Abstract
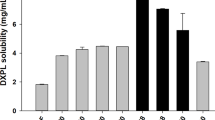
Nowadays, the incidence of acute bacterial skin and skin structure infection (ABSSSI) is increasing. The increased bioavailability and reduced drug resistance of antibiotics are crucial to obtain a more effective treatment response in these infections. These favorable properties could be achieved by different drug delivery systems such as liposomes. In this study, nanosized, radiolabeled tedizolid phosphate liposomal formulations were prepared and evaluated with their in vitro cellular binding capacity and biocompatible profile for topical treatment of ABSSSI. Liposomes were characterized by evaluation of their visual inspection, particle size (about 190–270 nm), zeta potential value (around 0), and encapsulation efficiency (nearly 10%). The release rate of tedizolid phosphate from liposomes was also studied using dialysis membranes and evaluated kinetically. The stability of formulations was observed at three different temperatures and humidity conditions for 28 days. Afterward, liposomes were labeled with 99mTc, and the optimal amount of reducing agent (stannous chloride) was determined as 500 μg in this direct labeling procedure. All liposome formulations were successfully radiolabeled with high efficiency and exhibited high radiochemical purity (> 80%) during 6 h in different media. Furthermore, the cellular bindings of liposomal formulations were evaluated in human skin fibroblast cells by measuring the radioactivity. Higher radioactivity values were obtained in CCD-1070Sk cells incubated by liposome formulations compared to sodium pertechnetate. This finding suggested that liposomal formulation increased the cellular binding of radioactivity. By the result of our study, nanosized, tedizolid phosphate encapsulated liposome formulation was found to be a favorable carrier system in the treatment of ABSSSI.





Similar content being viewed by others
References
Kaye KS, Petty LA, Shorr AF, Zilberberg MD. Current epidemiology, etiology, and burden of acute skin infections in the United States. Clin Infect Dis. 2019;68(Suppl 3):S193–S9. https://doi.org/10.1093/cid/ciz002.
Pollack CV Jr, Amin A, Ford WT Jr, Finley R, Kaye KS, Nguyen HH, et al. Acute bacterial skin and skin structure infections (ABSSSI): practice guidelines for management and care transitions in the emergency department and hospital. J Emerg Med. 2015;48(4):508–19. https://doi.org/10.1016/j.jemermed.2014.12.001.
Golan Y. Current treatment options for acute skin and skin-structure infections. Clin Infect Dis. 2019;68(Suppl 3):S206–S12. https://doi.org/10.1093/cid/ciz004.
Cesur S. Topical antibiotics and clinical use. Mikrobiyol Bul. 2002;36(3–4):353–61.
Bangham AD, Standish MM, Watkins JC. Diffusion of univalent ions across the lamellae of swollen phospholipids. J Mol Biol. 1965;13(1):238–52. https://doi.org/10.1016/s0022-2836(65)80093-6.
Aliakbari F, Shabani AA, Bardania H, Mohammad-Beigi H, Tayaranian Marvian A, Dehghani Esmatabad F, et al. Formulation and anti-neurotoxic activity of baicalein-incorporating neutral nanoliposome. Colloids Surf B Biointerfaces. 2018;161:578–87. https://doi.org/10.1016/j.colsurfb.2017.11.023.
Mahmoudi R, Ashraf Mirahmadi-Babaheidri S, Delaviz H, Fouani MH, Alipour M, Jafari Barmak M, et al. RGD peptide-mediated liposomal curcumin targeted delivery to breast cancer cells. J Biomater Appl. 2020;885328220949367:088532822094936. https://doi.org/10.1177/0885328220949367.
Bardania H, Shojaosadati SA, Kobarfard F, Dorkoosh F. Optimization of RGD-modified nano-liposomes encapsulating eptifibatide. Iran J Biotechnol. 2016;14(2):33–40. https://doi.org/10.15171/ijb.1399.
Altin JG, Parish CR. Liposomal vaccines—targeting the delivery of antigen. Methods. 2006;40(1):39–52. https://doi.org/10.1016/j.ymeth.2006.05.027.
