Abstract
It is now recognized that a number of excipients previously considered to be “inert” have the capacity to alter drug oral bioavailability through a range of in vivo effects. The various mechanisms through which an excipient can affect in vivo gastrointestinal physiology and drug absorption characteristics were explored in “A Critical Overview of The Biological Effects of Excipients (Part I): Impact on Gastrointestinal Absorption.” The next critical issue that needs to be discussed is how these biological effects are evaluated. Therefore, in Part 2 of this critical overview, the in vitro, in vivo, and in silico methods for evaluating excipient effects are considered. Examples are provided to illustrate how such studies employing these various procedures have been used to promote formulation understanding and optimization. Finally, a discussion of how the Center for Drug Evaluation and Research applies these tools to support biowaivers is provided.
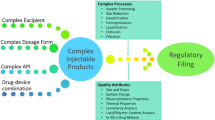
Graphical Abstract


Similar content being viewed by others
References
Brouwers J, Brewster ME, Augustijns P. Supersaturating drug delivery systems: the answer to solubility-limited oral bioavailability? J Pharm Sci. 2009;98:2549–72.
Ricarte RG, Van Zee NJ, Li Z, Johnson LM, Lodge TP, Hillmyer MA. Recent advances in understanding the micro- and nanoscale phenomena of amorphous solid dispersions. Mol Pharm American Chemical Society. 2019;16:4089–103.
Thakral NK, Meister E, Jankovsky C, Li L, Schwabe R, Luo L, et al. Prediction of in vivo supersaturation and precipitation of poorly water-soluble drugs: achievements and aspirations. Int J Pharm. 2021;600: 120505.
Ashwathy P, Anto AT, Sudheesh MS. A mechanistic review on the dissolution phase behavior and supersaturation stabilization of amorphous solid dispersions. Drug Dev Ind Pharm. Taylor & Francis; 2021;47:1–11.
Wilson VR, Mugheirbi NA, Mosquera-Giraldo LI, Deac A, Moseson DE, Smith DT, et al. Interaction of polymers with enzalutamide nanodroplets—impact on droplet properties and induction times. Mol Pharm American Chemical Society. 2021;18:836–49.
Ueda K, Hate SS, Taylor LS. Impact of hypromellose acetate succinate grade on drug amorphous solubility and in vitro membrane transport. J Pharm Sci. 2020;109:2464–73.
Ueda K, Moseson DE, Pathak V, Taylor LS. Effect of polymer species on maximum aqueous phase supersaturation revealed by quantitative nuclear magnetic resonance spectroscopy. Mol Pharm American Chemical Society. 2021;18:1344–55.
Price DJ, Ditzinger F, Koehl NJ, Jankovic S, Tsakiridou G, Nair A, et al. Approaches to increase mechanistic understanding and aid in the selection of precipitation inhibitors for supersaturating formulations - a PEARRL review. J Pharm Pharmacol. 2019;71:483–509.
Feeney OM, Crum MF, McEvoy CL, Trevaskis NL, Williams HD, Pouton CW, et al. 50years of oral lipid-based formulations: provenance, progress and future perspectives. Adv Drug Deliv Rev. 2016;101:167–94.
Stewart A, Yates I, Mudie D, Pivette P, Goodwin A, Sarmiento A, et al. Mechanistic study of belinostat oral absorption from spray-dried dispersions. J Pharm Sci. 2019;108:326–36.
Saboo S, Kestur US, Flaherty DP, Taylor LS. Congruent release of drug and polymer from amorphous solid dispersions: insights into the role of drug-polymer hydrogen bonding, surface crystallization, and glass transition. Mol Pharm. 2020;17:1261–75.
Harmon P, Galipeau K, Xu W, Brown C, Wuelfing WP. Mechanism of dissolution-induced nanoparticle formation from a copovidone-based amorphous solid dispersion. Mol Pharm. 2016;13:1467–81.
