Abstract
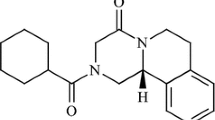
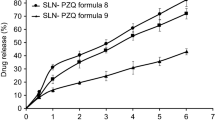
Praziquantel is a broad spectrum antihelmintic agent and represents the drug of choice for the treatment of schistosomiasis. However, its low aqueous solubility and strong bitter taste highly affect the bioavailability and compliance in pediatric patients. Thus, the purpose of this study was to develop a dry nanosuspension, by a combination of high-pressure homogenization and spray drying, intended for redispersion in a pleasant taste vehicle for extemporaneous use. Three formulations, varying stabilizers to drug ratio, were developed and characterized in terms of particle size distribution, crystallinity, morphology, in vitro dissolution, and sedimentation-redispersibility behavior. A significant reduction in particle size was achieved after the high-pressure homogenization process, and the nanoparticles were further microencapsulated by spray drying technique. The redispersed dried powders exhibited a conserved particle size distribution (in the nanometric range) and certain crystallinity extent, with satisfactory redispersion ability. Besides, the enhancement of the dissolution performance obtained after comminution was conserved, even after drying and redispersion of the extemporaneous powdered formulation. In conclusion, the developed nanoparticle-loaded powders comprise an interesting tool for the administration of praziquantel to preschool-age children.





Similar content being viewed by others
References
WHO, World Health Organization. Schistosomiasis, Disease. https://www.who.int/schistosomiasis/disease/en/. Accessed 9th May 2019.
WHO Schistosomiasis Fact Sheet. https://www.who.int/en/news-room/fact-sheets/detail/schistosomiasis. Accessed 9th May 2019
World Health Organization. Report of a meeting to review the results of studies on the treatment of Schistosomiasis in preschool-age children. Geneva, Switzerland, 2010. Available: https://apps.who.int/iris/bitstream/handle/10665/44639/9789241501880_eng.pdf?sequence=1. Accessed 9th May 2019.
WHO. Model list of essential medicines. 20th ed. Geneva: World Health Organization; 2017. Available in: https://apps.who.int/iris/bitstream/handle/10665/273826/EML-20-eng.pdf?ua=1. Accessed 9th May 2019
Fenwick A, Webster JP, Bosque-Oliva E, Blair L, Fleming FM, Zhang Y, et al. The Schistosomiasis Control Initiative (SCI): rationale, development and implementation from 2002–2008. Parasitology 2009. 136(13):1719–30. https://doi.org/10.1017/S0031182009990400.
Patzschke K, Putter J, Wegner LA, Horster FA, Diekmann HW. Serum concentrations and renal excretion in humans after oral administration of praziquantel - results of three determination methods. Eur J Drug Metab Pharmacokinet. 1979;4(3):149–56. https://doi.org/10.1007/BF03189418.
Trastullo R, Dolci LS, Passerini N, Albertini B. Development of flexible and dispersible oral formulations containing praziquantel for potential schistosomiasis treatment of pre-school age children. Int J Pharm. 2015;495(1):536–50. https://doi.org/10.1016/j.ijpharm.2015.09.019.
WHO. World Health Organization. Schistosomiasis. Strategy; 2016. http://www.who.int/schistosomiasis/strategy/en/. Accessed 9th May 2019.
Pediatric Praziquantel Consortium. https://www.pediatricpraziquantelconsortium.org/schistosomiasis. Accessed 9th May 2019.
Münster M, Mohamed-Ahmed AH, Immohr LI, Schoch C, Schmidt C, Tuleu C, et al. Comparative in vitro and in vivo taste assessment of liquid praziquantel formulations. Int J Pharm. 2017;529(1-2):310–8. https://doi.org/10.1016/j.ijpharm.2017.06.084.
Passerini N, Albertini B, Perissutti B, Rodriguez L. Evaluation of melt granulation and ultrasonic spray congealing as techniques to enhance the dissolution of praziquantel. Int J Pharm. 2006;318(1-2):92–102. https://doi.org/10.1016/j.ijpharm.2006.03.028.
González-Esquivel D, Rivera J, Castro N, Yepez-Mulia L, Helgi JC. In vitro characterization of some biopharmaceutical properties of praziquantel. Int J Pharm. 2005;295(1-2):93–9. https://doi.org/10.1016/j.ijpharm.2005.01.033.