Zhang Y, Rong Qi X, Gao Y, Wei L, Maitani Y, Nagai T. Mechanisms of co-modified liver-targeting liposomes as gene delivery carriers based on cellular uptake and antigens inhibition effect. J Control Release. 2007;117(2):281–90. https://doi.org/10.1016/j.jconrel.2006.11.006.
Barenholz Y. Doxil(R)—the first FDA-approved nano-drug: lessons learned. J Control Release. 2012;160(2):117–34. https://doi.org/10.1016/j.jconrel.2012.03.020.
Stone NR, Bicanic T, Salim R, Hope W. Liposomal amphotericin B (AmBisome((R))): a review of the pharmacokinetics, pharmacodynamics, clinical experience and future directions. Drugs. 2016;76(4):485–500. https://doi.org/10.1007/s40265-016-0538-7.
Bobo D, Robinson KJ, Islam J, Thurecht KJ, Corrie SR. Nanoparticle-based medicines: a review of FDA-approved materials and clinical trials to date. Pharm Res. 2016;33(10):2373–87. https://doi.org/10.1007/s11095-016-1958-5.
Alam M, Hartrick CT. Extended-release epidural morphine (DepoDur): an old drug with a new profile. Pain Pract. 2005;5(4):349–53. https://doi.org/10.1111/j.1533-2500.2005.00048.x.
Pierre MB, Dos Santos Miranda Costa I. Liposomal systems as drug delivery vehicles for dermal and transdermal applications. Arch Dermatol Res. 2011;303(9):607–21. https://doi.org/10.1007/s00403-011-1166-4.
Perugini P, Genta I, Pavanetto F, Conti B, Scalia S, Baruffini A. Study on glycolic acid delivery by liposomes and microspheres. Int J Pharm. 2000;196(1):51–61. https://doi.org/10.1016/s0378-5173(99)00439-1.
Patel VB, Misra A, Marfatia YS. Topical liposomal gel of tretinoin for the treatment of acne: research and clinical implications. Pharm Dev Technol. 2000;5(4):455–64. https://doi.org/10.1081/pdt-100102029.
Wong E, Rab S. Tedizolid phosphate (sivextro): a second-generation oxazolidinone to treat acute bacterial skin and skin structure infections. P T. 2014;39(8):555–79.
Cada DJ, Ingram K, Baker DE. Tedizolid phosphate. Hosp Pharm. 2014;49(10):961–71. https://doi.org/10.1310/hpj4910-961.
Yum JH, Choi SH, Yong D, Chong Y, Im WB, Rhee DK, et al. Comparative in vitro activities of torezolid (DA-7157) against clinical isolates of aerobic and anaerobic bacteria in South Korea. Antimicrob Agents Chemother. 2010;54(12):5381–6. https://doi.org/10.1128/AAC.00728-10.
Jones RN, Moet GJ, Sader HS, Mendes RE, Castanheira M. TR-700 in vitro activity against and resistance mutation frequencies among Gram-positive pathogens. J Antimicrob Chemother. 2009;63(4):716–20. https://doi.org/10.1093/jac/dkp021.
Schaadt R, Sweeney D, Shinabarger D, Zurenko G. In vitro activity of TR-700, the active ingredient of the antibacterial prodrug TR-701, a novel oxazolidinone antibacterial agent. Antimicrob Agents Chemother. 2009;53(8):3236–9. https://doi.org/10.1128/AAC.00228-09.
Thomson KS, Goering RV. Activity of tedizolid (TR-700) against well-characterized methicillin-resistant Staphylococcus aureus strains of diverse epidemiological origins. Antimicrob Agents Chemother. 2013;57(6):2892–5. https://doi.org/10.1128/AAC.00274-13.
Prokocimer P, Bien P, Surber J, Mehra P, DeAnda C, Bulitta JB, et al. Phase 2, randomized, double-blind, dose-ranging study evaluating the safety, tolerability, population pharmacokinetics, and efficacy of oral torezolid phosphate in patients with complicated skin and skin structure infections. Antimicrob Agents Chemother. 2011;55(2):583–92. https://doi.org/10.1128/AAC.00076-10.