Kesisoglou F, Wang M, Galipeau K, Harmon P, Okoh G, Xu W. Effect of amorphous nanoparticle size on bioavailability of anacetrapib in dogs. J Pharm Sci. 2019;108:2917–25.
Pollard J, Rajabi-Siahboomi A, Badhan RKS, Mohammed AR, Perrie Y. High-throughput screening of excipients with a biological effect: a kinetic study on the effects of surfactants on efflux-mediated transport. J Pharm Pharmacol. 2019;71:889–97.
https://www.accessdata.fda.gov/drugsatfda_docs/nda/2019/213051Orig1s000PharmR.pdf. Accessed 23rd June 2021.
Lewis AL, Mcentee N, Holland J, Patel A. Development and approval of rybelsus (oral semaglutide): ushering in a new era in peptide delivery. Drug Deliv Transl Res. 2021;
Ohtsu Y, Gibbons JA, Suzuki K, Fitzsimmons ME, Nozawa K, Arai H. Absorption, distribution, metabolism, and excretion of the androgen receptor inhibitor enzalutamide in rats and dogs. Eur J Drug Metab Pharmacokinet. 2017;42:611–26.
Kádár S, Tőzsér P, Nagy B, Farkas A, Nagy, K. Z, Tsinman O, et al. Flux-based formulation development—a proof of concept study. AAPS J. 2022;24.
Bajaj R, Chong LB, Zou L, Tsakalozou E, Ni Z, Giacomini KM, et al. Interaction Of commonly used oral molecular excipients with P-glycoprotein. AAPS J. 2021;23:106.
Metry M, Polli JE. Evaluation of excipient risk in BCS class I and III biowaivers. AAPS J. 2022;24:1–11.
Yang Y, Zhao Y, Yu A, Sun D, Yu LX. Chapter 12: oral drug absorption: evaluation and prediction. Dev Solid Oral Dos Forms Pharm Theory Pract Second Ed. 2017. p. 331–54.
Cummins CL, Salphati L, Reid MJ, Benet LZ. In vivo modulation of intestinal CYP3A metabolism by P-glycoprotein: studies using the rat single-pass intestinal perfusion model. J Pharmacol Exp Ther. 2003;305:306–14.
Grass M. Selecting in vitro dissolution tests for bioavailability enhancing oral formulations. American Pharmaceutical Review, October 15, 2017.
Mudie DM, Samiei N, Marshall DJ, Amidon GE, Bergström CAS. Selection of in vivo predictive dissolution media using drug substance and physiological properties. Aaps j. 2020;22:34.
O’Dwyer PJ, Box KJ, Dressman J, Griffin BT, Henze LJ, Litou C, et al. Oral biopharmaceutics tools: recent progress from partnership through the Pharmaceutical Education and Research with Regulatory Links collaboration. J Pharm Pharmacol. 2021;73:437–46.
Grignard E, Taylor R, McAllister M, Box K, Fotaki N. Considerations for the development of in vitro dissolution tests to reduce or replace preclinical oral absorption studies. Eur J Pharm Sci. 2017;99:193–201.
Gadgil P, Alleyne C, Feng KI, Hu M, Gindy M, Buevich AV, et al. Assessing the utility of in vitro screening tools for predicting bio-performance of oral peptide delivery. Pharm Res. 2019;36:151.
Fedi A, Vitale C, Ponschin G, Ayehunie S, Fato M, Scaglione S. In vitro models replicating the human intestinal epithelium for absorption and metabolism studies: a systematic review. J Control Release. 2021;335:247–68.
Hubatsch I, Ragnarsson EGE, Artursson P. Determination of drug permeability and prediction of drug absorption in Caco-2 monolayers. Nat Protoc. 2007;2:2111–9.
Twarog C, Liu K, O’Brien PJ, Dawson KA, Fattal E, Illel B, et al. A head-to-head Caco-2 assay comparison of the mechanisms of action of the intestinal permeation enhancers: SNAC and sodium caprate (C 10). Eur J Pharm Biopharm. 2020;152:95–107.
