Abstract
Presently, most of the treatment strategies for cancer are focused on the surgical removal of cancerous tumors, along with physical and chemical treatment such as radiotherapy and chemotherapy, respectively. The primary issue associated with these methods is the inhibition of normal cell growth and serious side effects associated with systemic toxicity. The traditional chemotherapeutics which were delivered systemically were inadequate and had serious dose limiting side effects. Recent advances in the development of chemotherapeutics have simultaneously paved the way for efficient targeted drug delivery. Despite the advances in the field of oncogenic drugs, several limitations remain, such as early blood clearance, acquired resistance against cytotoxic agents, toxicity associated with chemotherapeutics, and site-specific drug delivery. Hence, this review article focuses on the recent scientific advancements made in different types of drug delivery systems, including, organic nanocarriers (polymers, albumins, liposomes, and micelles), inorganic nanocarriers (mesoporous silica nanoparticles, gold nanoparticles, platinum nanoparticles, and carbon nanotubes), aptamers, antibody–drug conjugates, and peptides. These targeted drug delivery approaches offer numerous advantages such as site-specific drug delivery, minimal toxicity, better bioavailability, and an increased overall efficacy of the chemotherapeutics.

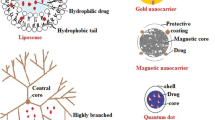
Graphical abstract


Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7–30.
Pérez-Herrero E, Fernández-Medarde A. Advanced targeted therapies in cancer: drug nanocarriers, the future of chemotherapy. Eur J Pharm Biopharm. 2015;93:52–79.
Zhao J. Cancer stem cells and chemoresistance: The smartest survives the raid. Pharmacol Ther. 2016;160:145–58.
Yao Y, Zhou Y, Liu L, Xu Y, Chen Q, Wang Y, et al. Nanoparticle-based drug delivery in cancer therapy and its role in overcoming drug resistance. Front Mol Biosci. 2020;7:193.
Patra JK, Das G, Fraceto LF, Campos EVR, Rodriguez-Torres MDP, Acosta-Torres LS, et al. Nano based drug delivery systems: recent developments and future prospects. J Nanobiotechnology. 2018;16(1):71.
Sun J, Yang Z, Teng L. Nanotechnology and microtechnology in drug delivery systems. Dose Response. 2020;18(2):1559325820907810.
Rocha M, Chaves N, Bao S. Nanobiotechnology for breast cancer treatment. In: Van Pham P, editor. Breast Cancer - From Biology to Medicine. London, England: InTech; 2017.
Yan L, Shen J, Wang J, Yang X, Dong S, Lu S. Nanoparticle-based drug delivery system: a patient-friendly chemotherapy for oncology. Dose Response. 2020;18(3):1559325820936161.
Kumar S, Randhawa JK. High melting lipid based approach for drug delivery: solid lipid nanoparticles. Mater Sci Eng C Mater Biol Appl. 2013;33(4):1842–52.
Peng Y, Bariwal J, Kumar V, Tan C, Mahato RI. Organic nanocarriers for delivery and targeting of therapeutic agents for cancer treatment. Adv Ther (Weinh). 2020;3(2):1900136.
Song SY, Kim K-P, Jeong S-Y, Park J, Park J, Jung J, et al. Polymeric nanoparticle-docetaxel for the treatment of advanced solid tumors: phase I clinical trial and preclinical data from an orthotopic pancreatic cancer model. Oncotarget. 2016;7(47):77348–57.
Hou S, Schmid A, Desai N. Abstract 348: ABI-009 (nab-Sirolimus) improves tumor accumulation and antitumor activity over oral mTOR inhibitors. In: Experimental and Molecular Therapeutics. American Association for Cancer Research; 2019. p. 348–348.
ABI-008 Trial in Patients With Hormone-refractory Prostate Cancer [Internet]. Clinicaltrials.gov. [cited 2021 Oct 4]. Available from: https://clinicaltrials.gov/ct2/show/NCT00477529. Accessed 4 Oct 2021
Autio KA, et al. Safety and efficacy of BIND-014, a docetaxel nanoparticle targeting prostate-specific membrane antigen for patients with metastatic castration-resistant prostate cancer: a phase 2 clinical trial. JAMA Oncol. 2018;4(10):1344.
Voss MH, Hussain A, Vogelzang N, Lee JL, Keam B, Rha SY, et al. A randomized phase II trial of CRLX101 in combination with bevacizumab versus standard of care in patients with advanced renal cell carcinoma. Ann Oncol. 2017;28(11):2754–60.
