Abstract
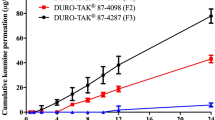
The objective of this study was to develop a lappaconitine (LA) transdermal patch with counter-ion to increase the transdermal permeability of the drug, and a theory of counter-ion altering the conformation of the skin keratin was put forward based on the in vitro skin permeation study and physicochemical properties of ion-pairs. Formulation factors including pressure sensitive adhesives (PSAs), drug-loading, counter-ions and molar ratios of counter-ion were screened by in vitro skin permeation study. The optimized formulation was composed of 7% LA, 1.5 mole cinnamic acid and AAOH (PSA containing hydroxyl group synthesized by our laboratory) as an adhesive matrix. The optimized patch was evaluated by the pharmacokinetic and analgesic pharmacodynamic studies. AUC0–t and pain inhibition ratio of the optimized patch were 2450.40 ± 848.52 h ng/mL and 81.18%, which showed good absorption into the skin and excellent analgesic effect. The mechanism of facilitated transdermal drug permeation by counter-ion was investigated by ATR-FTIR, thermal analysis, FTIR, XPS and molecular docking. The results indicated that after the formation of ion-pairs, the excess counter-ions would alter the conformation of the skin keratin, thus increasing the transdermal penetration of LA. In conclusion, the LA patch was successfully optimized, and the effect of counter-ions on the skin was clarified at the molecular level. These findings provided additional references for the application of counter-ion in the transdermal drug delivery system.











Similar content being viewed by others
References
Y-f L, Zheng Y-m YY, Gan Y, Gao Z-b. Inhibitory effects of lappaconitine on the neuronal isoforms of voltage-gated sodium channels. Acta Pharmacol Sin. 2019;40(4):451–9.
Wright SN. Irreversible block of human heart (hH1) sodium channels by the plant alkaloid lappaconitine. Mol Pharmacol. 2001;59(2):183–92.
Ou S, Zhao Y-D, Xiao Z, Wen H-Z, Cui J, Ruan H-Z. Effect of lappaconitine on neuropathic pain mediated by P2X3 receptor in rat dorsal root ganglion. Neurochem Int. 2011;58(5):564–73.
Chen F, Shen X, Huang P, Fu H, Jin Y, Wen C. Quantification of lappaconitine in mouse blood by UPLC-MS/MS and its application to a pharmacokinetic study. Biomed Res Int. 2019;2019:1–6.
Alkilani AZ, McCrudden MT, Donnelly RF. Transdermal drug delivery: innovative pharmaceutical developments based on disruption of the barrier properties of the stratum corneum. Pharmaceutics. 2015;7(4):438–70.
Teng G, Zhang X, Zhang C, Chen L, Sun W, Qiu T, Zhang J. Lappaconitine trifluoroacetate contained polyvinyl alcohol nanofibrous membranes: characterization, biological activities and transdermal application. Mater Sci Eng C. 2020;108:110515.
Prausnitz MR, Langer R. Transdermal drug delivery. Nat Biotechnol. 2008;26(11):1261–8.
Prausnitz MR, Mitragotri S, Langer R. Current status and future potential of transdermal drug delivery. Nat Rev Drug Discov. 2004;3(2):115–24.
Barry BW. Novel mechanisms and devices to enable successful transdermal drug delivery. Eur J Pharm Sci. 2001;14(2):101–14.
Wang H, Tian Q, Quan P, Liu C, Fang L. Probing the role of ion-pair strategy in controlling dexmedetomidine penetrate through drug-in-adhesive patch: mechanistic insights based on release and percutaneous absorption process. AAPS PharmSciTech. 2020;21(1):1–14.
Ma X, Fang L, Guo J, Zhao N, He Z. Effect of counter-ions and penetration enhancers on the skin permeation of flurbiprofen. J Pharm Sci. 2010;99(4):1826–37.
Nam SH, Xu YJ, Nam H, Jin G-W, Jeong Y, An S, et al. Ion pairs of risedronate for transdermal delivery and enhanced permeation rate on hairless mouse skin. Int J Pharm. 2011;419(1-2):114–20.
Song T, Quan P, Xiang R, Fang L. Regulating the skin permeation rate of escitalopram by ion-pair formation with organic acids. AAPS PharmSciTech. 2016;17(6):1267–73.
Liu C, Quan P, Li S, Zhao Y, Fang L. A systemic evaluation of drug in acrylic pressure sensitive adhesive patch in vitro and in vivo: the roles of intermolecular interaction and adhesive mobility variation in drug controlled release. J Control Release. 2017;252:83–94.
Li Q, Wan X, Liu C, Fang L. Investigating the role of ion-pair strategy in regulating nicotine release from patch: mechanistic insights based on intermolecular interaction and mobility of pressure sensitive adhesive. Eur J Pharm Sci. 2018;119:102–11.