Lundquist P, Artursson P. Oral absorption of peptides and nanoparticles across the human intestine: opportunities, limitations and studies in human tissues. Adv Drug Deliv Rev. 2016;106:256–76.
Maher S, Heade J, McCartney F, Waters S, Bleiel SB, Brayden DJ. Effects of surfactant-based permeation enhancers on mannitol permeability, histology, and electrogenic ion transport responses in excised rat colonic mucosae. Int J Pharm. 2018;539:11–22.
McCartney F, Rosa M, Brayden DJ. Evaluation of sucrose laurate as an intestinal permeation enhancer for macromolecules: ex vivo and in vivo studies. Pharmaceutics. 2019;11:565.
Sjögren E, Eriksson J, Vedin C, Breitholtz K, Hilgendorf C. Excised segments of rat small intestine in Ussing chamber studies: a comparison of native and stripped tissue viability and permeability to drugs. Int J Pharm. 2016;505:361–8.
Fattah S, Ismaiel M, Murphy B, Rulikowska A, Frias JM, Winter DC, et al. Salcaprozate sodium (SNAC) enhances permeability of octreotide across isolated rat and human intestinal epithelial mucosae in Ussing chambers. Eur J Pharm Sci. 2020;154.
von Erlach T, Saxton S, Shi Y, Minahan D, Reker D, Javid F, et al. Robotically handled whole-tissue culture system for the screening of oral drug formulations. Nat Biomed Eng. 2020;4:544–59.
Wuyts B, Riethorst D, Brouwers J, Tack J, Annaert P, Augustijns P. Evaluation of fasted and fed state simulated and human intestinal fluids as solvent system in the Ussing chambers model to explore food effects on intestinal permeability. Int J Pharm. 2015;478:736–44.
Riethorst D, Brouwers J, Motmans J, Augustijns P. Human intestinal fluid factors affecting intestinal drug permeation in vitro. Eur J Pharm Sci. 2018;121:338–46.
Presas E, McCartney F, Sultan E, Hunger C, Nellen S, V. Alvarez C, et al. Physicochemical, pharmacokinetic and pharmacodynamic analyses of amphiphilic cyclodextrin-based nanoparticles designed to enhance intestinal delivery of insulin. J Control release. 2018;286:402–14.
Taverner A, Dondi R, Almansour K, Laurent F, Owens SE, Eggleston IM, et al. Enhanced paracellular transport of insulin can be achieved via transient induction of myosin light chain phosphorylation. J Control release. 2015;210:189–97.
Tuvia S, Pelled D, Marom K, Salama P, Levin-Arama M, Karmeli I, et al. A novel suspension formulation enhances intestinal absorption of macromolecules via transient and reversible transport mechanisms. Pharm Res. 2014;31:2010–21.
Thwala LN, Delgado DP, Leone K, Marigo I, Benetti F, Chenlo M, et al. Protamine nanocapsules as carriers for oral peptide delivery. J Control release. 2018;291:157–68.
Wang X, Maher S, Brayden DJ. Restoration of rat colonic epithelium after in situ intestinal instillation of the absorption promoter, sodium caprate. Ther Deliv. 2010;1:75–82.
Liu J, Werner U, Funke M, Besenius M, Saaby L, Fanø M, et al. SEDDS for intestinal absorption of insulin: application of Caco-2 and Caco-2/HT29 co-culture monolayers and intra-jejunal instillation in rats. Int J Pharm. 2019;560:377–84.
Dahlgren D, Roos C, Lundqvist A, Tannergren C, Sjöblom M, Sjögren E, et al. Time-dependent effects on small intestinal transport by absorption-modifying excipients. Eur J Pharm Biopharm. 2018;132:19–28.