Lindenberg M, Kopp S, Dressman JB. Classification of orally administered drugs on the World Health Organization Model list of Essential Medicines according to the biopharmaceutics classification system. Eur J Pharm Biopharm. 2004;58(2):265–78. https://doi.org/10.1016/j.ejpb.2004.03.001.
Shawahna R. Pediatric biopharmaceutical classification system: using age-appropriate initial gastric volume. AAPS J. 2016;18(3):728–36. https://doi.org/10.1208/s12248-016-9885-2.
Müller RH, Jacobs C, Kayser O. Nanosuspensions as particulate drug formulations in therapy rationale for development and what we can expect for the future. Adv Drug Deliv Rev. 2001;47(1):3–19. https://doi.org/10.1016/S0169-409X(00)00118-6.
Zhou Y, Fang Q, Niu B, Wu B, Zhao Y, Quan G, et al. Comparative studies on amphotericin B nanosuspensions prepared by a high pressure homogenization method and an antisolvent precipitation method. Colloid Surf B Biointerfaces. 2018;172:372–9. https://doi.org/10.1016/j.colsurfb.2018.08.016.
Noyes AA, Whitney WR. The rate of solution of solid substances in their own solutions. J Am Chem Soc. 1897;19(12):930–4. https://doi.org/10.1021/ja02086a00.
Lakshmi P, Kumar GA. Nanosuspension technology: a review. Int J Pharm Sci. 2010;2(4):35–40.
Keck CM, Müller RH. Drug nanocrystals of poorly soluble drugs produced by high-pressure homogenization. Eur J Pharm Biopharm. 2006;62(1):3–16. https://doi.org/10.1016/j.ejpb.2005.05.009.
Foglio Bonda A, Rinaldi M, Segale L, Palugan L, Cerea M, Vecchio C, et al. Nanonized itraconazole powders for extemporary oral suspensions: role of formulation components studied by a mixture design. Eur J Pharm Sci. 2016;83:175–83. https://doi.org/10.1016/j.ejps.2015.12.030.
Wu L, Zhang J, Watanabe W. Physical and chemical stability of drug nanoparticles. Adv Drug Deliv Rev. 2011;63(6):456–69. https://doi.org/10.1016/j.addr.2011.02.001.
Kumar S, Gokhale R, Burgess DJ. Quality by design approach to spray drying processing of crystalline nanosuspensions. Int J Pharm. 2014;464(1-2):234–42. https://doi.org/10.1016/j.ijpharm.2013.12.039.
Zhang X, Guan J, Ni R, Li LC, Mao S. Preparation and solidification of redispersible nanosuspensions. J Pharm Sci. 2014;103(7):2166–76. https://doi.org/10.1002/jps.24015.
Chaubal MV, Popescu C. Conversion of nanosuspensions into dry powders by spray drying: a case study. Pharm Res. 2008;25(10):2302–8. https://doi.org/10.1007/s11095-008-9625-0.
Van Eerdenbrugh B, Van den Mooter G, Augustijns P. Top-down production of drug nanocrystals: nanosuspension stabilization, miniaturization and transformation into solid products. Int J Pharm. 2008;364(1):64–75. https://doi.org/10.1016/j.ijpharm.2008.07.023.
Gonzalez MA, Ramírez-Rigo MV, Gonzalez Vidal NG. Praziquantel systems with improved dissolution rate obtained by high pressure homogenization. Mater Sci Eng C Mater. 2018;93:28–35. https://doi.org/10.1016/j.msec.2018.07.050.
Paredes AJ, Llabot JM, Sanchez Bruni S, Allemandi D, Palma SD. Self-dispersible nanocrystals of albendazole produced by high pressure homogenization and spray-drying. Drug Dev Ind Pharm. 2016;42(10):1564–70. https://doi.org/10.3109/03639045.2016.1151036.
Hecq J, Deleers M, Fanara D, Vranckx H, Amighi K. Preparation and characterization of nanocrystals for solubility and dissolution rate enhancement of nifedipine. Int J Pharm. 2005;299(1-2):167–77. https://doi.org/10.1016/j.ijpharm.2005.05.014.
