Abstract
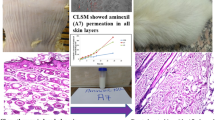
The first melatonergic antidepressant drug, agomelatine (AGM), is commonly used for controlling major depressive disorders. AGM suffers low (< 5%) oral bioavailability owing to the hepatic metabolism. The current work investigated the potential of low-frequency sonophoresis on enhancing transdermal delivery of AGM-loaded novasomes and, hence, bioavailability of AGM. Drug-loaded novasomes were developed using free fatty acid (stearic acid or oleic acid), surfactant (span 60 or span 80), and cholesterol via thin-film hydration technique. The systems (N1-N16) were assessed for zeta potential (ZP), particle size (PS), encapsulation efficiency (EE%), and drug percent released after 0.5 h (Q0.5 h) and 8 h (Q8h), drug-crystallinity, morphology, and ex vivo drug permeation. Skin pre-treatment with low-frequency ultrasound (LFU) waves, via N13-novasomal gel systems, was optimized to enhance ex vivo drug permeation. Influences of LFU mode (continuous or pulsed), duty cycle (50% or 100%), and application period (10 or 15 min) were optimized. The pharmacokinetics of the optimized system (N13-LFU-C4) was assessed in rabbits. N13 was the best achieved novasomal system with respect to PS (471.6 nm), ZP (− 63.6 mv), EE% (60.5%), Q0.5 h (27.8%), Q8h (83.9%), flux (15.5 μg/cm2/h), and enhancement ratio (6.9). N13-LFU-C4 was the optimized novasomal gel system (desirability; 0.997) which involves skin pre-treatment with LFU in a continuous mode, at 100% duty cycle, for 15 min. Compared to AGM dispersion, the significantly (P < 0.05) higher flux (26.7 μg/cm2/h), enhancement ratio (11.9), Cmax (118.23 ng/mL), and relative bioavailability (≈ 8.6 folds) could elucidate the potential of N13-LFU-C4 system in improving transdermal drug permeability and bioavailability.






Similar content being viewed by others
References
James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1789–858. https://doi.org/10.1016/S0140-6736(18)32279-7.
Zajecka JM. Clinical issues in long-term treatment with antidepressants. J Clin Psychiatry. 2000;61:20–5.
Millan MJ, Gobert A, Lejeune F, Dekeyne A, Newman-Tancredi A, Pasteau V, et al. The novel melatonin agonist agomelatine (S20098) is an antagonist at 5-hydroxytryptamine2c receptors, blockade of which enhances the activity of frontocortical dopaminergic and adrenergic pathways. J Pharmacol Exp Ther. 2003;306(3):954–64. https://doi.org/10.1124/jpet.103.051797.paradigm.
Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. 2018;391(10128):1357–66. https://doi.org/10.1016/S0140-6736(17)32802-7.
Said M, Elsayed I, Aboelwafa AA, Elshafeey AH. Transdermal agomelatine microemulsion gel: pyramidal screening, statistical optimization and in vivo bioavailability optimization and in vivo bioavailability. Drug Deliv. 2017;24(1):1159–69. https://doi.org/10.1080/10717544.2017.1365392.
Ita K. Recent progress in transdermal sonophoresis. Pharm Dev Technol. 2015;22(4):458–66. https://doi.org/10.3109/10837450.2015.1116566.
Zorec B, Préat V, Miklavčič D, Pavšelj N. Active enhancement methods for intra- and transdermal drug delivery: a review. Zdr Vestn. 2013;82(5):339–56.
Tawfik MA, Tadros MI, Mohamed MI, Nageeb E-H. Low-frequency versus high-frequency ultrasound-mediated transdermal delivery of agomelatine-loaded invasomes: development, optimization and in-vivo pharmacokinetic assessment. Int J Nanomedicine. 2020;15:8893–910. https://doi.org/10.2147/IJN.S283911.
Nair A, Vyas H, Shah J, Kumar A. Effect of permeation enhancers on the iontophoretic transport of metoprolol tartrate and the drug retention in skin. Drug Deliv. 2011;18(1):19–25. https://doi.org/10.3109/10717544.2010.509361.
