59(2):91–5.
Patel IH, Zhang X, Nieforth K, Salgo M, Buss N. Pharmacokinetics, pharmacodynamics and drug interaction potential of enfuvirtide. Clin Pharmacokinet. 2005;44(2):175–86.
Payne RW, Nayar R, Tarantino R, Terzo SD, Moschera J, Di J, et al. Second virial coefficient determination of a therapeutic peptide by self-interaction chromatography. Peptide Science: Original Research on Biomolecules. 2006;84(5):527–33.
Owen DH, Katz DF. A review of the physical and chemical properties of human semen and the formulation of a semen simulant. J Androl. 2005;26(4):459–69.
Neves J, d, da Silva MV, Gonçalves MP, Amaral MH, Bahia MF. Rheological properties of vaginal hydrophilic polymer gels. Current Drug Delivery. 2009;6(1):83–92.
Hochmeister M. Evaluation of Prostate-Specific Antigen (PSA) Membrane tests for the forensic identification of semen. 1997;
Haase AT. Targeting early infection to prevent HIV-1 mucosal transmission. Nature. 2010 Mar;464(7286):217–23.
Veazey RS, Ketas TA, Klasse PJ, Davison DK, Singletary M, Green LC, et al. Tropism-independent protection of macaques against vaginal transmission of three SHIVs by the HIV-1 fusion inhibitor T-1249. Proc Natl Acad Sci U S A. 2008/07/22 ed. 2008 Jul 29;105(30):10531–6.
Zhang T, Sturgis TF, Youan BBC. pH-responsive nanoparticles releasing tenofovir intended for the prevention of HIV transmission. Eur J Pharm Biopharm. 2011;79(3):526–36.
Coulibaly FS, Ezoulin MJ, Purohit SS, Ayon NJ, Oyler NA, Youan BBC. Layer-by-layer engineered microbicide drug delivery system targeting HIV-1 gp120: physicochemical and biological properties. Mol Pharm. 2017;14(10):3512–27.
Agrahari V, Zhang C, Zhang T, Li W, Gounev TK, Oyler NA, et al. Hyaluronidase-sensitive nanoparticle templates for triggered release of HIV/AIDS microbicide in vitro. AAPS J. 2014;16(2):181–93.
Mattsson JM, Ravela S, Hekim C, Jonsson M, Malm J, Närvänen A, et al. Proteolytic activity of prostate-specific antigen (PSA) towards protein substrates and effect of peptides stimulating PSA activity. PLoS ONE. 2014;9(9): e107819.
Plant TM, Zeleznik AJ. (Eds.). Knobil and Neill’s physiology of reproduction (4th ed.). Academic Press; 2014;1:790–793.
Clark MR, Aliyar HA, Lee C, won, Jay JI, Gupta KM, Watson KM, et al. Enzymatic triggered release of an HIV-1 entry inhibitor from prostate specific antigen degradable microparticles. Int J Pharm. 2011;413(1–2):10–8.
LeBeau AM, Kostova M, Craik CS, Denmeade SR. Prostate-specific antigen: an overlooked candidate for the targeted treatment and selective imaging of prostate cancer. Biol Chem. 2010;391(4):333–43.
Yang CF, Porter ES, Boths J, Kanyi D, Hsieh MC, Cooperman BS. Design of synthetic hexapeptide substrates for prostate-specific antigen using single-position minilibraries. J Pept Res. 1999;54(5):444–8.
Debela M, Magdolen V, Schechter N, Valachova M, Lottspeich F, Craik CS, et al. Specificity profiling of seven human tissue kallikreins reveals individual subsite preferences. J Biol Chem. 2006;281(35):25678–88.
Nelson M, Arastéh K, Clotet B, Cooper DA, Henry K, Katlama C, et al. Durable efficacy of enfuvirtide over 48 weeks in heavily treatment-experienced HIV-1-infected patients in the T-20 versus optimized background regimen only 1 and 2 clinical trials. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2005;40(4):404–12.
Lazzarin A, Clotet B, Cooper D, Reynes J, Arastéh K, Nelson M, et al. Efficacy of enfuvirtide in patients infected with drug-resistant HIV-1 in Europe and Australia. N Engl J Med. 2003;348(22):2186–95.
Lalezari JP, Henry K, O’Hearn M, Montaner JS, Piliero PJ, Trottier B, et al. Enfuvirtide, an HIV-1 fusion inhibitor, for drug-resistant HIV infection in North and South America. N Engl J Med. 2003;348(22):2175–85.
Acknowledgements
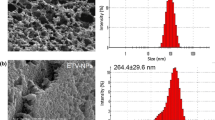
The authors thank Dr. Thomas Johnston for allowing us to use Shimadzu LC-2010A instrument. The authors acknowledge Drs. Zahra Niroobaksh and Reid Brenner for their assistance with rheological experiments and studies with FTIR spectrometer, respectively. The authors also acknowledge Dr. Donggao Zhao, the director of EM lab, UMKC school of Dentistry, for the electron microscopy service.
Funding
This study was supported by the research grant from the School of Graduate Studies in the University of Missouri-Kansas City, the Research bridge fund from Division of Pharmacology and Pharmaceutical Sciences, and the Graduate assistant fund from the UMKC women’s council.
Author information
Authors and Affiliations
Contributions
T. Yeruva: initiate, design the conception, and implementation of the work; also involved with the acquisition, analysis, and interpretation of data for the work.
C. Lee: design and drafting of the work, interpretation of data for the work, revising it critically for important intellectual content, and final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yeruva, T., Lee, C.H. Enzyme Responsive Delivery of Anti-Retroviral Peptide via Smart Hydrogel. AAPS PharmSciTech 23, 234 (2022). https://doi.org/10.1208/s12249-022-02391-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-022-02391-w