Abstract
With the limitation of solubility and dissolution rate of insoluble drugs, following oral administration, they would rifely prove poor and volatile bioavailability, which may fail to realize its therapeutic value. The drug nanocrystals are perceived as effective tactic for oral administration of insoluble drugs attributes to possess many prominent properties such as elevating dissolution rate and saturation solubility, high drug loading capacity, and improving oral bioavailability. Based on these advantages, the application of nanocrystals in oral drug delivery has acquired significant achievement, and so far more than 20 products of drug nanocrystals have been confirmed in the market. However, the oral absorption of drug nanocrystals is still facing huge challenges due to the limitation of many factors. Intrinsic properties of the drugs and complex physiological environment of the intestinal tract are the two most important factors affecting the oral bioavailability of drugs. In addition, the research on the multi-aspect mechanisms of nanocrystals promoting gastrointestinal absorption and bioavailability has been gradually deepened. In this review, we summarized recent advances of the nanocrystals delivered orally, and provided an overview to the research progress for crossing the intestinal tract transport mechanisms of the nanocrystals by some new research techniques. Meanwhile, the factors relevant to the transport of drug nanocrystals were also elaborated in detail.

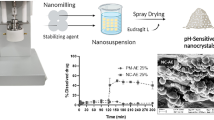
Graphical Abstract







Similar content being viewed by others
References
Pawar VK, Singh Y, Meher JG, Gupta S, Chourasia MK. Engineered nanocrystal technology: in-vivo fate, targeting and applications in drug delivery. J Control Release. 2014;183:51–66. https://doi.org/10.1016/j.jconrel.2014.03.030 Epub 2014 Mar 23.
Guo M, Fu Q, Wu C, Guo Z, Li M, Sun J, et al. Rod shaped nanocrystals exhibit superior in vitro dissolution and in vivo bioavailability over spherical like nanocrystals: a case study of lovastatin. Colloids Surf B: Biointerfaces. 2015;128:410–8. https://doi.org/10.1016/j.colsurfb.2015.02.039 Epub 2015 Feb 25.
Schittny A, Philipp-Bauer S, Detampel P, Huwyler J, Puchkov M. Mechanistic insights into effect of surfactants on oral bioavailability of amorphous solid dispersions. J Control Release. 2020;320:214–25. https://doi.org/10.1016/j.jconrel.2020.01.031 Epub 2020 Jan 21.
Plourde K, Derbali RM, Desrosiers A, Dubath C, Vallée-Bélisle A, Leblond J. Aptamer-based liposomes improve specific drug loading and release. J Control Release. 2017;251:82–91. https://doi.org/10.1016/j.jconrel.2017.02.026 Epub 2017 Feb 24.
Diwan R, Ravi PR, Pathare NS, Aggarwal V. Pharmacodynamic, pharmacokinetic and physical characterization of cilnidipine loaded solid lipid nanoparticles for oral delivery optimized using the principles of design of experiments. Colloids Surf B: Biointerfaces. 2020;193:111073. https://doi.org/10.1016/j.colsurfb.2020.111073 Epub 2020 Apr 24.
Cui B, Lv Y, Gao F, Wang C, Zeng Z, Wang Y, et al. Improving abamectin bioavailability via nanosuspension constructed by wet milling technique. Pest Manag Sci. 2019;75(10):2756–64. https://doi.org/10.1002/ps.5386 Epub 2019 Apr 1.
Yuan H, Li X, Zhang C, Pan W, Liang Y, Chen Y, et al. Nanosuspensions as delivery system for gambogenic acid: characterization and in vitro/in vivo evaluation. Drug Deliv. 2016;23(8):2772–9. https://doi.org/10.3109/10717544.2015.1077294 Epub 2015 Aug 18.
Jinno J, Kamada N, Miyake M, Yamada K, Mukai T, Odomi M, et al. Effect of particle size reduction on dissolution and oral absorption of a poorly water-soluble drug, cilostazol, in beagle dogs. J Control Release. 2006;111(1-2):56–64. https://doi.org/10.1016/j.jconrel.2005.11.013 Epub 2006 Jan 10.
Sun W, Ni R, Zhang X, Li LC, Mao S. Spray drying of a poorly water-soluble drug nanosuspension for tablet preparation: formulation and process optimization with bioavailability evaluation. Drug Dev Ind Pharm. 2015;41(6):927–33. https://doi.org/10.3109/03639045.2014.914528 Epub 2014 May 2.