Dahlgren D, Roos C, Johansson P, Tannergren C, Lundqvist A, Langguth P, et al. The effects of three absorption-modifying critical excipients on the in vivo intestinal absorption of six model compounds in rats and dogs. Int J Pharm. 2018;547:158–68.
Dahlgren D, Sjöblom M, Lennernäs H. Intestinal absorption-modifying excipients: a current update on preclinical in vivo evaluations. Eur J Pharm Biopharm. 2019;142:411–20.
Hagio M, Matsumoto M, Fukushima M, Hara H, Ishizuka S. Improved analysis of bile acids in tissues and intestinal contents of rats using LC/ESI-MS s⃞. J Lipid Res. 2009;50:173–80.
Fancher RM, Zhang H, Sleczka B, Derbin G, Rockar R, Marathe P. Development of a canine model to enable the preclinical assessment of Ph-dependent absorption of test compounds. J Pharm Sci. 2011;100:2979–88.
Hatton GB, Yadav V, Basit AW, Merchant HA. Animal farm: considerations in animal gastrointestinal physiology and relevance to drug delivery in humans. J Pharm Sci. 2015;104:2747–76.
van de Waterbeemd H, Gifford E. ADMET in silico modelling: towards prediction paradise? Nat Rev Drug Discov. 2003;2:192–204.
Sugano K. Biopharmaceutics modeling and simulations theory, practice, methods and applications. Shizuoka, Japan: Wiley; 2012.
Chow EC, Talattof A, Tsakalozou E, Fan J, Zhao L, Zhang X. Using physiologically based pharmacokinetic (PBPK) modeling to evaluate the impact of pharmaceutical excipients on oral drug absorption: sensitivity analyses. AAPS J. 2016;18:1500–11.
Wu F, Cristofoletti R, Zhao L, Rostami-Hodjegan A. Scientific considerations to move towards biowaiver for biopharmaceutical classification system class III drugs: how modeling and simulation can help. Biopharm Drug Dispos. 2021;42:118–27.
Sugano K, Terada K. Rate- and extent-limiting factors of oral drug absorption: theory and applications. J Pharm Sci. 2015;104:2777–88.
Stewart AM, Grass ME. Practical approach to modeling the impact of amorphous drug nanoparticles on the oral absorption of poorly soluble drugs. Mol Pharm. 2020;17:180–9.
Mitra A, Zhu W, Kesisoglou F. Physiologically based absorption modeling for amorphous solid dispersion formulations. Mol Pharm. 2016;13:3206–15.
Avdeef A. Absorption and drug development: solubility, permeability, and charge state. 2nd ed. United States: John Wiley and Sons; 2012.
Mooney KG, Mintun MA, Himmelstein KJ, Stella VJ. Dissolution kinetics of carboxylic acids I: effect of pH under unbuffered conditions. J Pharm Sci Wiley Online Library. 1981;70:13–22.
Mooney KG, Mintun MA, Himmelstein KJ, Stella VJ. Dissolution kinetics of carboxylic acids II: effect of buffers. J Pharm Sci Wiley Online Library. 1981;70:22–32.
Krieg BJ, Taghavi SM, Amidon GL, Amidon GE. In vivo predictive dissolution: transport analysis of the CO2, bicarbonate in vivo buffer system. J Pharm Sci. 2014;103:3473–90.
Mudie DM, Amidon GL, Amidon GE. Physiological parameters for oral delivery and in vitro testing. Mol Pharm. 2010;7:1388–405.
Uekusa T, Sugano K. Effect of buffer capacity on dissolution and supersaturation profiles of poorly soluble drug salt. APSJT Annu Meet. Toyama; 2019. p. 236.
Galia E, Nicolaides E, Hörter D, Löbenberg R, Reppas C, Dressman JB. Evaluation of various dissolution media for predicting in vivo performance of class I and II drugs. Pharm Res. 1998;15:698–705.
