Abstract
Linagliptin demonstrates substantial nonlinear pharmacokinetics due to its saturable binding to its pharmacological target dipeptidyl peptide 4 (DPP-4), a phenomenon known as target-mediated drug disposition (TMDD). In the current study, we established a novel whole-body physiologically-based pharmacokinetic (PBPK)-TMDD model for linagliptin. This comprehensive model contains plasma and 14 tissue compartments, among which TMDD binding process was incorporated in 9 of them, namely the plasma, kidney, liver, spleen, lung, skin, salivary gland, thymus, and reproductive organs. Our final model adequately captured the concentration-time profiles of linagliptin in both plasma and various tissues in both wildtype rats and DPP4-deficient rats following different doses. The association rate constant (kon) in plasma and tissues were estimated to be 0.943 and 0.00680 nM−1 h−1, respectively, and dissociation rate constant (koff), in plasma and tissues were estimated to be 0.0698 and 0.00880 h−1, respectively. The binding affinity of linagliptin to DPP-4 (Kd) was predicted to be higher in plasma (0.0740 nM) than that in tissue (1.29 nM). When scaled up to a human, this model captured the substantial and complex nonlinear pharmacokinetic behavior of linagliptin in human adults that is characterized by less-than dose-proportional increase in plasma exposure, dose-dependent clearance and volume of distribution, as well as long terminal half-life with minimal accumulation after repeated doses. Our modeling work is not only novel but also of high significance as the whole-body PBPK-TMDD model platform developed using linagliptin as the model compound could be applied to other small-molecule compounds exhibiting TMDD to facilitate their optimal dose selection.

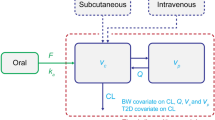
Graphical abstract





Similar content being viewed by others
References
Graefe-Mody U, Retlich S, Friedrich C. Clinical pharmacokinetics and pharmacodynamics of linagliptin. Clin Pharmacokinet. 2012;51(7):411–27.
Thomas L, Eckhardt M, Langkopf E, Tadayyon M, Himmelsbach F, Mark M. (R)-8-(3-amino-piperidin-1-yl)-7-but-2-ynyl-3-methyl-1-(4-methyl-quinazolin-2-ylmethyl)-3, 7-dihydro-purine-2, 6-dione (BI 1356), a novel xanthine-based dipeptidyl peptidase 4 inhibitor, has a superior potency and longer duration of action compared with other dipeptidyl peptidase-4 inhibitors. J Pharmacol Exp Ther. 2008;325(1):175–82.
Hartel S, Gossrau R, Hanski C, Reutter W. Dipeptidyl peptidase (DPP) IV in rat organs. Histochemistry. 1988;89(2):151–61.
Lankas GR, Leiting B, Roy RS, Eiermann GJ, Beconi MG, Biftu T, et al. Dipeptidyl peptidase IV inhibition for the treatment of type 2 diabetes: potential importance of selectivity over dipeptidyl peptidases 8 and 9. Diabetes. 2005;54(10):2988–94.
Elliott R, Morgan L, Tredger J, Deacon S, Wright J, Marks V. Glucagon-like peptide-1 (7–36) amide and glucose-dependent insulinotropic polypeptide secretion in response to nutrient ingestion in man: acute post-prandial and 24-h secretion patterns. J Endocrinol. 1993;138(1):159–66.
Nauck M, Bartels E, Orskov C, Ebert R, Creutzfeldt W. Additive insulinotropic effects of exogenous synthetic human gastric inhibitory polypeptide and glucagon-like peptide-1-(7-36) amide infused at near-physiological insulinotropic hormone and glucose concentrations. J Clin Endocrinol Metab. 1993;76(4):912–7.
Schwartz SL. Treatment of elderly patients with type 2 diabetes mellitus: a systematic review of the benefits and risks of dipeptidyl peptidase-4 inhibitors. Am J Geriatr Pharmacother. 2010;8(5):405–18.
Retlich S, Duval V, Ring A, Staab A, Hüttner S, Jungnik A, et al. Pharmacokinetics and pharmacodynamics of single rising intravenous doses (0.5 mg–10mg) and determination of absolute bioavailability of the dipeptidyl peptidase-4 inhibitor linagliptin (BI 1356) in healthy male subjects. Clin Pharmacokinet. 2010;49(12):829–40.
