ABSTRACT
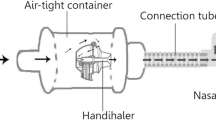
Inhalation is a promising and challenging method in pharmaceutical and biological science research. A stable environment is critical in dynamic inhalation administration. However, the establishment of a stable inhalation system is very challenging. Indacaterol glycopyrronium bromide inhalation powder (IM/GP mixed powder) is composed of indacaterol maleate and glycopyrronium bromide powder to treat chronic obstructive pulmonary disease (COPD). The aim of this study is to build suitable inhalation conditions and then to evaluate the pulmonary safety of this drug in Sprague-Dawley(SD) rats. In the research, through the coordination of the atomization flow, air pump flow, and scraper speed, aerosols were stabilized at 200 ± 20% mg/m3, and then rats were nose-only administered with the IM/GP mixed powder, Ultibro, and lactose-magnesium stearate mixed powder at 2.6 mg/kg/day for 14 days and 14 days of recovery period, respectively. After exposure, hematology, inflammatory cytokines in rats bronchoalveolar lavage fluid (BALF) and serum, histopathological examination were performed. Results showed that the stability of powder aerosols can be realized under the atomization generation flow: 10 L/min, sampling flow: 2 L/min, system pumping capacity: 10 L/min and powder scraper speed: 8–10 L/min, and there were no significant adverse effects on body weight, clinic signs, hematology, and pathology in rats. Overall, the results suggested that the IM/GP mixed powder inhalation at the dose of 2.6 mg/kg/d can be reached when the aerosol concentration is within the range of 200 ± 20% mg/m3, and there were no pulmonary toxicity effects in rats.
Graphical abstract








Similar content being viewed by others
Data availability
The data presented in this study are available upon request.
REFERENCES
Depreter F, Pilcer G, Amighi K. Inhaled proteins: Challenges and perspectives. Int J Pharm. 2013;447(1-2):251–80.
Sanchis J, Corrigan C, Levy ML, Viejo JL. Inhaler devices—from theory to practice. Respir Med. 2013;107(4):495–502.
Yang MY, Chan JG, Chan HK. Pulmonary drug delivery by powder aerosols. J Control Release. 2014;193:228–40.
Ibrahim M, Verma R, Garcia-Contreras L. Inhalation drug delivery devices: Technology update. Med Devices. 2015;8:131–9.
Pirozynski M, Sosnowski TR. Inhalation devices: From basic science to practical use, innovative vs generic products. Expert Opin Drug Deliv. 2016;13(11):1559–71.
Moon C, Smyth HDC, Watts AB, Williams RO 3rd. Delivery technologies for orally inhaled products: An update. AAPS PharmSciTech. 2019;20(3):019–1314.
Qiu Y, Liao Q, Chow MYT, Lam JKW. Intratracheal administration of dry powder formulation in mice. J Vis Exp. 2020;25(161):61469.
Morimoto Y, Izumi H, Yoshiura Y, Fujishima K, Yatera K, Yamamoto K. Usefulness of intratracheal instillation studies for estimating nanoparticle-induced pulmonary toxicity. Int J Mol Sci. 2016;17(2).
Nielsen TB, Yan J, Luna B, Spellberg B. Murine oropharyngeal aspiration model of ventilator-associated and hospital-acquired bacterial pneumonia. J Vis Exp. 2018;28(136):57672.
Kao RL, Huang W, Martin CM, Rui T. The effect of aerosolized indomethacin on lung inflammation and injury in a rat model of blunt chest trauma. Can J Surg. 2018;61(6):S208–S18.
Pauluhn J. Overview of inhalation exposure techniques: Strengths and weaknesses. Exp Toxicol Pathol. 2005;1:111–28.
Phalen RF, Mannix RC, Drew RT. Inhalation exposure methodology. Environ Health Perspect. 1984;56:23–34.
Świercz R, Wąsowicz W. The distribution and excretion of 1-Methylnaphthalene in rats exposed to 1-Methylnaphthalene by inhalation. Int J Occup Med Environ Health. 2018;31(6):763–70.
Wong BA. Inhalation exposure systems: design, methods and operation. Toxicol Pathol. 2007;35(1):3–14.
Pauluhn J, Mohr U. Inhalation studies in laboratory animals—current concepts and alternatives. Toxicol Pathol. 2000;28(5):734–53.
Cheng YS. Mechanisms of pharmaceutical aerosol deposition in the respiratory tract. AAPS PharmSciTech. 2014;15(3):630–40.
Kolli AR, Kuczaj AK, Martin F, Hayes AW, Peitsch MC, Hoeng J. Bridging inhaled aerosol dosimetry to physiologically based pharmacokinetic modeling for toxicological assessment: nicotine delivery systems and beyond. Crit Rev Toxicol. 2019;49(9):725–41.
Patil TS, Deshpande A, Shende PK, Deshpande S, Gaud R. Evaluation of nanocarrier-based dry powder formulations for inhalation with special reference to anti-tuberculosis drugs. Crit Rev Ther Drug Carrier Syst. 2019;36(3):239–76.
Viniol C, Vogelmeier CF. Exacerbations of COPD. Eur Respir Rev. 2018;27(147):0103–2017.
Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, Chen R, Decramer M, Fabbri LM, Frith P, Halpin DMG, López Varela MV, Nishimura M, Roche N, Rodriguez-Roisin R, Sin DD, Singh D, Stockley R, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD Executive Summary. Am J Respir Crit Care Med. 2017;195(5):557–82.
GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med. 2017;5(9):691–706. https://doi.org/10.1016/S2213-2600(17)30293-X.
Mirza S, Clay RD, Koslow MA, Scanlon PD. COPD guidelines: a review of the 2018 GOLD report. Mayo Clin Proc. 2018;93(10):1488–502.
Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163(5):1256–76.
Rodriquez-Roisin R. Twenty years of GOLD (1997–2017). The origins. 2020. https://goldcopd.org/wp-content/uploads/2019/03/GOLD-Origins-Final-Version-mar19.pdf.
Horita N, Nagashima A, Kaneko T. Long-acting β-agonists (LABA) combined with long-acting muscarinic antagonists or LABA combined with inhaled corticosteroids for patients with stable COPD. Jama. 2017;318(13):1274–5.
Terry PD, Dhand R. Inhalation therapy for stable COPD: 20 years of GOLD reports. Adv Ther. 2020;37(5):1812–28.
Bolon B, Baze W, Shilling CJ, Keatley KL, Patrick DJ, Schafer KA. Good laboratory practice in the academic setting: fundamental principles for nonclinical safety assessment and GLP-compliant pathology support when developing innovative biomedical products. ILAR J. 2018;59(1):18–28.
Nussberger J, Aubert JF, Bouzourene K, Pellegrin M, Hayoz D, Mazzolai L. Renin inhibition by aliskiren prevents atherosclerosis progression: Comparison with irbesartan, atenolol, and amlodipine. Hypertension. 2008;51(5):1306–11.
Alexander DJ, Collins CJ, Coombs DW, Gilkison IS, Hardy CJ, Healey G, Karantabias G, Johnson N, Karlsson A, Kilgour JD, McDonald P. Association of Inhalation Toxicologists (AIT) working party recommendation for standard delivered dose calculation and expression in non-clinical aerosol inhalation toxicology studies with pharmaceuticals. Inhal Toxicol. 2008;20(13):1179–89.
OECD. Test No. 412: subacute inhalation toxicity: 28-day study, OECD guidelines for the testing of chemicals, section 4. Paris: OECD Publishing; 2018. https://doi.org/10.1787/9789264070783-en.
Riva DR, Magalhães CB, Lopes AA, Lanças T, Mauad T, Malm O, Valença SS, Saldiva PH, Faffe DS, Zin WA. Low dose of fine particulate matter (PM2.5) can induce acute oxidative stress, inflammation and pulmonary impairment in healthy mice. Inhal Toxicol. 2011;23(5):257–67.
DiPietro LA, Burdick M, Low QE, Kunkel SL, Strieter RM. MIP-1alpha as a critical macrophage chemoattractant in murine wound repair. J Clin Invest. 1998;101(8):1693–8.
Wang Y, Wang H, Zhang C, Zhang C, Yang H, Gao R, Tong Z. Lung fluid biomarkers for acute respiratory distress syndrome: A systematic review and meta-analysis. Crit Care. 2019;23(1):019–2336.
Barnes PJ, Burney PG, Silverman EK, Celli BR, Vestbo J, Wedzicha JA, et al. Chronic obstructive pulmonary disease. Nat Rev Dis Primers. 2015;1(15076):76.
Yoon HK, Park YB, Rhee CK, Lee JH, Oh YM. Summary of the chronic obstructive pulmonary disease clinical practice guideline revised in 2014 by the korean academy of tuberculosis and respiratory disease. Tuberc Respir Dis. 2017;80(3):230–40.
Reagan-Shaw S, Nihal M, Ahmad N. Dose translation from animal to human studies revisited. FASEB J. 2008;22(3):659–61.
Choi HY, Lee YH, Lim CH, Kim YS, Lee IS, Jo JM, Lee HY, Cha HG, Woo HJ, Seo DS. Assessment of respiratory and systemic toxicity of Benzalkonium chloride following a 14-day inhalation study in rats. Part Fibre Toxicol. 2020;17(1):020–0339.
Lim D, Jeong J, Song KS, Sung JH, Oh SM, Choi J. Inhalation toxicity of polystyrene micro(nano)plastics using modified OECD TG 412. Chemosphere. 2021;262(128330):13.
Labiris NR, Dolovich MB. Pulmonary drug delivery. Part I: Physiological factors affecting therapeutic effectiveness of aerosolized medications. Br J Clin Pharmacol. 2003;56(6):588–99.
Martin AR, Moore CP, Finlay WH. Models of deposition, pharmacokinetics, and intersubject variability in respiratory drug delivery. Expert Opin Drug Deliv. 2018;15(12):1175–88.
Zanen P, Go LT, Lammers JW. The efficacy of a low-dose, monodisperse parasympathicolytic aerosol compared with a standard aerosol from a metered-dose inhaler. Eur J Clin Pharmacol. 1998;54(1):27–30.
Acknowledgements
The authors thank Yangteng Ou (University of Cambridge, UK) for some proofreading work.
Funding
This work was supported by the National Natural Science Foundation of China under Grant (81773479), the National Major Science and Technology Projects of China under Grant (2017ZX09201002-004), and the research project of Jiangsu Commission of Health (H201634).
Author information
Authors and Affiliations
Contributions
ZF: methodology, investigation, validation, data curation, writing—original draft. BZ: methodology, validation, investigation, writing—review and editing. YL: methodology, investigation, validation, writing—review and editing. WS: methodology, investigation, formal analysis. YF: validation, resources, data curation. HL: formal analysis, writing—review and editing. DC: validation, writing—review and editing. KL: validation, writing—review and editing. XW: writing—review and editing. TX: writing—review and editing. WX: resources, writing—review and editing. QB: conceptualization, resources, writing—review and editing, supervision, project administration, funding acquisition. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Fan, Z., Zhou, B., Liu, Y. et al. Optimization and Application of an Efficient and Stable Inhalation Exposure System for Rodents. AAPS PharmSciTech 23, 50 (2022). https://doi.org/10.1208/s12249-021-02191-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-021-02191-8