Abstract
Hepatocellular carcinoma (HCC) is a foremost type of cancer problem in which asialoglycoprotein receptors are overexpressed. In this study, asialoglycoprotein receptor–targeted nanoformulation (galactose-conjugated TPGS micelles) loaded with docetaxel (DTX) was developed to achieve its site-specific delivery for HCC therapy. The pharmaceutical characteristics like shape morphology, average particle size and zeta potential, drug entrapment efficiency, and in vitro release kinetics of developed system were evaluated. DTX-loaded galactosylated TPGS (DTX-TPGS-Gal) micelles and TPGS micelles (DTX-TPGS) were having 58.76 ± 1.82% and 54.76 ± 1.42% entrapment of the DTX, respectively. In vitro drug release behavior from micelles was controlled release. Cytotoxicitiy (IC50) of DTX-TPGS-Gal formulation on HepG2 cell lines was significantly (p ≤ 0.01) lower (6.3 ± 0.86 μg/ml) than DTX-TPGS (9.06 ± 0.82 μg/ml) and plain DTX (16.06 ± 0.98 μg/ml) indicating higher efficacy of targeted formulation. Further, in vivo biodistribution studies in animal model showed maximum drug accumulation at target site, i.e., the liver in the case of DTX-TPGS-Gal as compared with non-targeted one. It is concluded from the findings that TPGS-Gal micelles can be utilized for targeted drug delivery of cytotoxic drugs towards HCC with minimized side effects.

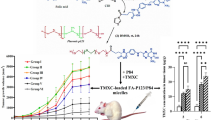
Graphical abstract






Similar content being viewed by others
References
Llovet JM, Decaens T, Raoul JL, Boucher E, Kudo M, Chang C, et al. Brivanib in patients with advanced hepatocellular carcinoma who were intolerant to sorafenib or for whom sorafenib failed: results from the randomized phase III BRISK-PS study. J Clin Oncol. 2013;31(28):3509–16. https://doi.org/10.1200/JCO.2012.47.3009.
Qin LX, Tang ZY. The prognostic significance of clinical and pathological features in hepatocellular carcinoma. World J Gastroenterol. 2002;8(2):193–9.
Gueritte-Voegelein F, Guenard D, Lavelle F, le Goff MT, Mangatal L, Potier P. Relationships between the structure of taxol analogues and their antimitotic activity. J Med Chem. 1991;34(3):992–8.
Wenzel C, Locker GJ, Schmidinger M, Rudas M, Taucher S, Gnant MFX, et al. Combined analysis of two phase II trials in patients with primary and advanced breast cancer with epidoxorubicin and docetaxel+granulocyte colony stimulating factor. Anti-Cancer Drugs. 2002;13(1):67–74.
Cascinu S, Graziano F, Barni S, Labianca R, Comella G, Casaretti R, et al. A phase II study of sequential chemotherapy with docetaxel after the weekly PELF regimen in advanced gastric cancer. A report from the Italian group for the study of digestive tract cancer. Br J Cancer. 2001;84(4):470–4. https://doi.org/10.1054/bjoc.2000.1631.
Ryan DP, Kulke MH, Fuchs CS, Grossbard ML, Grossman SR, Morgan JA, et al. A phase II study of gemcitabine and docetaxel in patients with metastatic pancreatic carcinoma. Cancer. 2002;94(1):97–103.
Sinibaldi VJ, Carducci MA, Moore-Cooper S, Laufer M, Zahurak M, Eisenberger MA. Phase II evaluation of docetaxel plus one-day oral estramustine phosphate in the treatment of patients with androgen independent prostate carcinoma. Cancer. 2002;94(5):1457–65.
Geng CX, Zeng ZC, Wang JY. Docetaxel inhibits SMMC-7721 human hepatocellular carcinoma cells growth and induces apoptosis. World J Gastroenterol. 2003;9(4):696–700.
Lin HL, Liu TY, Chau GY, Lui WY, Chi CW. Comparison of 2-methoxyestradiol-induced, docetaxel-induced, and paclitaxel-induced apoptosis in hepatoma cells and its correlation with reactive oxygen species. Cancer. 2000;89(5):983–94.
Hebbar M, Ernst O, Cattan S, Dominguez S, Oprea C, Mathurin P, et al. Phase II trial of docetaxel therapy in patients with advanced hepatocellular carcinoma. Oncology. 2006;70(2):154–8. https://doi.org/10.1159/000093007.