Heise T, Graefe-Mody E, Hüttner S, Ring A, Trommeshauser D, Dugi K. Pharmacokinetics, pharmacodynamics and tolerability of multiple oral doses of linagliptin, a dipeptidyl peptidase-4 inhibitor in male type 2 diabetes patients. Diabetes Obes Metab. 2009;11(8):786–94.
Horie Y, Kanada S, Watada H, Sarashina A, Taniguchi A, Hayashi N, et al. Pharmacokinetic, pharmacodynamic, and tolerability profiles of the dipeptidyl peptidase-4 inhibitor linagliptin: a 4-week multicenter, randomized, double-blind, placebo-controlled phase IIa study in Japanese type 2 diabetes patients. Clin Ther. 2011;33(7):973–89.
Hüttner S, Graefe-Mody E, Withopf B, Ring A, Dugi K. Safety, tolerability, pharmacokinetics, and pharmacodynamics of single oral doses of BI 1356, an inhibitor of dipeptidyl peptidase 4, in healthy male volunteers. J Clin Pharmacol. 2008;48(10):1171–8.
Retlich S, Withopf B, Greischel A, Staab A, Jaehde U, Fuchs H. Binding to dipeptidyl peptidase-4 determines the disposition of linagliptin (BI 1356)–investigations in DPP-4 deficient and wildtype rats. Biopharm Drug Dispos. 2009;30(8):422–36.
An G. Concept of pharmacologic target-mediated drug disposition in large-molecule and small-molecule compounds. J Clin Pharmacol. 2020;60(2):149–63. https://doi.org/10.1002/jcph.1545.
Levy G. Pharmacologic target-mediated drug disposition. Clin Pharmacol Ther. 1994;56(3):248–52.
Fuchs H, Tillement JP, Urien S, Greischel A, Roth W. Concentration-dependent plasma protein binding of the novel dipeptidyl peptidase 4 inhibitor BI 1356 due to saturable binding to its target in plasma of mice, rats and humans. J Pharm Pharmacol. 2009;61(1):55–62.
Fuchs H, Binder R, Greischel A. Tissue distribution of the novel DPP-4 inhibitor BI 1356 is dominated by saturable binding to its target in rats. Biopharm Drug Dispos. 2009;30(5):229–40.
Levy G, Mager DE, Cheung WK, Jusko WJ. Comparative pharmacokinetics of coumarin anticoagulants L: physiologic modeling of S-warfarin in rats and pharmacologic target-mediated warfarin disposition in man. J Pharm Sci. 2003;92(5):985–94.
Mager DE, Jusko WJ. General pharmacokinetic model for drugs exhibiting target-mediated drug disposition. J Pharmacokinet Pharmacodyn. 2001;28(6):507–32.
Volz A-K, Krause A, Haefeli WE, Dingemanse J, Lehr T. Target-mediated drug disposition pharmacokinetic–pharmacodynamic model of bosentan and endothelin-1. Clin Pharmacokinet. 2017;56(12):1499–511.
An G, Liu W, Katz DA, Marek GJ, Awni W, Dutta S. Population pharmacokinetics of the 11β-hydroxysteroid dehydrogenase type 1 inhibitor ABT-384 in healthy volunteers following single and multiple dose regimens. Biopharm Drug Dispos. 2014;35(7):417–29.
Wu N, Hammock B, Lee KSS, An G. Simultaneous target-mediated drug disposition (TMDD) model for two small-molecule compounds competing for their pharmacological target: soluble epoxide hydrolase. J Pharmacol Exp Ther. 2020;374:223–32. https://doi.org/10.1124/jpet.120.265330.
Tadayasu Y, Sarashina A, Tsuda Y, Tatami S, Friedrich C, Retlich S, et al. Population pharmacokinetic/pharmacodynamic analysis of the DPP-4 inhibitor linagliptin in Japanese patients with type 2 diabetes mellitus. J Pharm Pharm Sci. 2013;16(5):708–21.
Gerlowski LE, Jain RK. Physiologically based pharmacokinetic modeling: principles and applications. J Pharm Sci. 1983;72(10):1103–27. https://doi.org/10.1002/jps.2600721003.
Bi Y, Deng J, Murry DJ, An G. A whole-body physiologically based pharmacokinetic model of gefitinib in mice and scale-up to humans. AAPS J. 2016;18(1):228–38. https://doi.org/10.1208/s12248-015-9836-3.
