Abstract
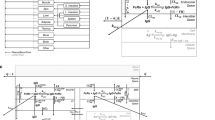
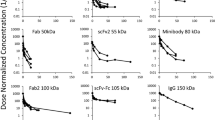
Here, we have investigated the effect of size of protein therapeutics on brain pharmacokinetics (PK) following systemic administration in rats. All tested proteins were derived from trastuzumab that do not bind to any targets in rats. PK data generated with F(ab)2 (100 kDa), Fab (50 kDa), and scFv (27 kDa) fragments of trastuzumab, along with published PK data for FcRn non-binding and wild-type trastuzumab (150 kDa), were used to establish a relationship between the protein size and brain exposure. A large-pore microdialysis system was used to measure the PK of proteins in the plasma, the interstitial fluid (ISF) at the striatum (ST), and the cerebrospinal fluid (CSF) at the lateral ventricle (LV) and cisterna magna (CM). Concentrations of all the proteins in plasma, brain homogenate, ISF, and CSF were measured using ELISA. When evaluating the effect of protein size in the absence of FcRn binding, we found a bell-shaped relationship between the size and ISF/plasma AUC ratio, where 100 kDa F(ab)2 demonstrated the highest exposure. A similar bell-shaped relationship was observed for the brain homogenate/plasma AUC ratio, with a peak at 50 kDa. The CSF/plasma AUC ratio at LV increased monotonously with a decrease in the size of proteins. We observed that the exposure of protein therapeutics in different regions of the brain could be significantly different and there could be optimal sizes of protein therapeutics to accomplish maximum/selective exposure in selected brain regions following systemic administration.
Graphical abstract







Similar content being viewed by others
Change history
24 May 2022
A Correction to this paper has been published: https://doi.org/10.1208/s12248-022-00718-w
Abbreviations
- BBB:
-
Blood-brain barrier
- BCSFB:
-
Blood-cerebrospinal fluid barrier
- CHO:
-
Chinese Hamster Ovary
- CM:
-
Cisterna magna
- CNS:
-
Central nervous system
- CSF:
-
Cerebrospinal fluid
- CSF(CM):
-
CSF at the CM
- CSF(LV):
-
CSF at the LV
- ELISA:
-
Enzyme-linked immunosorbent assay
- IgG:
-
Immunoglobulin G
- ISF:
-
Interstitial fluid
- ISF(ST):
-
ISF at ST
- IV:
-
Intravenous
- KD:
-
Dissociation constant
- LV:
-
Lateral ventricles
- mAbs:
-
Monoclonal antibodies
- PD:
-
Pharmacodynamic
- PK:
-
Pharmacokinetics
- RMT:
-
Receptor-mediated transcytosis
- sdAb:
-
Single-domain antibody
- ST:
-
Striatum
References
de Lange EC. Utility of CSF in translational neuroscience. J Pharmacokinet Pharmacodyn. 2013;40(3):315–26.
Pardridge WM. CSF, blood-brain barrier, and brain drug delivery. Expert Opin Drug Deliv. 2016;13(7):963–75.
Bryniarski MA, Ren T, Rizvi AR, Snyder AM, Morris ME. Targeting the choroid plexuses for protein drug delivery. Pharmaceutics. 2020;12(10).
Hurley JV, Anderson RM, Sexton PT. The fate of plasma protein which escapes from blood vessels of the choroid plexus of the rat–an electron microscope study. J Pathol. 1981;134(1):57–70.
Johnsen KB, Burkhart A, Thomsen LB, Andresen TL, Moos T. Targeting the transferrin receptor for brain drug delivery. Prog Neurobiol. 2019;181:101665.
Stanimirovic DB, Sandhu JK, Costain WJ. Emerging technologies for delivery of biotherapeutics and gene therapy across the blood-brain barrier. BioDrugs. 2018;32(6):547–59.
Chang HY, Wu S, Li Y, Zhang W, Burrell M, Webster CI, Shah DK. Brain pharmacokinetics of anti- transferrin receptor antibody affinity variants in rats determined using microdialysis. MAbs. 2021;13(1):1874121.