Ruman U, Fakurazi S, Masarudin MJ, Hussein MZ. Nanocarrier-based therapeutics and theranostics drug delivery systems for next generation of liver cancer nanodrug modalities. Int J Nanomedicine. 2020;15:1437–56.
Avramović N, Mandić B, Savić-Radojević A, Simić T. Polymeric nanocarriers of drug delivery systems in cancer therapy. Pharmaceutics. 2020;12(4):298.
M. E. Grigore, “Organic and inorganic nano-systems used in cancer treatment,” Journal of Medical Research and Health Education, vol. 1, no. 1, 2017.
Kahraman E, Güngör S, Özsoy Y. Potential enhancement and targeting strategies of polymeric and lipid-based nanocarriers in dermal drug delivery. Ther Deliv. 2017;8(11):967–85.
Zhao M, Lei C, Yang Y, Bu X, Ma H, Gong H, et al. Abraxane, the nanoparticle formulation of paclitaxel can induce drug resistance by up-regulation of P-gp. PLoS One. 2015;10(7):e0131429.
ABI-008 Trial in Patients With Hormone-refractory Prostate Cancer [Internet]. Clinicaltrials.gov. [cited 2021 Oct 2]. Available from: https://clinicaltrials.gov/ct2/show/NCT00477529. Accessed 2 Oct 2021
Weiss GJ, Chao J, Neidhart JD, Ramanathan RK, Bassett D, Neidhart JA, et al. First-in-human phase 1/2a trial of CRLX101, a cyclodextrin-containing polymer-camptothecin nanopharmaceutical in patients with advanced solid tumor malignancies. Invest New Drugs. 2013;31(4):986–1000.
UPDATED: Cerulean Pharma’s lead nanodrug crashes in lung cancer study [Internet]. Fiercebiotech.com. 2013 [cited 2021 Oct 2]. Available from: https://www.fiercebiotech.com/venture-capital/updated-cerulean-pharma-s-lead-nanodrug-crashes-lung-cancer-study. Accessed 2 Oct 2021
Zhou Q, Sun X, Zeng L, Liu J, Zhang Z. A randomized multicenter phase II clinical trial of mitoxantrone-loaded nanoparticles in the treatment of 108 patients with unresected hepatocellular carcinoma. Nanomedicine. 2009;5(4):419–23.
Saraf S, Jain A, Tiwari A, Verma A, Panda PK, Jain SK. Advances in liposomal drug delivery to cancer: an overview. J Drug Deliv Sci Technol. 2020;56(101549):101549.
Malhi SS, Budhiraja A, Arora S, Chaudhari KR, Nepali K, Kumar R, et al. Intracellular delivery of redox cycler-doxorubicin to the mitochondria of cancer cell by folate receptor targeted mitocancerotropic liposomes. Int J Pharm. 2012;432(1–2):63–74.
Fernandes C, Suares D, Yergeri MC. Tumor microenvironment targeted nanotherapy. Front Pharmacol. 2018;9:1230.
Malhi S, Dixit K, Sohi H, Shegokar R. Expedition of liposomes to intracellular targets in solid tumors after intravenous administration. J Pharm Investig. 2013;43(2):75–87.
Besse HC, Barten-van Rijbroek AD, van der Wurff-Jacobs KMG, Bos C, Moonen CTW, Deckers R. Tumor drug distribution after local drug delivery by hyperthermia, in vivo. Cancers (Basel). 2019;11(10):1512.
Zahednezhad F, Zakeri-Milani P, ShahbazMojarrad J, Valizadeh H. The latest advances of cisplatin liposomal formulations: essentials for preparation and analysis. Expert Opin Drug Deliv. 2020;17(4):523–41.
Shepard R. Pb1743 liposomal annamycin - a new generation anthracycline that overcomes mdr and has no cardiac toxicity for the treatment of r/r aml: PB1743. HemaSphere. 2019;3(S1):801–2.
Koudelka S, Turánek J. Liposomal paclitaxel formulations. J Control Release. 2012;163(3):322–34.
Bulbake U, Doppalapudi S, Kommineni N, Khan W. Liposomal formulations in clinical use: an updated review. Pharmaceutics. 2017;9(2):12.
Si Y, Xu Y, Guan J, Chen K, Kim S, Yang ES, et al. Anti-EGFR antibody-drug conjugate for triple-negative breast cancer therapy. Eng Life Sci. 2021;21(1–2):37–44.