Münster M, Schoch C, Schmidt C, Breitkreutz J. Multiparticulate system combining taste masking and immediate release properties for the aversive compound praziquantel. Eur J Pharm Sci. 2017;109:446–54. https://doi.org/10.1016/j.ejps.2017.08.034.
Campbell GA, Vallejo E. Primary packaging considerations in developing medicines for children: oral liquid and powder for constitution. J Pharm Sci. 2015;104:52–62. https://doi.org/10.1002/jps.24223.
Strickley RG. Pediatric oral formulations: an updated review of commercially available pediatric oral formulations since 2007. J Pharm Sci. 2019;108(4):1335–65. https://doi.org/10.1016/j.xphs.2018.11.013.
Safety & Toxicity of Exciíents for Paediatrics Database (STEP Database). Available in: http://www.eupfi.org/step-database-info/. Accessed August 10th, 2019
Nahata MC, Morosco RS, Brady MT. Extemporaneous sildenafil citrate oral suspensions for the treatment of pulmonary hypertension in children. Am J Health Syst Pharm. 2006;63(3):254–7. https://doi.org/10.2146/ajhp050208.
Skillman KL, Caruthers RL, Johnson CE. Stability of an extemporaneously prepared clopidogrel oral suspension. Am J Health Syst Pharm. 2010;67(7):559–61. https://doi.org/10.2146/ajhp090163.
Helin-Tanninen M, Autio K, Keski-Rahkonen P, Naaranlahti T, Järvinen K. Comparison of six different suspension vehicles in compounding of oral extemporaneous nifedipine suspension for paediatric patients. Eur J Hosp Pharm. 2012;19:432–7. https://doi.org/10.1136/ejhpharm-2012-000159.
Calcagno AJ, Palma SD, Cabrera F, Ramírez-Rigo MV, Piña J. Meloxicam-Poloxamer solid dispersions by spray drying. Poster presentation. 3° Reunión Internacional de Ciencias Farmacéuticas (RICiFa 2014) Córdoba, Argentina, 2014.
Farmacotecnia, boletín informativo. Sociedad Española de Farmacia Hospitalaria. España; 2014. Available in: https://gruposdetrabajo.sefh.es/farmacotecnia/images/stories/Boletines/BOLETIN32014final.pdf. Accessed 9th May 2019
Haywood A, Glass BD. Liquid dosage forms extemporaneously prepared from commercially available products–considering new evidence on stability. J Pharm Pharm Sci. 2013;16(3):441–55. https://doi.org/10.18433/J38887.
Palazzo F, Giovagnoli S, Schoubben A, Blasi P, Rossi C, Ricci M. Development of a spray-drying method for the formulation of respirable microparticles containing ofloxacin–palladium complex. Int J Pharm. 2013;440(2):273–82. https://doi.org/10.1016/j.ijpharm.2012.05.045.
Di Battista CA, Constenla D, Ramírez-Rigo MV, Piña J. The use of arabic gum, maltodextrin and surfactants in the microencapsulation of phytosterols by spray drying. Powder Technol. 2015;286:193–201. https://doi.org/10.1016/j.powtec.2015.08.016.
Argentine Pharmacopeia, 7th Ed; Administración Nacional de Medicamentos, Alimentos y Tecnología Médica (ANMAT): Buenos Aires, Argentina; 2013.
The United States Pharmacopoeia and National Formulary. USP 41-NF 36. Rockville: The United States Pharmacopoeial Convention, Inc.; 2018.
De la Torre P, Torrado S, Torrado S. Preparation, dissolution and characterization of praziquantel solid dispersions. Chem Pharm Bull. 1999;47(11):1629–33. https://doi.org/10.1248/cpb.47.1629.
Khan KA. The concept of dissolution efficiency. J Pharm Pharmacol. 1975;27(1):48–9. https://doi.org/10.1111/j.2042-7158.1975.tb09378.x.
Zhang Y, Huo M, Zhou J, Zou A, Li W, Yao C, et al. DDSolver: an add-in program for modeling and comparison of drug dissolution profiles. AAPS J. 2010;12(3):263–71. https://doi.org/10.1208/s12248-010-9185-1.
Costa P, Sousa Lobo JM. Modeling and comparison of dissolution profiles. Eur J Pharm Sci. 2001;13(2):123–33. https://doi.org/10.1016/S0928-0987(01)00095-1.