Paliwal SR, Paliwal R, Agrawal GP, Vyas SP. Liposomal nanomedicine for breast cancer therapy. Nanomedicine : Nanotechnology, Biology, and Medicine. 2011;6(6):1085–100.
Choudhury H, Gorain B, Pandey M, Kumbhar SA, Tekade RK, Iyer AK, et al. Recent advances in TPGS-based nanoparticles of docetaxel for improved chemotherapy. Int J Pharm. 2017;529(1–2):506–22. https://doi.org/10.1016/j.ijpharm.2017.07.018.
Kurmi BD, Kayat J, Gajbhiye V, Tekade RK, Jain NK. Micro- and nanocarrier-mediated lung targeting. Exp Opin Drug Deliv. 2010;7(7):781–94. https://doi.org/10.1517/17425247.2010.492212.
Souris JS, Lee CH, Cheng SH, Chen CT, Yang CS, Ho JAA, et al. Surface charge-mediated rapid hepatobiliary excretion of mesoporous silica nanoparticles. Biomaterials. 2010;31(21):5564–74. https://doi.org/10.1016/j.biomaterials.2010.03.048.
Trere D, Fiume L, De Giorgi LB, et al. The asialoglycoprotein receptor in human hepatocellular carcinomas: its expression on proliferating cells. Br J Cancer. 1999;81(3):404–8. https://doi.org/10.1038/sj.bjc.6690708.
Varshosaz J, Hassanzadeh F, Sadeghi H, Khadem M. Galactosylated nanostructured lipid carriers for delivery of 5-FU to hepatocellular carcinoma. J Liposome Res. 2012;22(3):224–36. https://doi.org/10.3109/08982104.2012.662653.
Kim TH, Park IK, Nah JW, Choi YJ, Cho CS. Galactosylated chitosan/DNA nanoparticles prepared using water-soluble chitosan as a gene carrier. Biomaterials. 2004;25(17):3783–92. https://doi.org/10.1016/j.biomaterials.2003.10.063.
Terada T, Iwai M, Kawakami S, Yamashita F, Hashida M. Novel PEG-matrix metalloproteinase-2 cleavable peptide-lipid containing galactosylated liposomes for hepatocellular carcinoma-selective targeting. J Control Release. 2006;111(3):333–42. https://doi.org/10.1016/j.jconrel.2005.12.023.
Managit C, Kawakami S, Yamashita F, Hashida M. Effect of galactose density on asialoglycoprotein receptor-mediated uptake of galactosylated liposomes. J Pharm Sci. 2005;94(10):2266–75. https://doi.org/10.1002/jps.20443.
Ma Y, Chen H, Su S, Wang T, Zhang C, Fida G, et al. Galactose as broad ligand for multiple tumor imaging and therapy. J Cancer. 2015;6(7):658–70. https://doi.org/10.7150/jca.11647.
Huang KW, Lai YT, Chern GJ, Huang SF, Tsai CL, Sung YC, et al. Galactose derivative-modified nanoparticles for efficient siRNA delivery to hepatocellular carcinoma. Biomacromolecules. 2018;19(6):2330–9. https://doi.org/10.1021/acs.biomac.8b00358.
Zheng G, Zhao R, Xu A, Shen Z, Chen X, Shao J. Co-delivery of sorafenib and siVEGF based on mesoporous silica nanoparticles for ASGPR mediated targeted HCC therapy. Eur J Pharm Sc. 2018;111:492–502. https://doi.org/10.1016/j.ejps.2017.10.036.
Duan C, Gao J, Zhang D, Jia L, Liu Y, Zheng D, et al. Galactose-decorated pH-responsive nanogels for hepatoma-targeted delivery of oridonin. Biomacromolecules. 2011;12(12):4335–43. https://doi.org/10.1021/bm201270m.
Zhao J, Mi Y, Feng SS. Targeted co-delivery of docetaxel and siPlk1 by herceptin-conjugated vitamin E TPGS based immunomicelles. Biomaterials. 2013;34(13):3411–21. https://doi.org/10.1016/j.biomaterials.2013.01.009.
Bhadra D, Yadav AK, Bhadra S, Jain NK. Glycodendrimeric nanoparticulate carriers of primaquine phosphate for liver targeting. Int J Pharm. 2005;295(1–2):221–33. https://doi.org/10.1016/j.ijpharm.2005.01.026.