Wang R-H, Cao H-M, Tian Z-J, Jin B, Wang Q, Ma H, et al. Efficacy of dual-functional liposomes containing paclitaxel for treatment of lung cancer. Oncol Rep. 2015;33(2):783–91.
Dunne M, Epp-Ducharme B, Sofias AM, Regenold M, Dubins DN, Allen C. Heat-activated drug delivery increases tumor accumulation of synergistic chemotherapies. J Control Release. 2019;308:197–208.
Serinan E, Department of Basic Oncology, DokuzEylul University Institute of Oncology, Izmir, Turkey, Altun Z, Aktas S, Cecen E, Olgun N, et al Comparison of cisplatin with lipoplatin in terms of ototoxicity. J Int Adv Otol 2018;14 (2):211–5.
Chen L-T, Su M-H. EndoTAG-1 plus gemcitabine versus gemcitabine alone in patients with measurable locally advanced and/or metastatic adenocarcinoma of the pancreas failed on FOLFIRINOX treatment (NCT03126435). J Clin Oncol. 2020;38(15_suppl):TPS4669–TPS4669.
Hsu W-C, Cheng C-N, Lee T-W, Hwang J-J. Cytotoxic effects of PEGylated anti-EGFR immunoliposomes combined with doxorubicin and rhenium-188 against cancer cells. Anticancer Res. 2015;35(9):4777–88.
Fu H, Shi K, Hu G, Yang Y, Kuang Q, Lu L, et al. Tumor-targeted paclitaxel delivery and enhanced penetration using TAT-decorated liposomes comprising redox-responsive poly(ethylene glycol). J Pharm Sci. 2015;104(3):1160–73.
Mallya P, Gowda DV, Mahendran B, Bhavya MV, Jain V. Recent developments in nano micelles as drug delivery system. Int j res pharm sci. 2020;11(1):176–84.
Senapati S, Mahanta AK, Kumar S, Maiti P. Controlled drug delivery vehicles for cancer treatment and their performance. Signal Transduct Target Ther. 2018;3(1):7.
Werner ME, Cummings ND, Sethi M, Wang EC, Sukumar R, Moore DT, et al. Preclinical evaluation of Genexol-PM, a nanoparticle formulation of paclitaxel, as a novel radiosensitizer for the treatment of non-small cell lung cancer. Int J Radiat Oncol Biol Phys. 2013;86(3):463–8.
Subbiah V, Grilley-Olson JE, Combest AJ, Sharma N, Tran RH, Bobe I, et al. Phase Ib/II trial of NC-6004 (nanoparticle cisplatin) plus gemcitabine in patients with advanced solid tumors. Clin Cancer Res. 2018;24(1):43–51.
Fujiwara Y, Mukai H, Saeki T, Ro J, Lin Y-C, Nagai SE, et al. A multi-national, randomised, open-label, parallel, phase III non-inferiority study comparing NK105 and paclitaxel in metastatic or recurrent breast cancer patients. Br J Cancer. 2019;120(5):475–80.
Docetaxel-polymeric Micelles(PM) and Oxaliplatin for esophageal carcinoma - full text view - ClinicalTrials.Gov [Internet]. Clinicaltrials.gov. [cited 2021 Oct 2]. Available from: https://clinicaltrials.gov/ct2/show/NCT03585673. Accessed 2 Oct 2021
Atrafi F, van Eerden RAG, van HylckamaVlieg MAM, Oomen-de Hoop E, de Bruijn P, Lolkema MP, et al. Intratumoral comparison of nanoparticle entrapped docetaxel (CPC634) with conventional docetaxel in patients with solid tumors. Clin Cancer Res. 2020;26(14):3537–45.
Chawla SP, Goel S, Chow W, Braiteh F, Singh AS, Olson JEG, et al. A phase 1b dose escalation trial of NC-6300 (nanoparticle epirubicin) in patients with advanced solid tumors or advanced, metastatic, or unresectable soft-tissue sarcoma. Clin Cancer Res. 2020;26(16):4225–32.
Atrafi F, Dumez H, Mathijssen RHJ, Menke CW, Costermans J, Rijcken CJF, et al. A phase I dose-finding and pharmacokinetics study of CPC634 (nanoparticle entrapped docetaxel) in patients with advanced solid tumors. J Clin Oncol. 2019;37(15_suppl):3026–3026.