Ammar HO, Mohamed MI, Tadros MI, Fouly AA. High frequency ultrasound mediated transdermal delivery of ondansetron hydrochloride employing bilosomal gel systems: ex-vivo and in-vivo characterization studies. J Pharm Investig. 2020;50:613–24. https://doi.org/10.1007/s40005-020-00491-y.
Alexander A, Dwivedi S, Ajazuddin, Giri TK, Saraf S, Saraf S, et al. Approaches for breaking the barriers of drug permeation through transdermal drug delivery. J Control Release. 2012;164(1):26–40. https://doi.org/10.1016/j.jconrel.2012.09.017.
Polat BE, Blankschtein D, Langer R. Low-frequency sonophoresis: application to the transdermal delivery of macromolecules and hydrophilic drugs. Expert Opin Drug Deliv. 2010;7(12):1415–32. https://doi.org/10.1517/17425247.2010.538679.
Boucaud A, Machet L, Arbeille B, Machet MC, Sournac M, Mavon A, et al. In vitro study of low-frequency ultrasound-enhanced transdermal transport of fentanyl and caffeine across human and hairless rat skin. Int J Pharm. 2001;228(1–2):69–77. https://doi.org/10.1016/S0378-5173(01)00820-1.
Boucaud A, Tessier L, Machet L, Vaillant L, Patat F. Transdermal delivery of insulin using low frequency ultrasound. In: Proceedings of the IEEE Ultrasonics Symposium. 2000. p. 1453–1456. doi:https://doi.org/10.1109/ultsym.2000.921597.
Langer M, Lewis S, Fleshman S, Lewis G. “SonoBandage” a transdermal ultrasound drug delivery system for peripheral neuropathy. Proc Meet Acoust. 2013;19(1). https://doi.org/10.1121/1.4801417.
Aldwaikat M, Alarjah M. Investigating the sonophoresis effect on the permeation of diclofenac sodium using 3D skin equivalent. Ultrason Sonochem. 2015;22:580–7. https://doi.org/10.1016/j.ultsonch.2014.02.017.
Polat BE, Hart D, Langer R, Blankschtein D. Ultrasound-mediated transdermal drug delivery: mechanisms, scope, and emerging trends. J Control Release. 2011;152(3):330–48. https://doi.org/10.1016/j.jconrel.2011.01.006.
Singh A, Malviya R, Sharma PK. Novasome-A breakthrough in pharmaceutical technology a review article. Adv Biol Res (Rennes). 2011;5(4):184–9.
Said M, Elsayed I, Aboelwafa AA, Elshafeey AH. A novel concept of overcoming the skin barrier using augmented liquid nanocrystals: Box-Behnken optimization, ex vivo and in vivo evaluation. Colloids Surf B Biointerfaces. 2018;170:258–65. https://doi.org/10.1016/j.colsurfb.2018.06.025.
Shinde M, Bali N, Rathod S, Karemore M, Salve P. Effect of binary combinations of solvent systems on permeability profiling of pure agomelatine across rat skin: a comparative study with statistically optimized polymeric nanoparticles. Drug Dev Ind Pharm. 2020;46:826–45. https://doi.org/10.1080/03639045.2020.1757697.
Abd-Elal RMA, Shamma RN, Rashed HM, Bendas ER. Trans-nasal zolmitriptan novasomes: in-vitro preparation, optimization and in-vivo evaluation of brain targeting efficiency. Drug Deliv. 2016;23(9):3374–86. https://doi.org/10.1080/10717544.2016.1183721.
Tscharnuter W. Photon correlation spectroscopy in particle sizing. In: Meyers RA, editors. Encyclopedia of Analytical Chemistry. Chichester: John Wiley & Sons Ltd; 2000. p. 5469–5485. https://doi.org/10.1002/9780470027318.a1512.
Kassem MA, Aboul-Einien MH, El Taweel MM. Dry gel containing optimized felodipine-loaded transferosomes: a promising transdermal delivery system to enhance drug bioavailability. AAPS PharmSciTech. 2018;19(5):2155–73. https://doi.org/10.1208/s12249-018-1020-5.