Kutty RV, Feng SS. Cetuximab conjugated vitamin E TPGS micelles for targeted delivery of docetaxel for treatment of triple negative breast cancers. Biomaterials. 2013;34(38):10160–71. https://doi.org/10.1016/j.biomaterials.2013.09.043.
Saxena V, Hussain MD. Poloxamer 407/TPGS mixed micelles for delivery of gambogic acid to breast and multidrug-resistant cancer. Int J Nanomedicine. 2012;7:713–21. https://doi.org/10.2147/IJN.S28745.
Sheetal M. A simple ultraviolet spectrophotometric method for the estimation of docetaxel in bulk drug and formulation. Asian J Pharm Anal. 2013;3(2):48–52.
Kurmi BD, Gajbhiye V, Kayat J, Jain NK. Lactoferrin-conjugated dendritic nanoconstructs for lung targeting of methotrexate. J Pharm Sci. 2011;100(6):2311–20. https://doi.org/10.1002/jps.22469.
Zhu X, Tsend-Ayush A, Yuan Z, Wen J, Cai J, Luo S, et al. Glycyrrhetinic acid-modified TPGS polymeric micelles for hepatocellular carcinoma-targeted therapy. Int J Pharm. 2017;529(1–2):451–64. https://doi.org/10.1016/j.ijpharm.2017.07.011.
Mi Y, Liu Y, Feng SS. Formulation of docetaxel by folic acid-conjugated d-alpha-tocopheryl polyethylene glycol succinate 2000 (vitamin E TPGS(2k)) micelles for targeted and synergistic chemotherapy. Biomaterials. 2011;32(16):4058–66. https://doi.org/10.1016/j.biomaterials.2011.02.022.
Liu Y, Li K, Liu B, Feng SS. A strategy for precision engineering of nanoparticles of biodegradable copolymers for quantitative control of targeted drug delivery. Biomaterials. 2010;31(35):9145–55. https://doi.org/10.1016/j.biomaterials.2010.08.053.
Liu H, Wang H, Xu Y, Guo R, Wen S, Huang Y, et al. Lactobionic acid-modified dendrimer-entrapped gold nanoparticles for targeted computed tomography imaging of human hepatocellular carcinoma. ACS Appl Mater Interfaces. 2014;6(9):6944–53. https://doi.org/10.1021/am500761x.
Peng DJ, Sun J, Wang YZ, Tian J, Zhang YH, Noteborn MHM, et al. Inhibition of hepatocarcinoma by systemic delivery of Apoptin gene via the hepatic asialoglycoprotein receptor. Cancer Gene Ther. 2007;14(1):66–73. https://doi.org/10.1038/sj.cgt.7700985.
Wang S, Cheng L, Yu F, Pan W, Zhang J. Delivery of different length poly(L-lysine)-conjugated ODN to HepG2 cells using N-stearyllactobionamide-modified liposomes and their enhanced cellular biological effects. Int J Pharm. 2006;311(1–2):82–8. https://doi.org/10.1016/j.ijpharm.2005.12.014.
Paliwal SR, Paliwal R, Mishra N, Mehta A, Vyas SP. A novel cancer targeting approach based on estrone anchored stealth liposome for site-specific breast cancer therapy. Curr Cancer Drug Targets. 2010;10(3):343–53.
Matsumura Y, Maeda H. A new concept for macromolecular therapeutics in cancer chemotherapy: mechanism of tumoritropic accumulation of proteins and the antitumor agent smancs. Cancer Res. 1986;46(12 Pt 1):6387–92.
Tekchandani P, Kurmi BD, Paliwal SR. Nanomedicine to deal with cancer cell biology in multi-drug resistance. Mini Rev Med Chem. 2017;17(18):1793–810. https://doi.org/10.2174/1389557516666160219123222.
Xu Z, Chen L, Gu W, Gao Y, Lin L, Zhang Z, et al. The performance of docetaxel-loaded solid lipid nanoparticles targeted to hepatocellular carcinoma. Biomaterials. 2009;30(2):226–32. https://doi.org/10.1016/j.biomaterials.2008.09.014.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tekchandani, P., Kurmi, B.D., Paliwal, R. et al. Galactosylated TPGS Micelles for Docetaxel Targeting to Hepatic Carcinoma: Development, Characterization, and Biodistribution Study. AAPS PharmSciTech 21, 174 (2020). https://doi.org/10.1208/s12249-020-01690-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-020-01690-4