Mohammad IS, Hu H, Yin L, He W. Drug nanocrystals: fabrication methods and promising therapeutic applications. Int J Pharm. 2019;562:187–202. https://doi.org/10.1016/j.ijpharm.2019.02.045 Epub 2019 Mar 6.
Lai SK, Wang YY, Wirtz D, Hanes J. Micro- and macrorheology of mucus. Adv Drug Deliv Rev. 2009;61(2):86–100. https://doi.org/10.1016/j.addr.2008.09.012 Epub 2009 Jan 3.
Nagarwal RC, Kumar R, Dhanawat M, Das N, Pandit JK. Nanocrystal technology in the delivery of poorly soluble drugs: an overview. Curr Drug Deliv. 2011;8(4):398–406. https://doi.org/10.2174/156720111795767988.
Chen Y, Li T. Cellular uptake mechanism of paclitaxel nanocrystals determined by confocal imaging and kinetic measurement. AAPS J. 2015;17(5):1126–34. https://doi.org/10.1208/s12248-015-9774-0 Epub 2015 Jun 24.
Beloqui A, des Rieux A, Préat V. Mechanisms of transport of polymeric and lipidic nanoparticles across the intestinal barrier. Adv Drug Deliv Rev. 2016;106(Pt B):242–55. https://doi.org/10.1016/j.addr.2016.04.014 Epub 2016 Apr 23.
Win KY, Feng SS. Effects of particle size and surface coating on cellular uptake of polymeric nanoparticles for oral delivery of anticancer drugs. Biomaterials. 2005;26(15):2713–22. https://doi.org/10.1016/j.biomaterials.2004.07.050.
Sugano K, Kansy M, Artursson P, Avdeef A, Bendels S, Di L, et al. Coexistence of passive and carrier-mediated processes in drug transport. Nat Rev Drug Discov. 2010;9(8):597–614. https://doi.org/10.1038/nrd3187.
Fröhlich E, Roblegg E. Oral uptake of nanoparticles: human relevance and the role of in vitro systems. Arch Toxicol. 2016;90(10):2297–314. https://doi.org/10.1007/s00204-016-1765-0 Epub 2016 Jun 25.
Yu M, Yang Y, Zhu C, Guo S, Gan Y. Advances in the transepithelial transport of nanoparticles. Drug Discov Today. 2016;21(7):1155–61. https://doi.org/10.1016/j.drudis.2016.05.007 Epub 2016 May 16.
Creton C, Ciccotti M. Fracture and adhesion of soft materials: a review. Rep Prog Phys. 2016;79(4):046601. https://doi.org/10.1088/0034-4885/79/4/046601 Epub 2016 Mar 23.
Mackie AR, Goycoolea FM, Menchicchi B, Caramella CM, Saporito F, Lee S, et al. Innovative methods and applications in mucoadhesion research. Macromol Biosci. 2017;17(8). https://doi.org/10.1002/mabi.201600534 Epub 2017 Apr 5.
Leal J, Smyth HDC, Ghosh D. Physicochemical properties of mucus and their impact on transmucosal drug delivery. Int J Pharm. 2017;532(1):555–72. https://doi.org/10.1016/j.ijpharm.2017.09.018 Epub 2017 Sep 14.
Roger E, Lagarce F, Garcion E, Benoit JP. Biopharmaceutical parameters to consider in order to alter the fate of nanocarriers after oral delivery. Nanomedicine (London). 2010;5(2):287–306. https://doi.org/10.2217/nnm.09.110.
Khutoryanskiy VV. Beyond PEGylation: alternative surface-modification of nanoparticles with mucus-inert biomaterials. Adv Drug Deliv Rev. 2018;124:140–9. https://doi.org/10.1016/j.addr.2017.07.015 Epub 2017 Jul 20.
Mei L, Zhang Z, Zhao L, Huang L, Yang XL, Tang J, et al. Pharmaceutical nanotechnology for oral delivery of anticancer drugs. Adv Drug Deliv Rev. 2013;65(6):880–90. https://doi.org/10.1016/j.addr.2012.11.005 Epub 2012 Dec 7.
Maisel K, Ensign L, Reddy M, Cone R, Hanes J. Effect of surface chemistry on nanoparticle interaction with gastrointestinal mucus and distribution in the gastrointestinal tract following oral and rectal administration in the mouse. J Control Release. 2015;197:48–57. https://doi.org/10.1016/j.jconrel.2014.10.026 Epub 2014 Nov 4.