Fatouh AM, Elshafeey AH, Abdelbary A. Agomelatine-based in situ gels for brain targeting via the nasal route: statistical optimization, in vitro, and in vivo evaluation. Drug Deliv. 2017;24(1):1077–85. https://doi.org/10.1080/10717544.2017.1357148.
Duarah S, Durai RD, Narayanan VHB. Nanoparticle-in-gel system for delivery of vitamin C for topical application. Drug Deliv Transl Res. 2017;7(5):750–60. https://doi.org/10.1007/s13346-017-0398-z.
Balzus B, Colombo M, Sahle FF, Zoubari G, Staufenbiel S, Bodmeier R. Comparison of different in vitro release methods used to investigate nanocarriers intended for dermal application. Int J Pharm. 2016;513(1–2):247–54. https://doi.org/10.1016/j.ijpharm.2016.09.033.
Tawfik MA, Tadros MI, Mohamed MI. Lipomers (lipid-polymer hybrid particles) of vardenafil hydrochloride: a promising dual platform for modifying the drug release rate and enhancing its oral bioavailability. AAPS PharmSciTech. 2018;19(8):3650–60. https://doi.org/10.1208/s12249-018-1191-0.
Ammar HO, Mohamed MI, Tadros MI, Fouly AA. Transdermal delivery of ondansetron hydrochloride via bilosomal systems: in vitro, ex vivo, and in vivo characterization studies. AAPS PharmSciTech. 2018;19(5):2276–87. https://doi.org/10.1208/s12249-018-1019-y.
Fahmy AM, El-Setouhy DA, Ibrahim AB, Habib BA, Tayel SA, Bayoumi NA. Penetration enhancer-containing spanlastics (PECSs) for transdermal delivery of haloperidol: in vitro characterization, ex vivo permeation and in vivo biodistribution studies. Drug Deliv. 2018;25(1):12–22. https://doi.org/10.1080/10717544.2017.1410262.
Aziz DE, Abdelbary AA, Elassasy AI. Investigating superiority of novel bilosomes over niosomes in the transdermal delivery of diacerein: in vitro characterization, ex vivo permeation and in vivo skin deposition study. J Liposome Res. 2019;29(1):73–85. https://doi.org/10.1080/08982104.2018.1430831.
Ammar HO, Tadros MI, Salama NM, Ghoneim AM. Ethosome-derived invasomes as a potential transdermal delivery system for vardenafil hydrochloride : development, optimization and application of physiologically based pharmacokinetic modeling in adults and geriatrics. Int J Nanomedicine. 2020;15:5671–85. https://doi.org/10.2147/IJN.S261764.
Skelly JP, Shah VP, Maibach HI, Guy RH, Wester RC, Flynn G, et al. FDA and AAPS report of the workshop on principles and practices of in vitro percutaneous penetration studies: relevance to bioavailability and bioequivalence. Pharm Res. 1987;4(3):265–7. https://doi.org/10.1023/A:1016428716506.
Shinde M, Salve P, Rathod S. Development and evaluation of nanoparticles based transdermal patch of agomelatine for the treatment of depression. J Drug Deliv Ther. 2019;9 supple 4:126–144. https://doi.org/10.22270/jddt.v9i4-s.3229.
Patil RR, Gaikwad RV, Samad A, Devarajan PV. Role of lipids in enhancing splenic uptake of polymer-lipid (LIPOMER) nanoparticles. J Biomed Nanotechnol. 2008;4(3):359–66. https://doi.org/10.1166/jbn.2008.320.
Lingan MA, Sathali AA, Kumar MRV, Gokila A. Formulation and evaluation of topical drug delivery system containing clobetasol propionate niosomes. Sci Rev Chem Commun. 2011;1(1):7–17.
Abdelkader H, Ismail S, Kamal A, Alany RG. Preparation of niosomes as an ocular delivery system for naltrexone hydrochloride: physicochemical characterization. Pharmazie. 2010;65(11):811–7. https://doi.org/10.1691/ph.2010.0138.
Nowroozi F, Almasi A, Javidi J, Haeri A, Dadashzadeh S. Effect of surfactant type, cholesterol content and various downsizing methods on the particle size of niosomes. Iran J Pharm Res. 2018;17(Special Issue 2):1–11. https://doi.org/10.22037/ijpr.2018.2368.