Mengual O, Meunier G, Cayré I, Puech K, Snabre P. TURBISCAN MA 2000: multiple light scattering measurement for concentrated emulsion and suspension instability analysis. Talanta. 1999;50(2):445–56. https://doi.org/10.1016/S0039-9140(99)00129-0.
Celia C, Locatelli M, Cilurzo F, Cosco D, Gentile E, Scalise D, et al. Long term stability evaluation of prostacyclin released from biomedical device through Turbiscan lab expert. Med Chem. 2015;11(4):391–9. https://doi.org/10.2174/1573406410666141110153502.
Vilches AP, Jimenez-Kairuz A, Alovero F, Olivera ME, Allemandi DA, Manzo RH. Release kinetics and up-take studies of model fluoroquinolones from carbomer hydrogels. Int J Pharm. 2002;246(1-2):17–24. https://doi.org/10.1016/S0378-5173(02)00333-2.
Yue PF, Li Y, Wan J, Yang M, Zhu WF. Wang, CH. Study on formability of solid nanosuspensions during nanodispersion and solidification: I. Novel role of stabilizer/drug property. Int J Pharm. 2013;454(1):269–77. https://doi.org/10.1016/j.ijpharm.2013.06.050.
Al-Khattawi A, Bayly A, Phillips A, et al. The design and scale-up of spray dried particle delivery systems. Expert Opin Drug Deliv. 2018;15(1):47–63. https://doi.org/10.1080/17425247.2017.1321634.
Arpagaus C, Schwartzbach H. Scale-up from bench-top research to labotory production. Büchi Mini Spray Dyer B-290. Information Bulletin N° 52/2008.
Ceschan NE, Bucalá V, Ramírez-Rigo MV. New alginic acid–atenolol microparticles for inhalatory drug targeting. Mater Sci Eng C Mater. 2014;41:255–66. https://doi.org/10.1016/j.msec.2014.04.040.
Seremeta KP, Tur MIR, Pérez SM, Höcht C, Taira C, Hernández ODL, et al. Spray-dried didanosine-loaded polymeric particles for enhanced oral bioavailability. Colloid Surf B Biointerfaces. 2014;123:515–23. https://doi.org/10.1016/j.colsurfb.2014.09.055.
Rowe RC, Sheskey PJ, Owen SC, editors. Handbook of pharmaceutical excipients. 5th ed. Pharmaceutical Press: London; 2006. p. 430–3.
Ribeiro de Souza AL, Andreani T, Nunes FM, Cassimiro DL, de Almeida AE, Ribeiro CA, et al. Loading of praziquantel in the crystal lattice of solid lipid nanoparticles: studies by DSC and SAXS. J Therm Anal Calorim. 2011;108(1):353–60. https://doi.org/10.1007/s10973-011-1871-4.
Turner DT, Schwartz A. The glass transition temperature of poly(N-vinyl pyrrolidone) by differential scanning calorimetry. Polymer. 1985;26:757–62. https://doi.org/10.1016/0032-3861(85)90114-4.
Bühler V. Polyvinylpyrrolidone – excipients for pharmaceuticals. Germany: Springer; 2005. p. 87. https://doi.org/10.1007/b138598.
Yoshioka M, Hancock B, Zografi G. Inhibition of indomethacin crystallization in poly(vinylpyrro1idone) coprecipitates. J Pharm Sci. 1995;84(8):983–6. https://doi.org/10.1002/jps.2600840814.
Perissutti B, Passerini N, Trastullo R, Keiser J, Zanolla D, Zingone G, et al. An explorative analysis of process and formulation variables affecting comilling in a vibrational mill: the case of praziquantel. Int J Pharm. 2017;533(2):402–12. https://doi.org/10.1016/j.ijpharm.2017.05.053.
Tantishaiyakul V, Kaewnopparat N, Ingkatawornwong S. Properties of solid dispersions of piroxicam in polyvinylpyrrolidone K-30. Int J Pharm. 1996;143(1):59–66. https://doi.org/10.1016/S0378-5173(96)04687-X.
Mura P, Faucci MT, Manderioli A, Bramanti G, Ceccarelli L. Compatibility study between ibuproxam and pharmaceutical excipients using differential scanning calorimetry, hot-stage microscopy and scanning electron microscopy. J Pharm Biomed Anal. 1998;18(1-2):151–63. https://doi.org/10.1016/S0731-7085(98)00171-X.
