Abstract
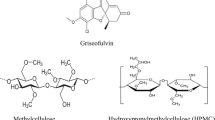
The collective impact of cellulosic polymers on the dissolution, solubility, and crystallization inhibition of amorphous active pharmaceutical ingredients (APIs) is still far from being adequately understood. The goal of this research was to explore the influence of cellulosic polymers and incubation conditions on enhancement of solubility and dissolution of amorphous felodipine, while inhibiting crystallization of the drug from a supersaturated state. Variables, including cellulosic polymer type, amount, ionic strength, and viscosity, were evaluated for effects on API dissolution/solubility and crystallization processes. Water-soluble cellulosic polymers, including HPMC E15, HPMC E5, HPMC K100-LV, L-HPC, and MC, were studied. All cellulosic polymers could extend API dissolution and solubility to various extents by delaying crystallization and prolonging supersaturation duration, with their effectiveness ranked from greatest to least as HPMC E15 > HPMC E5 > HPMC K100-LV > L-HPC > MC. Decreased polymer amount, lower ionic strength, or higher polymer viscosity tended to decrease dissolution/solubility and promote crystal growth to accelerate crystallization. HPMC E15 achieved greatest extended API dissolution and maintenance of supersaturation from a supersaturated state; this polymer thus had the greatest potential for maintaining sustainable API absorption within biologically relevant time frames.











Similar content being viewed by others
References
Amidon GL, Lennernäs H, Shah VP, Crison JR. A theoretical basis for a biopharmaceutic drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm Res. 1995;12(3):413–20.
Khadra I, Zhou Z, Dunn C, Wilson CG, Halbert G. Statistical investigation of simulated intestinal fluid composition on the equilibrium solubility of biopharmaceutics classification system class II drugs. Eur J Pharm Sci. 2015;67:65–75.
Xie F, Ji S, Cheng Z. In vitro dissolution similarity factor (f2) and in vivo bioequivalence criteria, how and when do they match? Using a BCS class II drug as a simulation example. Eur J Pharm Sci. 2015;66:163–72.
Han X, Ghoroi C, To D, Chen Y, Davé R. Simultaneous micronization and surface modification for improvement of flow and dissolution of drug particles. Int J Pharm. 2011;415(1–2):185–95.
He Y, Orton E, Yang D. The selection of a pharmaceutical salt-the effect of the acidity of the counterion on its solubility and potential biopharmaceutical performance. J Pharm Sci. 2018;107(1):419–25.
Zimmermann SC, Tichý T, Vávra J, Dash RP, Slusher CE, Gadiano AJ, et al. N-substituted prodrugs of mebendazole provide improved aqueous solubility and oral bioavailability in mice and dogs. J Med Chem. 2018;61(9):3918–29.
Jansook P, Ogawa N, Loftsson T. Cyclodextrins: structure, physicochemical properties and pharmaceutical applications. Int J Pharm. 2018;535(1–2):272–84.
Parikh T, Serajuddin ATM. Development of fast-dissolving amorphous solid dispersion of itraconazole by melt extrusion of its mixture with weak organic carboxylic acid and polymer. Pharm Res. 2018;35(7):127.
Healy AM, Worku ZA, Kumar D, Madi AM. Pharmaceutical solvates, hydrates and amorphous forms: a special emphasis on cocrystals. Adv Drug Deliv Rev. 2017;117:25–46.
Edueng K, Mahlin D, Bergström CAS. The need for restructuring the disordered science of amorphous drug formulations. Pharm Res. 2017;34(9):1754–72.
Kissi EO, Grohganz H, Löbmann K, Ruggiero MT, Zeitler JA, Rades T. Glass-transition temperature of the β-relaxation as the major predictive parameter for recrystallization of neat amorphous drugs. J Phys Chem B. 2018;122(10):2803–8.
Doreth M, Löbmann K, Priemel P, Grohganz H, Taylor R, Holm R, et al. Influence of PVP molecular weight on the microwave assisted in situ amorphization of indomethacin. Eur J Pharm Biopharm. 2018;122:62–9.
Lehmkemper K, Kyeremateng SO, Heinzerling O, Degenhardt M, Sadowski G. Long-term physical stability of PVP- and PVPVA-amorphous solid dispersions. Mol Pharm. 2017;14(1):157–71.
Li N, Taylor LS. Tailoring supersaturation from amorphous solid dispersions. J Control Release. 2018;279:114–25.
Van den Mooter G. The use of amorphous solid dispersions: a formulation strategy to overcome poor solubility and dissolution rate. Drug Discov Today Technol. 2012;9(2):e71–e174.