Efficacy Study of CPC634 (CriPec® Docetaxel) in Platinum Resistant Ovarian Cancer - Full Text View - ClinicalTrials.Gov [Internet]. Clinicaltrials.gov. [cited 2021 Oct 2]. Available from:https://clinicaltrials.gov/ct2/show/NCT03742713
Bayda S, Hadla M, Palazzolo S, Riello P, Corona G, Toffoli G, et al. Inorganic nanoparticles for cancer therapy: a transition from lab to clinic. Curr Med Chem. 2018;25(34):4269–303.
Kundu M, Chatterjee S, Ghosh N, Manna P, Das J, Sil PC. Tumor targeted delivery of umbelliferone via a smart mesoporous silica nanoparticles controlled-release drug delivery system for increased anticancer efficiency. Mater Sci Eng C Mater Biol Appl. 2020;116(111239):111239.
Lee N-K, Park SS, Ha C-S. PH-sensitive drug delivery system based on mesoporous silica modified with poly-L-lysine (PLL) as a gatekeeper. J NanosciNanotechnol. 2020;20(11):6925–34.
Cai D, Han C, Liu C, Ma X, Qian J, Zhou J, et al. Chitosan-capped enzyme-responsive hollow mesoporous silica nanoplatforms for colon-specific drug delivery. Nanoscale Res Lett. 2020;15(1):123.
Sreejivungsa K, Suchaichit N, Moosophon P, Chompoosor A. Light-regulated release of entrapped drugs from photoresponsive gold nanoparticles. J Nanomater. 2016;2016:1–7.
Ramalingam V, Varunkumar K, Ravikumar V, Rajaram R. Target delivery of doxorubicin tethered with PVP stabilized gold nanoparticles for effective treatment of lung cancer. Sci Rep. 2018;8(1):3815.
Farooq MU, Novosad V, Rozhkova EA, Wali H, Ali A, Fateh AA, et al. Gold nanoparticles-enabled efficient dual delivery of anticancer therapeutics to HeLa cells. Sci Rep. 2018;8(1):2907.
Agabeigi R, Rasta SH, Rahmati-Yamchi M, Salehi R, Alizadeh E. Novel chemo-photothermal therapy in breast cancer using methotrexate-loaded folic acid conjugated Au@SiO2 nanoparticles. Nanoscale Res Lett. 2020;15(1):62.
Jeyaraj M, Gurunathan S, Qasim M, Kang M-H, Kim J-H. A comprehensive review on the synthesis, characterization, and biomedical application of platinum nanoparticles. Nanomaterials (Basel). 2019;9(12):1719.
Fu B, Dang M, Tao J, Li Y, Tang Y. Mesoporous platinum nanoparticle-based nanoplatforms for combined chemo-photothermal breast cancer therapy. J Colloid Interface Sci. 2020;570:197–204.
Al-Karam LQ, Al-Neami AQ. Study of platinum nanoparticles with methotrexate as drug delivery system for cancer therapy on MCF7. Available from: http://impactfactor.org/PDF/IJDDT/9/IJDDT,Vol9,Issue4,Article10.pdf
Roldo M. Carbon nanotubes in drug delivery: just a carrier? Ther Deliv. 2016;7(2):55–7.
OmurtagOzgen PS, Atasoy S, Zengin Kurt B, Durmus Z, Yigit G, Dag A. Glycopolymer decorated multiwalled carbon nanotubes for dual targeted breast cancer therapy. J Mater Chem B Mater Biol Med. 2020;8(15):3123–37.
Daima HK, Selvakannan PR, Shukla R, Bhargava SK, Bansal V. Fine-tuning the antimicrobial profile of biocompatible gold nanoparticles by sequential surface functionalization using polyoxometalates and lysine. PLoS One. 2013;8(10):e79676.
Shi J, Kantoff PW, Wooster R, Farokhzad OC. Cancer nanomedicine: progress, challenges and opportunities. Nat Rev Cancer. 2017;17(1):20–37.
Navya PN, Kaphle A, Srinivas SP, Bhargava SK, Rotello VM, Daima HK. Current trends and challenges in cancer management and therapy using designer nanomaterials. Nano Converg. 2019;6(1):23.
Yoon S, Rossi JJ. Emerging cancer-specific therapeutic aptamers. CurrOpin Oncol. 2017;29(5):366–74.
Mitra AK, Agrahari V, Mandal A, Cholkar K, Natarajan C, Shah S, et al. Novel delivery approaches for cancer therapeutics. J Control Release. 2015;219:248–68.
Kim M, Kim D-M, Kim K-S, Jung W, Kim D-E. Applications of cancer cell-specific aptamers in targeted delivery of anticancer therapeutic agents. Molecules. 2018;23(4):830.