Russo P, Stigliani M, Prota L, Auriemma G, Crescenzi C, Porta A, et al. Gentamicin and leucine inhalable powder: what about antipseudomonal activity and permeation through cystic fibrosis mucus? Int J Pharm. 2013;440(2):250–5. https://doi.org/10.1016/j.ijpharm.2012.05.077 Epub 2012 Jun 7.
Guo M, Wei M, Li W, Guo M, Guo C, Ma M, et al. Impacts of particle shapes on the oral delivery of drug nanocrystals: mucus permeation, transepithelial transport and bioavailability. J Control Release. 2019;307:64–75. https://doi.org/10.1016/j.jconrel.2019.06.015 Epub 2019 Jun 15.
Xie Y, Chen Z, Su R, Li Y, Qi J, Wu W, et al. Preparation and optimization of amorphous ursodeoxycholic acid nano-suspensions by nanoprecipitation based on acid-base neutralization for enhanced dissolution. Curr Drug Deliv. 2017;14(4):483–91. https://doi.org/10.2174/1567201813666160902152122.
Tu L, Cheng M, Sun Y, Fang Y, Liu J, Liu W, et al. Fabrication of ultra-small nanocrystals by formation of hydrogen bonds: In vitro and in vivo evaluation. Int J Pharm. 2020;573:118730. https://doi.org/10.1016/j.ijpharm.2019.118730 Epub 2019 Nov 6.
Stamatovic SM, Keep RF, Kunkel SL, Andjelkovic AV. Potential role of MCP-1 in endothelial cell tight junction ‘opening’: signaling via Rho and Rho kinase. J Cell Sci. 2003;116(Pt 22):4615–28. https://doi.org/10.1242/jcs.00755.
Chen MC, Mi FL, Liao ZX, Hsiao CW, Sonaje K, Chung MF, et al. Recent advances in chitosan-based nanoparticles for oral delivery of macromolecules. Adv Drug Deliv Rev. 2013;65(6):865–79. https://doi.org/10.1016/j.addr.2012.10.010 Epub 2012 Nov 15.
Li H, Zhou J, Zhao J, Li Y, Lu K. Synthesis of cellulose nanocrystals-armored fluorinated polyacrylate latexes via Pickering emulsion polymerization and their film properties. Colloids Surf B: Biointerfaces. 2020;192:111071. https://doi.org/10.1016/j.colsurfb.2020.111071 Epub ahead of print.
Sharma S, Verma A, Pandey G, Mittapelly N, Mishra PR. Investigating the role of pluronic-g-cationic polyelectrolyte as functional stabilizer for nanocrystals: impact on Paclitaxel oral bioavailability and tumor growth. Acta Biomater. 2015;26:169–83. https://doi.org/10.1016/j.actbio.2015.08.005 Epub 2015 Aug 8.
O’ Neill MJ, Guo J, Byrne C, Darcy R, O’ Driscoll CM. Mechanistic studies on the uptake and intracellular trafficking of novel cyclodextrin transfection complexes by intestinal epithelial cells. Int J Pharm. 2011;413(1-2):174–83. https://doi.org/10.1016/j.ijpharm.2011.04.021 Epub 2011 Apr 16.
Duncan R, Richardson SC. Endocytosis and intracellular trafficking as gateways for nanomedicine delivery: opportunities and challenges. Mol Pharm. 2012;9(9):2380–402. https://doi.org/10.1021/mp300293n Epub 2012 Aug 20.
Gamboa JM, Leong KW. In vitro and in vivo models for the study of oral delivery of nanoparticles. Adv Drug Deliv Rev. 2013;65(6):800–10. https://doi.org/10.1016/j.addr.2013.01.003 Epub 2013 Feb 13.
Conner SD, Schmid SL. Regulated portals of entry into the cell. Nature. 2003;422(6927):37–44. https://doi.org/10.1038/nature01451.
Ruiz de Garibay AP, Solinís Aspiazu MÁ, Rodríguez Gascón A, Ganjian H, Fuchs R. Role of endocytic uptake in transfection efficiency of solid lipid nanoparticles-based nonviral vectors. J Gene Med. 2013;15(11-12):427–40. https://doi.org/10.1002/jgm.2749.