Finke JM, Banks WA. Modulators of IgG penetration through the blood-brain barrier: implications for Alzheimer’s disease immunotherapy. Hum Antibodies. 2017;25(3–4):131–46.
Poduslo JF, Ramakrishnan M, Holasek SS, Ramirez-Alvarado M, Kandimalla KK, Gilles EJ, Curran GL, Wengenack TM. In vivo targeting of antibody fragments to the nervous system for Alzheimer’s disease immunotherapy and molecular imaging of amyloid plaques. J Neurochem. 2007;102(2):420–33.
Tamura Y, Hamajima K, Matsui K, Yanoma S, Narita M, Tajima N, Xin KQ, Klinman D, Okuda K. The F(ab)’2 fragment of an Abeta-specific monoclonal antibody reduces Abeta deposits in the brain. Neurobiol Dis. 2005;20(2):541–9.
Wolak DJ, Thorne RG. Diffusion of macromolecules in the brain: implications for drug delivery. Mol Pharm. 2013;10(5):1492–504.
Thorne RG, Nicholson C. In vivo diffusion analysis with quantum dots and dextrans predicts the width of brain extracellular space. Proc Natl Acad Sci U S A. 2006;103(14):5567–72.
Pizzo ME, Wolak DJ, Kumar NN, Brunette E, Brunnquell CL, Hannocks MJ, Abbott NJ, Meyerand ME, Sorokin L, Stanimirovic DB, Thorne RG. Intrathecal antibody distribution in the rat brain: surface diffusion, perivascular transport and osmotic enhancement of delivery. J Physiol. 2018;596(3):445–75.
Pepinsky RB, Shao Z, Ji B, Wang Q, Meng G, Walus L, Lee X, Hu Y, Graff C, Garber E, Meier W, Mi S. Exposure levels of anti-LINGO-1 Li81 antibody in the central nervous system and dose-efficacy relationships in rat spinal cord remyelination models after systemic administration. J Pharmacol Exp Ther. 2011;339(2):519–29.
Farrington GK, Caram-Salas N, Haqqani AS, Brunette E, Eldredge J, Pepinsky B, Antognetti G, Baumann E, Ding W, Garber E, Jiang S, Delaney C, Boileau E, Sisk WP, Stanimirovic DB. A novel platform for engineering blood-brain barrier-crossing bispecific biologics. FASEB J. 2014;28(11):4764–78.
Wang Q, Delva L, Weinreb PH, Pepinsky RB, Graham D, Veizaj E, Cheung AE, Chen W, Nestorov I, Rohde E, Caputo R, Kuesters GM, Bohnert T, Gan LS. Monoclonal antibody exposure in rat and cynomolgus monkey cerebrospinal fluid following systemic administration. Fluids Barriers CNS. 2018;15(1):10.
Chang HY, Morrow K, Bonacquisti E, Zhang W, Shah DK. Antibody pharmacokinetics in rat brain determined using microdialysis. MAbs. 2018;10(6):843–53.
Chang HY, Wu S, Meno-Tetang G, Shah DK. A translational platform PBPK model for antibody disposition in the brain. J Pharmacokinet Pharmacodyn. 2019;46(4):319–38.
Levy G. Pharmacologic target-mediated drug disposition. Clin Pharmacol Ther. 1994;56(3):248–52.
Li Z, Li Y, Chang HP, Chang HY, Guo L, Shah DK. Effect of size on solid tumor disposition of protein therapeutics. Drug Metab Dispos. 2019;47(10):1136–45.
Hillman J, Aneman O, Anderson C, Sjogren F, Saberg C, Mellergard P. A microdialysis technique for routine measurement of macromolecules in the injured human brain. Neurosurgery. 2005;56(6):1264–1268; Discussion 1268–1270.
Trickler WJ, Miller DW. Use of osmotic agents in microdialysis studies to improve the recovery of macromolecules. J Pharm Sci. 2003;92(7):1419–27.