Kanicky JR, Shah DO. Effect of degree, type, and position of unsaturation on the pKa of long-chain fatty acids. J Colloid Interface Sci. 2002;256(1):201–7. https://doi.org/10.1006/jcis.2001.8009.
Yoshioka T, Sternberg B, Florence AT. Preparation and properties of vesicles (niosomes) of sorbitan monoesters (Span 20, 40, 60 and 80) and a sorbitan triester (Span 85). Int J Pharm. 1994;105:1–6. https://doi.org/10.1016/0378-5173(94)90228-3.
Abdelkader H, Alani AWG, Alany RG. Recent advances in non-ionic surfactant vesicles (niosomes): self-assembly, fabrication, characterization, drug delivery applications and limitations. Drug Deliv. 2014;21(2):87–100. https://doi.org/10.3109/10717544.2013.838077.
Al-Mahallawi AM, Abdelbary AA, Aburahma MH. Investigating the potential of employing bilosomes as a novel vesicular carrier for transdermal delivery of tenoxicam. Int J Pharm. 2015;485(1–2):329–40. https://doi.org/10.1016/j.ijpharm.2015.03.033.
Makino K, Yamada T, Kimura M, Oka T, Ohshima H, Kondo T. Temperature- and ionic strength-induced conformational changes in the lipid head group region of liposomes as suggested by zeta potential data. Biophys Chem. 1991;41(2):175–83. https://doi.org/10.1016/0301-4622(91)80017-L.
Fatouh AM, Elshafeey AH, Abdelbary A. Intranasal agomelatine solid lipid nanoparticles to enhance brain delivery: Formulation, optimization and in vivo pharmacokinetics. Drug Des Devel Ther. 2017;11:1815–25. https://doi.org/10.2147/DDDT.S102500.
Li Y, Wong HL, Shuhendler AJ, Rauth AM, Wu XY. Molecular interactions, internal structure and drug release kinetics of rationally developed polymer-lipid hybrid nanoparticles. J Control Release. 2008;128(1):60–70. https://doi.org/10.1016/j.jconrel.2008.02.014.
Lee KL, Zhou Y. Quantitative evaluation of sonophoresis efficiency and its dependence on sonication parameters and particle size. J Ultrasound Med. 2015;34(3):519–26. https://doi.org/10.7863/ultra.34.3.519.
Pereira TA, Ramos DN, Lopez RFV. Hydrogel increases localized transport regions and skin permeability during low frequency ultrasound treatment. Sci Rep. 2017;7:e44236. https://doi.org/10.1038/srep44236.
Huang B, Dong WJ, Yang GY, Wang W, Ji CH, Zhou FN. Dendrimer-coupled sonophoresis-mediated transdermal drug-delivery system for diclofenac. Drug Des Devel Ther. 2015;9:3867–76. https://doi.org/10.2147/DDDT.S75702.
Mabrouk AA., Tadros MI.,Refaie WM. Improving the efficacy of Cyclooxegenase-2 inhibitors in the management of oral cancer: insights into the implementation of nanotechnology and mucoadhesion. J Drug Del. Sci. Technol. 2021;61:Article number 102240.
Mitragotri S, Kost J. Low-frequency sonophoresis: a review. Adv Drug Deliv Rev. 2004;56(5):589–601. https://doi.org/10.1016/j.addr.2003.10.024.
Mitragotri S, Ray D, Farrell J, Tang H, Yu B, Kost J, et al. Synergistic effect of low-frequency ultrasound and sodium lauryl sulfate on transdermal transport. J Pharm Sci. 2000;89(7):892–900. https://doi.org/10.1002/1520-6017(200007)89:7%3c892::AID-JPS6%3e3.0.CO;2-V.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to this work.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tawfik, M.A., Mohamed, M.I., Tadros, M.I. et al. Low-Frequency Sonophoresis as an Active Approach to Potentiate the Transdermal Delivery of Agomelatine-Loaded Novasomes: Design, Optimization, and Pharmacokinetic Profiling in Rabbits. AAPS PharmSciTech 22, 261 (2021). https://doi.org/10.1208/s12249-021-02147-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-021-02147-y