Guo J, O’Mahony AM, Cheng WP, O’Driscoll CM. Amphiphilic polyallylamine based polymeric micelles for siRNA delivery to the gastrointestinal tract: in vitro investigations. Int J Pharm. 2013;447(1-2):150–7. https://doi.org/10.1016/j.ijpharm.2013.02.050 Epub 2013 Mar 1.
Deng F, Zhang H, Wang X, Zhang Y, Hu H, Song S, et al. Transmembrane pathways and mechanisms of rod-like paclitaxel nanocrystals through MDCK polarized monolayer. ACS Appl Mater Interfaces. 2017;9(7):5803–16. https://doi.org/10.1021/acsami.6b15151 Epub 2017 Feb 9.
Wu L, Bai Y, Liu M, Li L, Shan W, Zhang Z, et al. Transport mechanisms of butyrate modified nanoparticles: insight into “easy entry, hard transcytosis” of active targeting system in oral administration. Mol Pharm. 2018;15(9):4273–83. https://doi.org/10.1021/acs.molpharmaceut.8b00713 Epub 2018 Aug 23.
Neutra MR, Frey A, Kraehenbuhl JP. Epithelial M cells: gateways for mucosal infection and immunization. Cell. 1996sss;86(3):345–8. https://doi.org/10.1016/s0092-8674(00)80106-3.
Jung F, Nothnagel L, Gao F, Thurn M, Vogel V, Wacker MG. A comparison of two biorelevant in vitro drug release methods for nanotherapeutics based on advanced physiologically-based pharmacokinetic modelling. Eur J Pharm Biopharm. 2018;127:462–70. https://doi.org/10.1016/j.ejpb.2018.03.010 Epub 2018 Mar 27.
Singh B, Maharjan S, Jiang T, Kang SK, Choi YJ, Cho CS. Combinatorial approach of antigen delivery using M cell-homing peptide and mucoadhesive vehicle to enhance the efficacy of oral vaccine. Mol Pharm. 2015;12(11):3816–28. https://doi.org/10.1021/acs.molpharmaceut.5b00265 Epub 2015 Oct 2.
Patel K, Patil A, Mehta M, Gota V, Vavia P. Oral delivery of paclitaxel nanocrystal (PNC) with a dual Pgp-CYP3A4 inhibitor: preparation, characterization and antitumor activity. Int J Pharm. 2014;472(1-2):214–23. https://doi.org/10.1016/j.ijpharm.2014.06.031 Epub 2014 Jun 20.
Na YG, Pham TMA, Byeon JJ, Kim MK, Han MG, Baek JS, et al. Development and evaluation of TPGS/PVA-based nanosuspension for enhancing dissolution and oral bioavailability of ticagrelor. Int J Pharm. 2020;581:119287. https://doi.org/10.1016/j.ijpharm.2020.119287 Epub 2020 Mar 31.
Xiong W, Sang W, Linghu KG, Zhong ZF, Cheang WS, Li J, et al. Dual-functional Brij-S20-modified nanocrystal formulation enhances the intestinal transport and oral bioavailability of berberine. Int J Nanomedicine. 2018;13:3781–93. https://doi.org/10.2147/IJN.S163763.
Chaudhary S, Garg T, Murthy RS, Rath G, Goyal AK. Recent approaches of lipid-based delivery system for lymphatic targeting via oral route. J Drug Target. 2014;22(10):871–82. https://doi.org/10.3109/1061186X.2014.950664 Epub 2014 Aug 22.
Yin Y, Deng H, Wu K, He B, Dai W, Zhang H, et al. A multiaspect study on transcytosis mechanism of sorafenib nanogranules engineered by high-gravity antisolvent precipitation. J Control Release. 2020;323:600–12. https://doi.org/10.1016/j.jconrel.2020.04.008 Epub 2020 Apr 9.
Zhang G, Wang Y, Zhang Z, He Z, Liu Y, Fu Q. FRET imaging revealed that nanocrystals enhanced drug oral absorption by dissolution rather than endocytosis: a case study of coumarin 6. J Control Release. 2021;332:225–32. https://doi.org/10.1016/j.jconrel.2021.02.025 Epub ahead of print.
Fu Q, Sun J, Ai X, Zhang P, Li M, Wang Y, et al. Nimodipine nanocrystals for oral bioavailability improvement: role of mesenteric lymph transport in the oral absorption. Int J Pharm. 2013;448(1):290–7. https://doi.org/10.1016/j.ijpharm.2013.01.065 Epub 2013 Feb 4.