Tita B, Fulias A, Bandur G, Marian E, Tita D. Compatibility study between ketoprofen and pharmaceutical excipients used in solid dosage forms. J Pharm Biomed Anal. 2011;56(2):221–7. https://doi.org/10.1016/j.jpba.2011.05.017.
Jackson CL, McKenna GB. The melting behavior of organic materials confined in porous solids. J Chem Phys. 1998;93(12):9002–11. https://doi.org/10.1063/1.459240.
Kuehl C, El-Gendy N, Berkland C. Nanoclusters surface area allows nanoparticle dissolution with microparticle properties. J Pharm Sci. 2014;103(6):1787–98. https://doi.org/10.1002/jps.23980.
Costa ED, Priotti J, Orlandi S, Leonardi D, Lamas MC, Nunes TG, et al. Unexpected solvent impact in the crystallinity of praziquantel/poly (vinylpyrrolidone) formulations. A solubility, DSC and solid-state NMR study. Int J Pharm. 2016;511(2):983–93. https://doi.org/10.1016/j.ijpharm.2016.08.009.
Corrigan OI. Thermal analysis of spray dried products. Thermochim Acta. 1995;248:245–58. https://doi.org/10.1016/0040-6031(94)01891-J.
Cugovčan M, Jablan J, Lovrić J, Cinčić D, Galić N, Jug M. Biopharmaceutical characterization of praziquantel cocrystals and cyclodextrin complexes prepared by grinding. J Pharm Biomed Anal. 2017;137:42–53. https://doi.org/10.1016/j.jpba.2017.01.025.
Sinswat P, Gao X, Yacaman MJ, Williams RO III, Johnston KP. Stabilizer choice for rapid dissolving high potency itraconazole particles formed by evaporative precipitation into aqueous solution. Int J Pharm. 2005;302(1-2):113–24. https://doi.org/10.1016/j.ijpharm.2005.06.027.
Wong SM, Kellaway IW, Murdan S. Enhancement of the dissolution rate and oral absorption of a poorly water soluble drug by formation of surfactant-containing microparticles. Int J Pharm. 2006;317(1):61–8. https://doi.org/10.1016/j.ijpharm.2006.03.001.
El-Subbagh HI, Al-Badr AA. Praziquantel. In: Florey, editor. Analytical profiles of drug substances and excipients, vol. 24: Academic Press Inc; 1998. p. 463–500.
Gao L, Zhang D, Chen M. Drug nanocrystals for the formulation of poorly soluble drugs and its application as a potential drug delivery system. J Nanopart Res. 2008;10(5):845–62. https://doi.org/10.1007/s11051-008-9357-4.
Paredes AJ, Sanchez Bruni S, Allemandi D, Lanusse C, Palma SD. Albendazole nanocrystals with improved pharmacokinetic performance in mice. Ther Deliv. 2018;9(2):89–97. https://doi.org/10.4155/tde-2017-0090.
Lippold BC, Ohm A. Correlation between wettability and dissolution rate of pharmaceutical powders. Int J Pharm. 1986;28(1):67–74. https://doi.org/10.1016/0378-5173(86)90148-1.
Acknowledgments
The authors kindly thank the Universidad Nacional del Sur (PGI 24/ZB70, PGI 24/B252), Agencia Nacional de Promoción Científica y Tecnológica (PICT-2016-0976), and CONICET (PIP 11220150100704CO) for the financial support; Lic. F. Cabrera, Tec. T. Odoux (PLAPIQUI, Argentina), Dr. F. Prado (IFISUR, Argentina), C. Briones Nieva, and Dr. J.M. Bermudez (INIQUI Argentina) for their technical assistance; and Dr. A. Ayala (Universidade Federal do Ceará, Brazil) for the assistance in PXRD data analysis. M. A. Gonzalez is grateful to CONICET (Argentina) for the PhD fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gonzalez, M.A., Ramírez Rigo, M.V. & Gonzalez Vidal, N.L. Orphan Formulations in Pediatric Schistosomiasis Treatment: Development and Characterization of Praziquantel Nanoparticle—Loaded Powders for Reconstitution. AAPS PharmSciTech 20, 318 (2019). https://doi.org/10.1208/s12249-019-1548-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-019-1548-z