Sugano K, Okazaki A, Sugimoto S, Tavornvipas S, Omura A, Mano T. Solubility and dissolution profile assessment in drug discovery. Drug Metab Pharmacokinet. 2007;22:225–54.
Okazaki A, Mano T, Sugano K. Theoretical dissolution model of poly-disperse drug particles in biorelevant media. J Pharm Sci. 2007;97.
Amidon GE, Higuchi WI, Ho NFH. Theoretical and experimental studies of transport of micelle-solubilized solutes. J Pharm Sci. 1982;71:77–84.
Poelma FG, Breäs R, Tukker JJ, Crommelin DJ. Intestinal absorption of drugs. The influence of mixed micelles on on the disappearance kinetics of drugs from the small intestine of the rat. J Pharm Pharmacol. 1991;43:317–24.
Yamaguchi T, Ikeda C, Sekine Y. Intestinal absorption of $β$-adrenergic blocking agent nadolol. I.: Comparison of absorption behavior of nadolol with those of other $β$-blocking agents in rats. Chem Pharm Bull. 1986;34:3362–9.
Ingels F, Beck B, Oth M, Augustijns P. Effect of simulated intestinal fluid on drug permeability estimation across Caco-2 monolayers. Int J Pharm. 2004;274:221–32.
Döppenschmitt S, Langguth P, Regårdh CG, Andersson TB, Hilgendorf C, Spahn-Langguth H. Characterization of binding properties to human P-glycoprotein: development of a [3H]verapamil radioligand-binding assay. J Pharmacol Exp Ther. 1999;288:348–57.
Lennernäs H, Regårdh C-G. Evidence for an interaction between the $β$-blocker pafenolol and bile salts in the intestinal lumen of the rat leading to dose-dependent oral absorption and double peaks in the plasma concentration–time profile. Pharm Res Springer. 1993;10:879–83.
Akiyama Y, Ito S, Fujita T, Sugano K. Prediction of negative food effect induced by bile micelle binding on oral absorption of hydrophilic cationic drugs. Eur J Pharm Sci. 2020;155.
Sugano K. Estimation of effective intestinal membrane permeability considering bile micelle solubilisation. Int J Pharm. 2009;368.
Oh DM, Curl RL, Amidon GL. Estimating the fraction dose absorbed from suspension of poorly soluble compounds in humans- Amidon- 1993.pdf. Pharm Res. 1993;10:264–70.
Fagerholm U, Lindahl A, Lennernäs H. Regional intestinal permeability in rats of compounds with different physicochemical properties and transport mechanisms. J Pharm Pharmacol Oxford University Press. 1997;49:687–90.
Sutton SC, Evans LA, Fortner JH, McCarthy JM, Sweeney K. Dog colonoscopy model for predicting human colon absorption. Pharm Res. 2006;23:1554–63.
Yamane M, Matsui K, Sugihara M, Tokunaga Y. The provisional no-effect threshold of sugar alcohols on oral drug absorption estimated by physiologically based biopharmaceutics model. J Pharm Sci: Elsevier; 2020.
Ichijo K, Oda R, Ishihara M, Okada R, Moteki Y, Funai Y, et al. Osmolality of orally administered solutions influences luminal water volume and drug absorption in intestine. J Pharm Sci Elsevier. 2017;106:2889–94.
Biancheria A, Kegeles G. Diffusion measurements in aqueous solutions of different viscosities. J Am Chem Soc ACS Publications. 1957;79:5908–12.
Yu LX. An integrated model for determining causes of poor oral drug absorption. Pharm. Res. 1999. p. 1883–7.
Sawamoto T, Haruta S, Kurosaki Y, Higaki K, Kimura T. Prediction of the plasma concentration profiles of orally administered drugs in rats on the basis of gastrointestinal transit kinetics and absorbability. J Pharm Pharmacol. 1997;49:450–7.