Miao X, Li Y, Wang X, Lee SM, Zheng Y. Transport mechanism of coumarin 6 nanocrystals with two particle sizes in MDCKII monolayer and larval zebrafish. ACS Appl Mater Interfaces. 2016;8(20):12620–30. https://doi.org/10.1021/acsami.6b01680 Epub 2016 May 16.
Chen C, Wang L, Cao F, Miao X, Chen T, Chang Q, et al. Formulation of 20(S)-protopanaxadiol nanocrystals to improve oral bioavailability and brain delivery. Int J Pharm. 2016;497(1-2):239–47. https://doi.org/10.1016/j.ijpharm.2015.12.014 Epub 2015 Dec 8.
Cheng M, Yuan F, Liu J, Liu W, Feng J, Jin Y, et al. Fabrication of fine puerarin nanocrystals by Box-Behnken design to enhance intestinal absorption. AAPS PharmSciTech. 2020;21(3):90. https://doi.org/10.1208/s12249-019-1616-4.
Jain S, Reddy VA, Arora S, Patel K. Development of surface stabilized candesartan cilexetil nanocrystals with enhanced dissolution rate, permeation rate across CaCo-2, and oral bioavailability. Drug Deliv Transl Res. 2016;6(5):498–510. https://doi.org/10.1007/s13346-016-0297-8.
He Y, Xia DN, Li QX, Tao JS, Gan Y, Wang C. Enhancement of cellular uptake, transport and oral absorption of protease inhibitor saquinavir by nanocrystal formulation. Acta Pharmacol Sin. 2015;36(9):1151–60. https://doi.org/10.1038/aps.2015.53 Epub 2015 Aug 10.
Malamatari M, Taylor KMG, Malamataris S, Douroumis D, Kachrimanis K. Pharmaceutical nanocrystals: production by wet milling and applications. Drug Discov Today. 2018;23(3):534–47. https://doi.org/10.1016/j.drudis.2018.01.016 Epub 2018 Jan 8.
Rabinow B, Kipp J, Papadopoulos P, Wong J, Glosson J, Gass J, et al. Itraconazole IV nanosuspension enhances efficacy through altered pharmacokinetics in the rat. Int J Pharm. 2007;339(1-2):251–60. https://doi.org/10.1016/j.ijpharm.2007.02.030 Epub 2007 Mar 3.
Wang J, Muhammad N, Li T, Wang H, Liu Y, Liu B, et al. Hyaluronic acid-coated camptothecin nanocrystals for targeted drug delivery to enhance anticancer efficacy. Mol Pharm. 2020;17(7):2411–25. https://doi.org/10.1021/acs.molpharmaceut.0c00161 Epub 2020 Jun 4.
Ng AN, de Jong-Curtain TA, Mawdsley DJ, White SJ, Shin J, Appel B, et al. Formation of the digestive system in zebrafish: III. Intestinal epithelium morphogenesis. Dev Biol. 2005;286(1):114–35. https://doi.org/10.1016/j.ydbio.2005.07.013.
Hussain N, Jaitley V, Florence AT. Recent advances in the understanding of uptake of microparticulates across the gastrointestinal lymphatics. Adv Drug Deliv Rev. 2001;50(1-2):107–42. https://doi.org/10.1016/s0169-409x(01)00152-1.
Zhang Q, He S, Kuang G, Liu S, Lu H, Li X, et al. Morphology tunable and acid-sensitive dextran-doxorubicin conjugate assemblies for targeted cancer therapy. J Mater Chem B. 2020;8(31):6898–904. https://doi.org/10.1039/d0tb00746c Epub 2020 May 13.
Na YG, Pham TMA, Byeon JJ, Kim MK, Han MG, Baek JS, et al. Development and evaluation of TPGS/PVA-based nanosuspension for enhancing dissolution and oral bioavailability of ticagrelor. Int J Pharm. 2020;581:119287. https://doi.org/10.1016/j.ijpharm.2020.119287 Epub 2020 Mar 31.
Ren T, Wang Q, Xu Y, Cong L, Gou J, Tao X, et al. Enhanced oral absorption and anticancer efficacy of cabazitaxel by overcoming intestinal mucus and epithelium barriers using surface polyethylene oxide (PEO) decorated positively charged polymer-lipid hybrid nanoparticles. J Control Release. 2018;269:423–38. https://doi.org/10.1016/j.jconrel.2017.11.015 Epub 2017 Nov 11.