Moran GJ, Fang E, Corey GR, Das AF, De Anda C, Prokocimer P. Tedizolid for 6 days versus linezolid for 10 days for acute bacterial skin and skin-structure infections (ESTABLISH-2): a randomised, double-blind, phase 3, non-inferiority trial. Lancet Infect Dis. 2014;14(8):696–705. https://doi.org/10.1016/S1473-3099(14)70737-6.
Prokocimer P, De Anda C, Fang E, Mehra P, Das A. Tedizolid phosphate vs linezolid for treatment of acute bacterial skin and skin structure infections: the ESTABLISH-1 randomized trial. JAMA. 2013;309(6):559–69. https://doi.org/10.1001/jama.2013.241.
Van Giau V, An SSA, Hulme J. Recent advances in the treatment of pathogenic infections using antibiotics and nano-drug delivery vehicles. Drug Des Devel Ther. 2019;13:327–43. https://doi.org/10.2147/DDDT.S190577.
Steen EJL, Edem PE, Norregaard K, Jorgensen JT, Shalgunov V, Kjaer A, et al. Pretargeting in nuclear imaging and radionuclide therapy: improving efficacy of theranostics and nanomedicines. Biomaterials. 2018;179:209–45. https://doi.org/10.1016/j.biomaterials.2018.06.021.
Verma DD, Verma S, Blume G, Fahr A. Particle size of liposomes influences dermal delivery of substances into skin. Int J Pharm. 2003;258(1–2):141–51. https://doi.org/10.1016/s0378-5173(03)00183-2.
du Plessis J, Ramachandran C, Weiner N, Müller DG. The influence of particle size of drug of liposomcs on the deposition into skin. Int J Pharm. 1994;6:272–82. https://doi.org/10.1016/0378-5173(94)90178-3.
Danaei M, Dehghankhold M, Ataei S, Hasanzadeh Davarani F, Javanmard R, Dokhani A, et al. Impact of particle size and polydispersity index on the clinical applications of lipidic nanocarrier systems. Pharmaceutics. 2018;10(2). https://doi.org/10.3390/pharmaceutics10020057.
Magarkar A, Dhawan V, Kallinteri P, Viitala T, Elmowafy M, Rog T, et al. Cholesterol level affects surface charge of lipid membranes in saline solution. Sci Rep. 2014;4:5005. https://doi.org/10.1038/srep05005.
van Hoogevest P, Wendel A. The use of natural and synthetic phospholipids as pharmaceutical excipients. Eur J Lipid Sci Technol. 2014;116(9):1088–107. https://doi.org/10.1002/ejlt.201400219.
Karpuz M, Silindir-Gunat M, Kursunel MA, Esendagli G, Dogan A, Ozer AY. Design and in vitro evaluation of folate-targeted, co-drug encapsulated theranostic liposomes for non-small cell lung cancer. J Drug Deliv Sci Technol. 2020;57:101707.
Silindir-Gunay M, Ozer AY, Erdogan S, Bodard S, Baysal I, Gulhan Z, et al. Development of nanosized, pramipexole-encapsulated liposomes and niosomes for the treatment of Parkinson’s disease. J Nanosci Nanotechnol. 2017;17:13.
Maherani B, Arab-Tehrany E, Kheirolomoom A, Geny D, Linder M. Calcein release behavior from liposomal bilayer; influence of physicochemical/mechanical/structural properties of lipids. Biochimie. 2013;95(11):2018–33. https://doi.org/10.1016/j.biochi.2013.07.006.
Dash S, Murthy PN, Nath L, Chowdhury P. Kinetic modeling on drug release from controlled drug delivery systems. Acta Pol Pharm. 2010;67(3):217–23.
Wojcik-Pastuszka D, Krzak J, Macikowski B, Berkowski R, Osinski B, Musial W. Evaluation of the release kinetics of a pharmacologically active substance from model intra-articular implants replacing the cruciate ligaments of the knee. Materials (Basel). 2019;12(8). https://doi.org/10.3390/ma12081202.
Karthikeyan MD, Deepa MK, Bassim E, Rahna CS, Sree Raj KR. Investigation of kinetic drug release characteristics and in vitro evaluation of sustained-release matrix tablets of a selective COX-2 inhibitor for rheumatic diseases. J Pharm Innov. 2020. https://doi.org/10.1007/s12247-020-09459-9.