Lehmkemper K, Kyeremateng SO, Bartels M, Degenhardt M, Sadowski G. Physical stability of API/polymer-blend amorphous solid dispersions. Eur J Pharm Biopharm. 2018;124:147–57.
Dos Santos KM, Barbosa RM, Vargas FGA, de Azevedo EP, Lins ACDS, Camara CA, et al. Development of solid dispersions of β-lapachone in PEG and PVP by solvent evaporation method. Drug Dev Ind Pharm. 2018;44(5):750–6.
Shi NQ, Lei YS, Song LM, Zhang XB, Wang XL. Impact of amorphous and semicrystalline polymers on the dissolution and crystallization inhibition of pioglitazone solid dispersions. Powder Technol. 2013;247:211–21.
Miyazaki T, Yoshioka S, Aso Y, Kojima S. Ability of polyvinylpyrrolidone and polyacrylic acid to inhibit the crystallization of amorphous acetaminophen. J Pharm Sci. 2004;93(11):2710–7.
Van den Mooter G, Wuyts M, Blaton N, Busson R, Grobet P, Augustijns P, et al. Physical stabilization of amorphous ketoconazole in solid dispersions with polyvinylpyrrolidone K25. Eur J Pharm Sci. 2001;12(3):261–9.
Aso Y, Yoshioka S, Zhang J, Zografi G. Effect of water on the molecular mobility of sucrose and poly(vinylpyrrolidone) in a colyophilized formulation as measured by (13)C-NMR relaxation time. Chem Pharm Bull. 2002;50(6):822–6.
Alonzo DE, Gao Y, Zhou D, Mo H, Zhang GGZ, Taylor LS. Dissolution and precipitation behavior of amorphous solid dispersions. J Pharm Sci. 2011;100(8):3316–31.
Sugihara H, Taylor LS. Evaluation of pazopanib phase behavior following pH-induced supersaturation. Mol Pharm. 2018;15(4):1690–9.
Xie T, Gao W, Taylor LS. Impact of Eudragit EPO and hydroxypropyl methylcellulose on drug release rate, supersaturation, precipitation outcome and redissolution rate of indomethacin amorphous solid dispersions. Int J Pharm. 2017;531(1):313–23.
Sarode AL, Wang P, Obara S, Worthen DR. Supersaturation, nucleation, and crystal growth during single- and biphasic dissolution of amorphous solid dispersions: polymer effects and implications for oral bioavailability enhancement of poorly water soluble drugs. Eur J Pharm Biopharm. 2014;86(3):351–60.
Konno H, Handa T, Alonzo DE, Taylor LS. Effect of polymer type on the dissolution profile of amorphous solid dispersions containing felodipine. Eur J Pharm Biopharm. 2008;70(2):493–9.
Tran TTD, Tran PHL. Perspectives on strategies using swellable polymers in solid dispersions for controlled drug release. Curr Pharm Des. 2017;23(11):1639–48.
Van Duong T, Van den Mooter G. The role of the carrier in the formulation of pharmaceutical solid dispersions. Part II: amorphous carriers. Expert Opin Drug Deliv. 2016;13(12):1681–94.
van der Lee R, Pfaffendorf M, Koopmans RP, van Lieshout JJ, van Montfrans GA, van Zwieten PA. Comparison of the time courses and potencies of the vasodilator effects of nifedipine and felodipine in the human forearm. Blood Press. 2001;10(4):217–22.
Leenen FH, Coletta E. Pharmacokinetic and antihypertensive profile of amlodipine and felodipine-ER in younger versus older patients with hypertension. J Cardiovasc Pharmacol. 2010;56(6):669–75.
Lipinski CA, Lombardo F, Dominy BW, Feeney PJ. Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings. Adv Drug Deliv Rev. 2001;46(1–3):3–26.
Hancock BC, Parks M. What is the true solubility advantage for amorphous pharmaceuticals? Pharm Res. 2000;17(4):397–404.
Bikiaris DN. Solid dispersions, part II: new strategies in manufacturing methods for dissolution rate enhancement of poorly water-soluble drugs. Expert Opin Drug Deliv. 2011;8(12):1663–80.
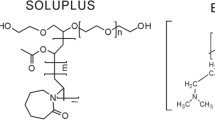
Shi NQ, Lai HW, Zhang Y, Feng B, Xiao X, Zhang HM, et al. On the inherent properties of Soluplus and its application in ibuprofen solid dispersions generated by microwave-quench cooling technology. Pharm Dev Technol. 2018;23(6):573–86.