Liu Y, Jiang Z, Hou X, Xie X, Shi J, Shen J, et al. Functional lipid polymeric nanoparticles for oral drug delivery: rapid mucus penetration and improved cell entry and cellular transport. Nanomedicine. 2019;21:102075. https://doi.org/10.1016/j.nano.2019.102075 Epub 2019 Aug 1.
Crater JS, Carrier RL. Barrier properties of gastrointestinal mucus to nanoparticle transport. Macromol Biosci. 2010;10(12):1473–83. https://doi.org/10.1002/mabi.201000137 Epub 2010 Sep 20.
Zhu ZJ, Posati T, Moyano DF, Tang R, Yan B, Vachet RW, et al. The interplay of monolayer structure and serum protein interactions on the cellular uptake of gold nanoparticles. Small. 2012;8(17):2659–63. https://doi.org/10.1002/smll.201200794 Epub 2012 Jun 25.
Ueda K, Higashi K, Yamamoto K, Moribe K. In situ molecular elucidation of drug supersaturation achieved by nano-sizing and amorphization of poorly water-soluble drug. Eur J Pharm Sci. 2015;77:79–89. https://doi.org/10.1016/j.ejps.2015.05.027 Epub 2015 May 30.
Lai SK, Wang YY, Hanes J. Mucus-penetrating nanoparticles for drug and gene delivery to mucosal tissues. Adv Drug Deliv Rev. 2009;61(2):158–71. https://doi.org/10.1016/j.addr.2008.11.002 Epub 2008 Dec 13.
Zhang YL, Zhang ZH, Jiang TY, Ayman-Waddad, Jing-Li LHX, et al. Cell uptake of paclitaxel solid lipid nanoparticles modified by cell-penetrating peptides in A549 cells. Pharmazie. 2013;68(1):47–53.
Yin Y, Chen D, Qiao M, Lu Z, Hu H. Preparation and evaluation of lectin-conjugated PLGA nanoparticles for oral delivery of thymopentin. J Control Release. 2006;116(3):337–45. https://doi.org/10.1016/j.jconrel.2006.09.015 Epub 2006 Oct 3.
Oshi MA, Lee J, Naeem M, Hasan N, Kim J, Kim HJ, et al. Curcumin nanocrystal/pH-responsive polyelectrolyte multilayer core-shell nanoparticles for inflammation-targeted alleviation of ulcerative colitis. Biomacromolecules. 2020;21(9):3571–81. https://doi.org/10.1021/acs.biomac.0c00589 Epub 2020 Aug 17.
Ding Z, Liu G, Hu J. Ratiometric fluorescent mapping of pH and glutathione dictates intracellular transport pathways of micellar nanoparticles. Biomacromolecules. 2020;21(8):3436–46. https://doi.org/10.1021/acs.biomac.0c00872 Epub 2020 Jul 29.
Li PP, Yan Y, Zhang HT, Cui SH, Wang CH, Wei W, et al. Biological activities of siRNA-loaded lanthanum phosphate nanoparticles on colorectal cancer. J Control Release. 2020;328:45–58. https://doi.org/10.1016/j.jconrel.2020.08.027 Epub 2020 Aug 27.
Pereira C, Araújo F, Barrias CC, Granja PL, Sarmento B. Dissecting stromal-epithelial interactions in a 3D in vitro cellularized intestinal model for permeability studies. Biomaterials. 2015;56:36–45. https://doi.org/10.1016/j.biomaterials.2015.03.054 Epub 2015 Apr 15.
Sheng H, Zhang Y, Nai J, Wang S, Dai M, Lin GZ, et al. Preparation of oridonin nanocrystals and study of their endocytosis and transcytosis behaviours on MDCK polarized epithelial cells. Pharm Biol. 2020;58(1):518–27. https://doi.org/10.1080/13880209.2020.1767160.
Lu Y, Lv Y, Li T. Hybrid drug nanocrystals. Adv Drug Deliv Rev. 2019;143:115–33. https://doi.org/10.1016/j.addr.2019.06.006 Epub 2019 Jun 26.
Luo J, Xie Z, Lam JW, Cheng L, Chen H, Qiu C, et al. Aggregation-induced emission of 1-methyl-1,2,3,4,5-pentaphenylsilole. Chem Commun (Camb). 2001;(18):1740–1. https://doi.org/10.1039/b105159h.