Papagiannopoulou D. Technetium-99m radiochemistry for pharmaceutical applications. J Labelled Comp Radiopharm. 2017;60(11):502–20. https://doi.org/10.1002/jlcr.3531.
Garg M, Garg BR, Jain S, Mishra P, Sharma RK, Mishra AK, et al. Radiolabeling, pharmacoscintigraphic evaluation and antiretroviral efficacy of stavudine loaded 99mTc labeled galactosylated liposomes. Eur J Pharm Sci. 2008;33(3):271–81. https://doi.org/10.1016/j.ejps.2007.12.006.
De Silva L, Fu JY, Htar TT, Muniyandy S, Kasbollah A, Wan Kamal WHB, et al. Characterization, optimization, and in vitro evaluation of Technetium-99m-labeled niosomes. Int J Nanomedicine. 2019;14:1101–17. https://doi.org/10.2147/IJN.S184912.
Baldas J, Bonnyman J, Pojer PM, Williams GA. The influence of reducing agents on the composition of 99Tc-complexes: implications for 99mTc-radiopharmaceutical preparation. Eur J Nucl Med. 1982;7(4):187–9. https://doi.org/10.1007/BF00443930.
Stern HS, Zolle I, McAfee JG. Preparation of technetium (Tc99m)-labeled serum albumin (human). Int J Appl Radiat Isot. 1965;16:283–8. https://doi.org/10.1016/0020-708x(65)90182-1.
Ilem-Ozdemir D, Atlihan-Gundogdu E, Ekinci M, Halay E, Ay K, Karayildirim T, et al. Radiolabeling and in vitro evaluation of a new 5-fluorouracil derivative with cell culture studies. J Labelled Comp Radiopharm. 2019;62(13):874–84. https://doi.org/10.1002/jlcr.3804.
Arulsudar N, Subramanian N, Mishra P, Chuttani K, Sharma RK, Murthy RS. Preparation, characterization, and biodistribution study of technetium-99m-labeled leuprolide acetate-loaded liposomes in Ehrlich ascites tumor-bearing mice. AAPS PharmSci. 2004;6(1):E5. https://doi.org/10.1208/ps060105.
Alhariri M, Azghani A, Omri A. Liposomal antibiotics for the treatment of infectious diseases. Expert Opin Drug Deliv. 2013;10(11):1515–32. https://doi.org/10.1517/17425247.2013.822860.
Silindir M, Erdogan S, Ozer AY, Dogan AL, Tuncel M, Ugur O, et al. Nanosized multifunctional liposomes for tumor diagnosis and molecular imaging by SPECT/CT. J Liposome Res. 2013;23(1):20–7. https://doi.org/10.3109/08982104.2012.722107.
Mallick S, Choi JS. Liposomes: versatile and biocompatible nanovesicles for efficient biomolecules delivery. J Nanosci Nanotechnol. 2014;14(1):755–65. https://doi.org/10.1166/jnn.2014.9080.
Hajiahmadi F, Alikhani MY, Shariatifar H, Arabestani MR, Ahmadvand D. The bactericidal effect of liposomal vancomycin as a topical combating system against Methicillin-resistant Staphylococcus aureus skin wound infection in mice. Med J Islam Repub Iran. 2019;33:153. https://doi.org/10.34171/mjiri.33.153.
Bardania H, Shojaosadati SA, Kobarfard F, Morshedi D, Aliakbari F, Tahoori MT, et al. RGD-modified nano-liposomes encapsulated eptifibatide with proper hemocompatibility and cytotoxicity effect. Iran J Biotechnol. 2019;17(2):e2008. https://doi.org/10.21859/ijb.2008.
Funding
This study was supported by Izmir Katip Celebi University Scientific Research Projects Coordination Unit, Project No: 2018-ONAP-ECZF-0002.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Karpuz, M., Atlihan-Gundogdu, E., Demir, E.S. et al. Radiolabeled Tedizolid Phosphate Liposomes for Topical Application: Design, Characterization, and Evaluation of Cellular Binding Capacity. AAPS PharmSciTech 22, 62 (2021). https://doi.org/10.1208/s12249-020-01917-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-020-01917-4