Tran PH, Tran TT, Lee KH, Kim DJ, Lee BJ. Dissolution-modulating mechanism of pH modifiers in solid dispersion containing weakly acidic or basic drugs with poor water solubility. Expert Opin Drug Deliv. 2010;7(5):647–61.
Fong SY, Bauer-Brandl A, Brandl M. Oral bioavailability enhancement through supersaturation: an update and meta-analysis. Expert Opin Drug Deliv. 2017;14(3):403–26.
Laitinen R, Löbmann K, Grohganz H, Priemel P, Strachan CJ, Rades T. Supersaturating drug delivery systems: the potential of co-amorphous drug formulations. Int J Pharm. 2017;532(1):1–12.
Brouwers J, Brewster ME, Augustijns P. Supersaturating drug delivery systems: the answer to solubility-limited oral bioavailability? J Pharm Sci. 2009;98(8):2549–72.
Brewster ME, Vandecruys R, Verreck G, Peeters J. Supersaturating drug delivery systems: effect of hydrophilic cyclodextrins and other excipients on the formation and stabilization of supersaturated drug solutions. Pharmazie. 2008;63(3):217–20.
Guzmán HR, Tawa M, Zhang Z, Ratanabanangkoon P, Shaw P, Gardner CR, et al. Combined use of crystalline salt forms and precipitation inhibitors to improve oral absorption of celecoxib from solid oral formulations. J Pharm Sci. 2007;96(10):2686–702.
Kawakami K. Modification of physicochemical characteristics of active pharmaceutical ingredients and application of supersaturatable dosage forms for improving bioavailability of poorly absorbed drugs. Adv Drug Deliv Rev. 2012;64(6):480–95.
Shi NQ, Zhang Y, Li Y, Lai HW, Xiao X, Feng B, et al. Self-micellizing solid dispersions enhance the properties and therapeutic potential of fenofibrate: advantages, profiles and mechanisms. Int J Pharm. 2017;528(1–2):563–77.
Xu S, Dai WG. Drug precipitation inhibitors in supersaturable formulations. Int J Pharm. 2013;453(1):36–43.
Liu C, Chen Z, Chen Y, Lu J, Li Y, Wang S, et al. Improving oral bioavailability of sorafenib by optimizing the "spring" and "parachute" based on molecular interaction mchanisms. Mol Pharm. 2016;13(2):599–608.
Sun DD, Lee PI. Evolution of supersaturation of amorphous pharmaceuticals: nonlinear rate of supersaturation generation regulated by matrix diffusion. Mol Pharm. 2015;12(4):1203–15.
Turnbull D, Fischer JC. Rate of nucleation in condensed systems. J Chem. Physics. 1949;17:71–3.
Schver GCRM, Lee PI. Combined effects of supersaturation rates and doses on the kinetic-solubility profiles of amorphous solid dispersions based on water-insoluble poly(2-hydroxyethyl methacrylate) hydrogels. Mol Pharm. 2018;15(5):2017–26.
Taylor LS, Zhang GGZ. Physical chemistry of supersaturated solutions and implications for oral absorption. Adv Drug Deliv Rev. 2016;101:122–42.
Ueda K, Higashi K, Yamamoto K, Moribe K. Equilibrium state at supersaturated drug concentration achieved by hydroxypropyl methylcellulose acetate succinate: molecular characterization using (1)H NMR technique. Mol Pharm. 2015;12(4):1096–104.
Ueda K, Higashi K, Kataoka M, Yamashita S, Yamamoto K, Moribe K. Inhibition mechanism of hydroxypropyl methylcellulose acetate succinate on drug crystallization in gastrointestinal fluid and drug permeability from a supersaturated solution. Eur J Pharm Sci. 2014;62:293–300.
Funding
This work was supported by Scientific Research Foundation of the Education Department of Jilin Province of China (No. 2015-401), Science and Technology Development Program of Jilin Province of China (Nos. 20160520046JH and 20140203012YY), the National Natural Science Foundation of China (No. 81602654), Science and Technology Development Program of Jilin City in Jilin Province of China (No. 201464053), the State Key Laboratory of Medicinal Chemical Biology of Nankai University (No. 201503001), and China Postdoctoral Science Foundation (No. 2015M571373).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shi, NQ., Jin, Y., Zhang, Y. et al. The Influence of Cellulosic Polymer’s Variables on Dissolution/Solubility of Amorphous Felodipine and Crystallization Inhibition from a Supersaturated State. AAPS PharmSciTech 20, 12 (2019). https://doi.org/10.1208/s12249-018-1266-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-018-1266-y