Shen C, Yang Y, Shen B, Xie Y, Qi J, Dong X, et al. Self-discriminating fluorescent hybrid nanocrystals: efficient and accurate tracking of translocation via oral delivery. Nanoscale. 2017;10(1):436–50. https://doi.org/10.1039/c7nr06052a.
Wagh A, Jyoti F, Mallik S, Qian S, Leclerc E, Law B. Polymeric nanoparticles with sequential and multiple FRET cascade mechanisms for multicolor and multiplexed imaging. Small. 2013;9(12):2129–39. https://doi.org/10.1002/smll.201202655 Epub 2013 Jan 29.
Xiong S, Liu W, Li D, Chen X, Liu F, Yuan D, et al. Oral delivery of puerarin nanocrystals to improve brain accumulation and anti-Parkinsonian efficacy. Mol Pharm. 2019;16(4):1444–55. https://doi.org/10.1021/acs.molpharmaceut.8b01012 Epub 2019 Mar 6.
Gao W, Lee D, Meng Z, Li T. Exploring intracellular fate of drug nanocrystals with crystal-integrated and environment-sensitive fluorophores. J Control Release. 2017;267:214–22. https://doi.org/10.1016/j.jconrel.2017.08.031 Epub 2017 Aug 24.
Wang M, Zhang Y, Feng J, Gu T, Dong Q, Yang X, et al. Preparation, characterization, and in vitro and in vivo investigation of chitosan-coated poly (d,l-lactide-co-glycolide) nanoparticles for intestinal delivery of exendin-4. Int J Nanomedicine. 2013;8:1141–54. https://doi.org/10.2147/IJN.S41457 Epub 2013 Mar 15.
Alam MA, Al-Jenoobi FI, Al-Mohizea AM. Everted gut sac model as a tool in pharmaceutical research: limitations and applications. J Pharm Pharmacol. 2012;64(3):326–36. https://doi.org/10.1111/j.2042-7158.2011.01391.x Epub 2011 Nov 10.
Bohets H, Annaert P, Mannens G, Van Beijsterveldt L, Anciaux K, Verboven P, et al. Strategies for absorption screening in drug discovery and development. Curr Top Med Chem. 2001;1(5):367–83. https://doi.org/10.2174/1568026013394886.
Dahlgren D, Cano-Cebrián MJ, Olander T, Hedeland M, Sjöblom M, Lennernäs H. Regional intestinal drug permeability and effects of permeation enhancers in rat. Pharmaceutics. 2020;12(3):242. https://doi.org/10.3390/pharmaceutics12030242.
Chang D, Ma Y, Cao G, Wang J, Zhang X, Feng J, et al. Improved oral bioavailability for lutein by nanocrystal technology: formulation development, in vitro and in vivo evaluation. Artif Cells Nanomed Biotechnol. 2018;46(5):1018–24. https://doi.org/10.1080/21691401.2017.1358732 Epub 2017 Jul 27.
Cruz LJ, Stammes MA, Que I, van Beek ER, Knol-Blankevoort VT, Snoeks TJA, et al. Effect of PLGA NP size on efficiency to target traumatic brain injury. J Control Release. 2016 Feb 10;223:31–41. https://doi.org/10.1016/j.jconrel.2015.12.029 Epub 2015 Dec 18.
Zhao Z, Chen S, Shen X, Mahtab F, Yu Y, Lu P, et al. Aggregation-induced emission, self-assembly, and electroluminescence of 4,4′-bis(1,2,2-triphenylvinyl)biphenyl. Chem Commun (Camb). 2010;46(5):686–8. https://doi.org/10.1039/b915271g Epub 2009 Oct 14.
Crecente-Campo J, Guerra-Varela J, Peleteiro M, Gutiérrez-Lovera C, Fernández-Mariño I, Diéguez-Docampo A, et al. The size and composition of polymeric nanocapsules dictate their interaction with macrophages and biodistribution in zebrafish. J Control Release. 2019;308:98–108. https://doi.org/10.1016/j.jconrel.2019.07.011 Epub 2019 Jul 12.
Funding
This work was supported by the National Natural Science Foundations of China (81860628), and Ningxia Key Research and Development Projects (No. 2019BEG03038).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tian, Z., Mai, Y., Meng, T. et al. Nanocrystals for Improving Oral Bioavailability of Drugs: Intestinal Transport Mechanisms and Influencing Factors. AAPS PharmSciTech 22, 179 (2021). https://doi.org/10.1208/s12249-021-02041-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-021-02041-7