Fu Z, Xiang J. Aptamers, the nucleic acid antibodies, in cancer therapy. Int J Mol Sci [Internet]. 2020;21(8). Available from: https://www.mdpi.com/resolver?pii=ijms21082793. Accessed 2 Oct 2021
Clinical Study Of Pegaptanib Sodium (EYE001) For wet-type age-related macular degeneration [Internet]. Clinicaltrials.gov. [cited 2021 Oct 2]. Available from:https://clinicaltrials.gov/ct2/show/NCT00239928
Zhou J, Rossi J. Aptamers as targeted therapeutics: current potential and challenges. Nat Rev Drug Discov. 2017;16(3):181–202.
Boyer DS, Goldbaum M, Leys AM, Starita C, V.I.S.I.O.N. Study Group. Effect of pegaptanib sodium 0.3 mg intravitreal injections (Macugen) in intraocular pressure: posthoc analysis from V.I.S.I.O.N. study. Br J Ophthalmol. 2014;98 (11):1543–6.
Powell Gray B, Song X, Hsu DS, Kratschmer C, Levy M, Barry AP, et al. An aptamer for broad cancer targeting and therapy. Cancers (Basel). 2020;12(11):3217.
Khongorzul P, Ling CJ, Khan FU, Ihsan AU, Zhang J. Antibody-drug conjugates: a comprehensive review. Mol Cancer Res. 2020;18(1):3–19.
Xu Z, Guo D, Jiang Z, Tong R, Jiang P, Bai L, et al. Novel HER2-targeting antibody-drug conjugates of trastuzumab beyond T-DM1 in breast cancer: trastuzumab deruxtecan(DS-8201a) and (Vic-)trastuzumab duocarmazine (SYD985). Eur J Med Chem. 2019;183(111682):111682.
Hong R, Xia W, Wang L, Lee K, Lu Q, Jiang K, et al. Safety, tolerability, and pharmacokinetics of BAT8001 in patients with HER2-positive breast cancer: an open-label, dose-escalation, phase I study. Cancer Commun (Lond) [Internet]. 2021;(cac2.12135). Available from: https://pubmed.ncbi.nlm.nih.gov/33528890/
O’Malley DM, Matulonis UA, Birrer MJ, Castro CM, Gilbert L, Vergote I, et al. Phase Ib study of mirvetuximabsoravtansine, a folate receptor alpha (FRα)-targeting antibody-drug conjugate (ADC), in combination with bevacizumab in patients with platinum-resistant ovarian cancer. Gynecol Oncol. 2020;157(2):379–85.
Decary S, Berne P-F, Nicolazzi C, Lefebvre A-M, Dabdoubi T, Cameron B, et al. Preclinical activity of SAR408701: a novel anti-CEACAM5-maytansinoid antibody-drug conjugate for the treatment of CEACAM5-positive epithelial tumors. Clin Cancer Res. 2020;26(24):6589–99.
Kahl BS, Hamadani M, Radford J, Carlo-Stella C, Caimi P, Reid E, et al. A phase I study of ADCT-402 (loncastuximabtesirine), a novel pyrrolobenzodiazepine-based antibody-drug conjugate, in relapsed/refractory B-cell non-Hodgkin lymphoma. Clin Cancer Res. 2019;25(23):6986–94.
Epperla N, Hamadani M. A new target for Hodgkin lymphoma – camidanlumab tesirine. CurrHematolMalig Rep [Internet]. 2021; Available from: https://pubmed.ncbi.nlm.nih.gov/33492560/
Anti-cancer ADC drugs: 3 design elements, 10 approved ADCs, multiple clinical trials [Internet]. Biochempeg.com. [cited 2021 Feb 16]. Available from: https://www.biochempeg.com/article/74.html
Beck A, Dumontet C, Joubert N. Les immunoconjuguésenoncologie: Les nouvellesstratégiesendéveloppement. Med Sci (Paris). 2019;35(12):1043–53.
Joubert N, Beck A, Dumontet C, Denevault-Sabourin C. Antibody–drug conjugates: the last decade. Pharmaceuticals (Basel). 2020;13(9):245.
Fda.gov. [cited 2021 Mar 20]. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/761121s000lbl.pdf
Fda.gov. [cited 2021 Mar 20]. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/761137s000lbl.pdf
Fda.gov. [cited 2021 Mar 20]. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/761115s000lbl.pdf
Fda.gov. [cited 2021 Mar 20]. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/761139s011lbl.pdf
Peters C, Brown S. Antibody-drug conjugates as novel anti-cancer chemotherapeutics. Biosci Rep. 2015;35(4):e00225–e00225.