Yu A, Jackson T, Tsume Y, Koenigsknecht M, Wysocki J, Marciani L, et al. Mechanistic fluid transport model to estimate gastrointestinal fluid volume and its dynamic change over time. AAPS J Springer. 2017;19:1682–90.
Schiller C, Fröhlich CP, Giessmann T, Siegmund W, Mönnikes H, Hosten NWW. Intestinal fluid volumes and transit of dosage forms as assessed by magnetic resonance imaging. Aliment Pharmacol Ther. 2005;22:971–9.
Mudie DM, Amidon GL, Amidon GE, Murray K, Hoad CL, Pritchard SE, et al. Quantification of gastrointestinal liquid volumes and distribution following a 240 mL dose of water in the fasted state. Mol Pharm. 2014;11:3039–47.
Johnson KC. Mechanistic modeling of gastrointestinal motility with integrated dissolution for simulating drug absorption. ADMET DMPK. Me{\dj}unarodna udruga fizikalnih kemičara; 2020;8:314–24.
Sugano K. Aqueous boundary layers related to oral absorption of a drug: from dissolution of a drug to carrier mediated transport and intestinal wall metabolism. Mol Pharm. 2010;7:1362–73.
Higuchi M, Yoshihashi Y, Tarada K, Sugano K. Minimum rotation speed to prevent coning phenomena in compendium paddle dissolution apparatus. Eur J Pharm Sci. Elsevier B.V.; 2014;65:74–8.
Adson A, Burton PS, Raub TJ, Barsuhn CL, Audus KL, Ho NFH. Passive diffusion of weak organic electrolytes across Caco-2 cell monolayers: uncoupling the contributions of hydrodynamic, transcellular, and paracellular barriers. J Pharm Sci Elsevier. 1995;84:1197–204.
Sugano K, Takata N, Machida M, Saitoh K, Terada K. Prediction of passive intestinal absorption using bio-mimetic artificial membrane permeation assay and the paracellular pathway model. Int J Pharm. 2002;241.
Avdeef A, Tam KY. How well can the caco-2/madin-darby canine kidney models predict effective human jejunal permeability? J Med Chem. 2010;53:3566–84.
Heikkinen AT, Mönkkönen J, Korjamo T. Determination of permeation resistance distribution in in vitro cell monolayer permeation experiments. Eur J Pharm Sci. 2010;40:132–42.
Tachibana T, Kitamura S, Kato M, Mitsui T, Shirasaka Y, Yamashita S, et al. Model analysis of the concentration-dependent permeability of P-gp substrates. Pharm Res Springer. 2010;27:442–6.
Sugano K, Shirasaka Y, Yamashita S. Estimation of Michaelis-Menten constant of efflux transporter considering asymmetric permeability. Int J Pharm. 2011;418.
Porat D, Dahan A. Active intestinal drug absorption and the solubility-permeability interplay. Int J Pharm. 2018;537:84–93.
Chen Y, Ma F, Jones NS, Yoshida K, Chiang PC, Durk MR, et al. Physiologically-based pharmacokinetic model-informed drug development for fenebrutinib: understanding complex drug-drug interactions. CPT Pharmacometrics Syst Pharmacol. 2020;9:332–41.
Yamane M, Matsui K, Sugihara M, Tokunaga Y. The provisional no-effect threshold of sugar alcohols on oral drug absorption estimated by physiologically based biopharmaceutics model. J Pharm Sci. 2021;110:467–77.
McFeely SJ, Yu J, Wang Y, Wu C, Ragueneau-Majlessi I. Excipient knowledgebase: development of a comprehensive tool for understanding the disposition and interaction potential of common excipients. CPT Pharmacometrics Syst Pharmacol. 2021;10:953–61.
Zou L, Pottel J, Khuri N, Ngo HX, Ni Z, Tsakalozou E, et al. Interactions of oral molecular excipients with breast cancer resistance protein. BCRP Mol Pharm. 2020;17:748–56.