Jadhav SB, Khaowroongrueng V, Fueth M, Otteneder MB, Richter W, Derendorf H. Tissue distribution of a therapeutic monoclonal antibody determined by large pore microdialysis. J Pharm Sci. 2017;106(9):2853–9.
Jadhav SB, Khaowroongrueng V, Derendorf H. Microdialysis of large molecules. J Pharm Sci. 2016;105(11):3233–42.
Sjogren F, Svensson C, Anderson C. Technical prerequisites for in vivo microdialysis determination of interleukin-6 in human dermis. Br J Dermatol. 2002;146(3):375–82.
Rukwied R, Lischetzki G, McGlone F, Heyer G, Schmelz M. Mast cell mediators other than histamine induce pruritus in atopic dermatitis patients: a dermal microdialysis study. Br J Dermatol. 2000;142(6):1114–20.
Papoiu AD, Wang H, Nattkemper L, Tey HL, Ishiuji Y, Chan YH, Schmelz M, Yosipovitch G. A study of serum concentrations and dermal levels of NGF in atopic dermatitis and healthy subjects. Neuropeptides. 2011;45(6):417–22.
Diehl KH, Hull R, Morton D, Pfister R, Rabemampianina Y, Smith D, Vidal JM, van de Vorstenbosch C, European Federation of Pharmaceutical Industries A, European Centre for the Validation of Alternative M. A good practice guide to the administration of substances and removal of blood, including routes and volumes. J Appl Toxicol. 2001;21(1):15–23.
Nedelman JR, Gibiansky E, Lau DT. Applying Bailer’s method for AUC confidence intervals to sparse sampling. Pharm Res. 1995;12(1):124–8.
Motulsky H. Intuitive biostatistics: a nonmathematical guide to statistical thinking. New York: Oxford University Press; 2018.
Da Mesquita S, Fu Z, Kipnis J. The meningeal lymphatic system: a new player in neurophysiology. Neuron. 2018;100(2):375–88.
Louveau A, Plog BA, Antila S, Alitalo K, Nedergaard M, Kipnis J. Understanding the functions and relationships of the glymphatic system and meningeal lymphatics. J Clin Invest. 2017;127(9):3210–9.
Tamura R, Yoshida K, Toda M. Current understanding of lymphatic vessels in the central nervous system. Neurosurg Rev. 2020;43(4):1055–64.
Li Z, Krippendorff BF, Shah DK. Influence of molecular size on the clearance of antibody fragments. Pharm Res. 2017;34(10):2131–2141.
Acknowledgements
We thank Dr. Kristin Hill and Dr. Vivian Rodriguez-Cruz for their advice on in vivo catheterization surgery. We also thank Dr. Lena Medina (Instech infusion) for the advice on the blood collection. Finally, we thank Dr. Chunxia Qiao for the advice on the scFv plasmid and the pcDNA5_FRT plasmid.
Funding
This research was funded by the grant from the Center for Protein Therapeutics (CPT) at the University at Buffalo. DKS is also supported by National Institute of General Medical Sciences grant [GM114179], National Institute of Allergy and Infectious Diseases grant [AI138195], and National Cancer Institute grants [R01CA246785 and R01CA256928].
Author information
Authors and Affiliations
Contributions
Conceptualization: Dhaval K. Shah, Hsueh-Yuan Chang, Shengjia Wu.
ScFv expression in CHO cells: Leiming Guo.
Protein Purification: Hsueh-Yuan Chang, Yingyi Li, Leiming Guo.
In vivo investigation: Hsueh-Yuan Chang, Shengjia Wu, Yuelin Li.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary Video 1 (MOV 34.4 MB)
Supplementary Video 2 (MP4 2.79 MB)
Rights and permissions
About this article
Cite this article
Chang, HY., Wu, S., Li, Y. et al. Effect of the Size of Protein Therapeutics on Brain Pharmacokinetics Following Systematic Administration. AAPS J 24, 62 (2022). https://doi.org/10.1208/s12248-022-00701-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-022-00701-5