Derakhshankhah H, Jafari S. Cell penetrating peptides: a concise review with emphasis on biomedical applications. Biomed Pharmacother. 2018;108:1090–6.
Tripathi PP, Arami H, Banga I, Gupta J, Gandhi S. Cell penetrating peptides in preclinical and clinical cancer diagnosis and therapy. Oncotarget. 2018;9(98):37252–67.
Pärn K, Eriste E, Langel Ü. The antimicrobial and antiviral applications of cell-penetrating peptides. Methods Mol Biol. 2015;1324:223–45.
Kristensen M, Birch D, Mørck NH. Applications and challenges for use of cell-penetrating peptides as delivery vectors for peptide and protein cargos. Int J Mol Sci. 2016;17(2):185.
Habault J, Poyet J-L. Recent advances in cell penetrating peptide-based anticancer therapies. Molecules. 2019;24(5):927.
Borrelli A, Tornesello AL, Tornesello ML, Buonaguro FM. Cell penetrating peptides as molecular carriers for anti-cancer agents. Molecules [Internet]. 2018;23(2). Available from: https://www.mdpi.com/resolver?pii=molecules23020295. Accessed 2 Oct 2021
Yu M, Li X, Huang X, Zhang J, Zhang Y, Wang H. New cell-penetrating peptide (KRP) with multiple physicochemical properties endows doxorubicin with tumor targeting and improves its therapeutic index. ACS Appl Mater Interfaces. 2019;11(2):2448–58.
Duan Z, Chen C, Qin J, Liu Q, Wang Q, Xu X, et al. Cell-penetrating peptide conjugates to enhance the antitumor effect of paclitaxel on drug-resistant lung cancer. Drug Deliv. 2017;24(1):752–64.
Izabela R, Jarosław R, Magdalena A, Piotr R, Ivan K. Transportan 10 improves the anticancer activity of cisplatin. NaunynSchmiedebergs Arch Pharmacol. 2016;389(5):485–97.
Zapadka KL, Becher FJ, Gomes Dos Santos AL, Jackson SE. Factors affecting the physical stability aggregation of peptide therapeutics. Interface Focus. 2017;7(6):20170030.
Su T, Yang H, Fan Q, Jia D, Tao Z, Wan L, et al. Enhancing the circulating half-life and the antitumor effects of a tumor-selective cytotoxic peptide by exploiting endogenous serum albumin as a drug carrier. Int J Pharm. 2016;499(1–2):195–204.
Ilangala AB, Lechanteur A, Fillet M, Piel G. Therapeutic peptides for chemotherapy: trends and challenges for advanced delivery systems. Eur J Pharm Biopharm. 2021;167:140–58.
Chambers CV. Cancer vaccines. Prim Care. 2011;38(4):703–15, viii–ix.
Cheng L, Wang Y, Du J. Human Papillomavirus vaccines: An updated review. Vaccines (Basel). 2020;8(3):391.
DeMaria PJ, Bilusic M. Cancer vaccines. Hematol Oncol Clin North Am. 2019;33(2):199–214.
Murias Henriquez C, Arkenau H-T, Dutoit V, Patrikidou A. Cancer vaccines. In: Arnouk H, editor. Cancer I.mmunotherapy and Biological Cancer Treatments. London, England: IntechOpen; 2019
Fda.gov. [cited 2021 Mar 20]. Available from: https://www.fda.gov/files/vaccines,%20blood%20&%20biologics/published/Package-Insert---Gardasil.pdf
Fda.gov. [cited 2021 Mar 20]. Available from: https://www.fda.gov/media/78013/download
Fda.gov. [cited 2021 Mar 20]. Available from: https://www.fda.gov/media/90064/download
Author information
Authors and Affiliations
Contributions
Asmita Yadav and Sakshi Singh carried out information retrieval, designing the tables and figures, compilation, and writing of the draft, Harmik Sohi analyzed the clinical trials information, and Shweta Dang conceptualized, supervised, and finalized the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare no conflict of interest. This submission is original work of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Asmita Yadav and Sakshi Singh contributed equally to this work
Rights and permissions
About this article
Cite this article
Yadav, A., Singh, S., Sohi, H. et al. Advances in Delivery of Chemotherapeutic Agents for Cancer Treatment. AAPS PharmSciTech 23, 25 (2022). https://doi.org/10.1208/s12249-021-02174-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-021-02174-9