Zou L, Spanogiannopoulos P, Pieper LM, Chien HC, Cai W, Khuri N, et al. Bacterial metabolism rescues the inhibition of intestinal drug absorption by food and drug additives. Proc Natl Acad Sci U S A. 2020;117:16009–18.
U.S.: Food and Drug Administration. Guidance for industry: waiver of in vivo bioavailability and bioequivalence studies for immediate release solid oral dosage forms based on a biopharmaceutical classification system. 2017.
U.S.: Food and Drug Administration. Guidance on hydroxychloroquine sulfate. Recommended Apr 2011, Finalized Apr 2020.
U.S.: Food and Drug Administration. FY2021 GDUFA science and research report. Accessed in March, 2022. Available from: https://www.fda.gov/drugs/generic-drugs/fy-2021-gdufa-science-and-research-report
U.S.: Food and Drug Administration. Generic drug research priorities & projects. Accessed in December, 2021. Available from: https://www.fda.gov/drugs/generic-drugs/generic-drug-research-priorities-projects
Malkov D, Wang HZ, Dinh S, Gomez-Orellana I. Pathway of oral absorption of heparin with sodium N-[8-(2-hydroxybenzoyl)amino] caprylate. Pharm Res. 2002;19:1180–4.
Gleeson JP, Frías JM, Ryan SM, Brayden DJ. Sodium caprate enables the blood pressure-lowering effect of Ile-Pro-Pro and Leu-Lys-Pro in spontaneously hypertensive rats by indirectly overcoming PepT1 inhibition. Eur J Pharm Biopharm. 2018;128:179–87.
Tomita M, Doi N, Hayashi M. Effects of acylcarnitines on efflux transporting system in Caco-2 cell monolayers. Eur J Drug Metab Pharmacokinet. 2010;35:1–7.
Alvi MM, Chatterjee P. A prospective analysis of co-processed non-ionic surfactants in enhancing permeability of a model hydrophilic drug. AAPS PharmSciTech. 2014;15:339–53.
Raimondi F, Santoro P, Barone MV, Pappacoda S, Barretta ML, Nanayakkara M, et al. Bile acids modulate tight junction structure and barrier function of Caco-2 monolayers via EGFR activation. Am J Physiol Gastrointest Liver Physiol. 2008;294.
Söderholm JD, Öman H, Blomquist L, Veen J, Lindmark T, Olaison G. Reversible increase in tight junction permeability to macromolecules in rat ileal mucosa in vitro by sodium caprate, a constituent of milk fat. Dig Dis Sci. 1998;43:1547–52.
Lecluyse EL, Sutton SC, Fix JA. In vitro effects of long-chain acylcarnitines on the permeability, transepithelial electrical resistance and morphology of rat colonic mucosa. J Pharmacol Exp Ther. 1993;265:955–62.
McCartney F, Jannin V, Chevrier S, Boulghobra H, Hristov DR, Ritter N, et al. Labrasol® is an efficacious intestinal permeation enhancer across rat intestine: ex vivo and in vivo rat studies. J Control Release. 2019;310:115–26.
Brayden DJ, Stuettgen V. Sodium glycodeoxycholate and sodium deoxycholate as epithelial permeation enhancers: in vitro and ex vivo intestinal and buccal bioassays. Eur J Pharm Sci. 2021;159: 105737.
Brayden D, Creed E, O’Connell A, Leipold H, Agarwal R, Leone-Bay A. Heparin absorption across the intestine: effects of sodium N-[8-(2-hydroxybenzoyl)amino]caprylate in rat in situ intestinal instillations and in Caco-2 monolayers. Pharm Res. 1997;14:1772–9.
Tomita M, Sawada T, Ogawa T, Ouchi H, Hayashi M, Awazu S. Differences in the enhancing effects of sodium caprate on colonic and jejunal drug absorption. Pharm Res. 1992;9:648–53.