Fuchs H, Runge F, Held H-D. Excretion of the dipeptidyl peptidase-4 inhibitor linagliptin in rats is primarily by biliary excretion and P-gp-mediated efflux. Eur J Pharm Sci. 2012;45(5):533–8.
Sarashina A, Sesoko S, Nakashima M, Hayashi N, Taniguchi A, Horie Y, et al. Linagliptin, a dipeptidyl peptidase-4 inhibitor in development for the treatment of type 2 diabetes mellitus: a phase I, randomized, double-blind, placebo-controlled trial of single and multiple escalating doses in healthy adult male Japanese subjects. Clin Ther. 2010;32(6):1188–204.
Blech S, Ludwig-Schwellinger E, Gräfe-Mody EU, Withopf B, Wagner K. The metabolism and disposition of the oral dipeptidyl peptidase-4 inhibitor, linagliptin, in humans. Drug Metab Dispos. 2010;38(4):667–78.
Delp MD, Evans MV, Duan C. Effects of aging on cardiac output, regional blood flow, and body composition in Fischer-344 rats. J Appl Physiol. 1998;85(5):1813–22.
Nagler RM, Baum BJ, Fox PC. Effects of X irradiation on the function of rat salivary glands at 3 and 40 days. Radiat Res. 1993;136(3):392–6.
Mobarak N, Alice Y. Lead distribution in the saliva and blood fractions of rats after intraperitoneal injections. Toxicology. 1984;32(1):67–74.
Davies B, Morris T. Physiological parameters in laboratory animals and humans. Pharm Res. 1993;10(7):1093–5.
Jansky L, Hart J. Cardiac output and organ blood flow in warm-and cold-acclimated rats exposed to cold. Can J Physiol Pharmacol. 1968;46(4):653–9.
Lee H, Blaufox M. Blood volume in the rat. J Nucl Med. 1985;26(1):72–6.
Valentin J. Basic anatomical and physiological data for use in radiological protection: reference values: ICRP publication 89. Ann ICRP. 2002;32(3–4):1–277.
Feher JJ. Quantitative human physiology: an introduction: academic press; 2017.
Tarhan S, Gümüs B, Gündüz İ, Ayyildiz V, Göktan C. Effect of varicocele on testicular artery blood flow in men color doppler investigation. Scand J Urol Nephrol. 2003;37(1):38–42.
Hurley PJ. Red cell and plasma volumes in normal adults. J Nucl Med. 1975;16(1):46–52.
Choi G-W, Lee Y-B, Cho H-Y. Interpretation of non-clinical data for prediction of human pharmacokinetic parameters: in vitro-in vivo extrapolation and allometric scaling. Pharmaceutics. 2019;11(4):168.
Kenyon EM. Interspecies extrapolation. Computational Toxicology: Springer; 2012. 501–20.
Yu Y, Fuscoe JC, Zhao C, Guo C, Jia M, Qing T, et al. A rat RNA-Seq transcriptomic body map across 11 organs and 4 developmental stages. Nat Commun. 2014;5(1):1–11.
van Waterschoot RAB, Parrott NJ, Olivares-Morales A, Lave T, Rowland M, Smith DA. Impact of target interactions on small-molecule drug disposition: an overlooked area. Nat Rev Drug Discov. 2018;17(4):299. https://doi.org/10.1038/nrd.2018.26.
An G. Small-molecule compounds exhibiting target-mediated drug disposition (TMDD): a minireview. J Clin Pharmacol. 2017;57(2):137–50.
An G, Liu W, Dutta S. Small-molecule compounds exhibiting target-mediated drug disposition—a case example of ABT-384. J Clin Pharmacol. 2015;55(10):1079–85.
Funding
This work is partially supported via University of Iowa Pharmaceutics Development Consortium.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Goodness fit plots for the final PBPK-TMDD modeling for linagliptin observed versus model-predicted in both wildtype and DPP4-deficient rat different tissues after 0.01, 0.1, 0.3, 1, 3, 10, and 50 mg/kg intravenous dose at 72 h. Yellow bars represent predicted linagliptin tissue concentration. Gray bars represent observed linagliptin tissue concentration
Rights and permissions
About this article
Cite this article
Wu, N., An, G. Incorporating Pharmacological Target-Mediated Drug Disposition (TMDD) in a Whole-Body Physiologically Based Pharmacokinetic (PBPK) Model of Linagliptin in Rat and Scale-up to Human. AAPS J 22, 125 (2020). https://doi.org/10.1208/s12248-020-00481-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-020-00481-w