Lu Y, Kim S, Park K. In vitro–in vivo correlation: perspectives on model development. Int J Pharm. 2011;418(1):142–8.
Quan P, Jiao B, Shang R, Liu C, Fang L. Alternative therapy of rheumatoid arthritis with a novel transdermal patch containing Siegesbeckiae Herba extract. J Ethnopharmacol. 2021;265:113294.
Berton P, Di Bona KR, Yancey D, Rizvi SA, Gray M, Gurau G, et al. Transdermal bioavailability in rats of lidocaine in the forms of ionic liquids, salts, and deep eutectic. ACS Med Chem Lett. 2017;8(5):498–503.
Zhao H, Liu C, Quan P, Wan X, Shen M, Fang L. Mechanism study on ion-pair complexes controlling skin permeability: effect of ion-pair dissociation in the viable epidermis on transdermal permeation of bisoprolol. Int J Pharm. 2017;532(1):29–36.
Kalia YN, Guy RH. Modeling transdermal drug release. Adv Drug Delivery Rev. 2001;48(2-3):159–72.
Jiang J, Quan P, Chen Y, Fang L. Mechanistic investigation and reversible effect of 2-isopropyl-5-methylcyclohexyl heptanoate on the in vitro percutaneous absorption of indomethacin. Drug Deliv. 2014;21(1):26–33.
Yang D, Liu C, Piao H, Quan P, Fang L. Enhanced drug loading in the drug-in-adhesive transdermal patch utilizing a drug–ionic liquid strategy: insight into the role of ionic hydrogen bonding. Mol Pharm. 2021;18(3):1157–66.
Liu X, Quan P, Li S, Liu C, Zhao Y, Zhao Y, Fang L. Time dependence of the enhancement effect of chemical enhancers: molecular mechanisms of enhancing kinetics. J Control Release. 2017;248:33–44.
Uppoor VRS. Regulatory perspectives on in vitro (dissolution)/in vivo (bioavailability) correlations. J Control Release. 2001;72(1-3):127–32.
Schiller R, Funke A, Günther C. DSC measurements on full thickness mice skin. J Therm Anal Calorim. 2004;77(2):497–510.
Anselmo AC, Gokarn Y, Mitragotri S. Non-invasive delivery strategies for biologics. Nat Rev Drug Discov. 2019;18(1):19–40.
Liu C, Hui M, Quan P, Fang L. Drug in adhesive patch of palonosetron: effect of pressure sensitive adhesive on drug skin permeation and in vitro-in vivo correlation. Int J Pharm. 2016;511(2):1088–97.
Fang L, Numajiri S, Kobayashi D, Ueda H, Nakayama K, Miyamae H, Morimoto Y. Physicochemical and crystallographic characterization of mefenamic acid complexes with alkanolamines. J Pharm Sci. 2004;93(1):144–54.
Strati F, Neubert RH, Opálka L, Kerth A, Brezesinski G. Non-ionic surfactants as innovative skin penetration enhancers: insight in the mechanism of interaction with simple 2D stratum corneum model system. Eur J Pharm Sci. 2021;157:105620.
Notman R, den Otter WK, Noro MG, Briels WJ, Anwar J. The permeability enhancing mechanism of DMSO in ceramide bilayers simulated by molecular dynamics. Biophys J. 2007;93(6):2056–68.
Babita K, Kumar V, Rana V, Jain S, Tiwary AK. Thermotropic and spectroscopic behavior of skin: relationship with percutaneous permeation enhancement. Curr Drug Deliv. 2006;3(1):95–113.
Kaushik D, Michniak-Kohn B. Percutaneous penetration modifiers and formulation effects: thermal and spectral analyses. AAPS PharmSciTech. 2010;11(3):1068–83.
Boncheva M, Damien F, Normand V. Molecular organization of the lipid matrix in intact Stratum corneum using ATR-FTIR spectroscopy. BBA-Biomembranes. 2008;1778(5):1344–55.
Tamm LK, Tatulian SA. Infrared spectroscopy of proteins and peptides in lipid bilayers. Q Rev Biophys. 1997;30(4):365–429.
Cai Y, Tian Q, Liu C, Fang L. Development of long-acting rivastigmine drug-in-adhesive patch utilizing ion-pair strategy and characterization of controlled release mechanism. Eur J Pharm Sci. 2021;161:105774.
Author information
Authors and Affiliations
Contributions
ML: methodology, investigation, formal analysis, data curation, writing—original draft. CL: supervision, writing—review and editing. YC: resources. HS: investigation, formal analysis, validation. LF: conceptualization, resources, project administration, funding acquisition.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 4640 kb)
Rights and permissions
About this article
Cite this article
Li, M., Liu, C., Cai, Y. et al. Transdermal Enhancement Strategy of Lappaconitine: Alteration of Keratin Configuration by Counter-Ion. AAPS PharmSciTech 23, 61 (2022). https://doi.org/10.1208/s12249-021-02190-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-021-02190-9