Sutton SC, LeCluyse EL, Cammack L, Fix JA. Enhanced bioavailability of cefoxitin using palmitoyl L-carnitine. I. Enhancer activity in different intestinal regions. Pharm Res. 1992;9:191–4.
Koga K, Kawashima S, Murakami M. In vitro and in situ evidence for the contribution of Labrasol and Gelucire 44/14 on transport of cephalexin and cefoperazone by rat intestine. Eur J Pharm Biopharm. 2002;54:311–8.
Fricker G, Fahr A, Beglinger C, Kissel T, Reiter G, Drewe J. Permeation enhancement of octreotide by specific bile salts in rats and human subjects: in vitro, in vivo correlations. Br J Pharmacol. 1996;117:217–23.
Dahlgren D, Roos C, Lundqvist A, Tannergren C, Langguth P, Sjöblom M, et al. Preclinical effect of absorption modifying excipients on rat intestinal transport of model compounds and the mucosal barrier marker 51 Cr-EDTA. Mol Pharm. 2017;14:4243–51.
Ates M, Kaynak MS, Sahin S. Effect of permeability enhancers on paracellular permeability of acyclovir. J Pharm Pharmacol. 2016;68:781–90.
Dahlgren D, Sjöblom M, Hedeland M, Lennernäs H. The in vivo effect of transcellular permeation enhancers on the intestinal permeability of two peptide drugs enalaprilat and hexarelin. Pharmaceutics. 2020;12:99.
Zhou W, Di LQ, Wang J, Shan JJ, Liu SJ, Ju WZ, et al. Intestinal absorption of forsythoside A in in situ single-pass intestinal perfusion and in vitro Caco-2 cell models. Acta Pharmacol Sin. 2012;33:1069–79.
Shen Y, Lu Y, Jv M, Hu J, Li Q, Tu J. Enhancing effect of Labrasol on the intestinal absorption of ganciclovir in rats. Drug Dev Ind Pharm. 2011;37:1415–21.
Gao H, Wang M, Sun D, Sun S, Sun C, Liu J, et al. Evaluation of the cytotoxicity and intestinal absorption of a self-emulsifying drug delivery system containing sodium taurocholate. Eur J Pharm Sci. 2017;106:212–9.
Author information
Authors and Affiliations
Contributions
Manuscript conceptualization: Marilyn Martinez, Fang Wu, and Balint Sinko.
Manuscript development lead: Marilyn Martinez.
Manuscript development co-leads: Fang Wu and Balint Sinko.
Introduction: Marilyn Martinez, Fang Wu, Balint Sinko, David Brayden, Aaron Stewart, and Michael Glass.
In vitro test selection for bioavailability-enhancing formulations: David J. Brayden, Michael Grass, and Aaron Stewart.
Using in silico models of API-excipient interactions to inform formulation development: Filippos Kesisoglou.
Considerations for the development of predictive models describing the impact of excipients on the rate and extent of oral drug absorption: Michael Grass, Aaron Stewart, and Kiyohiko Sugano.
How might excipients impact bioequivalence assessments of human generic drug products: Fang Wu.
Conclusion: Marilyn Martinez, Fang Wu, and Balint Sinko.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no relevant financial or non-financial interests to disclose.
Disclaimer
The contents of this manuscript reflect the views of the authors and should not be construed to represent FDA’s views or policies.
Additional information
Guest Editors: Marilyn N. Martinez, Balint Sinko and Fang Wu.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Marilyn N. Martinez, Fang Wu, and Balint Sinko are co-editors for the theme issue on “The Biological Effects of Excipients.”.
Rights and permissions
About this article
Cite this article
Martinez, M.N., Wu, F., Sinko, B. et al. A Critical Overview of the Biological Effects of Excipients (Part II): Scientific Considerations and Tools for Oral Product Development. AAPS J 24, 61 (2022). https://doi.org/10.1208/s12248-022-00713-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-022-00713-1