Abstract
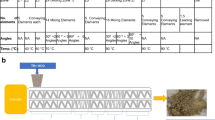
Existing dissolution chambers have relatively large volume compared to the size of the periodontal pocket. A small volume dissolution method that simulates the physiological release environment for periodontal drug delivery is needed. The objectives were to construct a small, more physiologically relevant, dissolution chamber and investigate the properties of the new dissolution chamber for the assessment of sustained drug release systems in periodontal delivery. Flow-through dissolution chambers were constructed using three-dimensional (3D) printing. Drug release experiments were performed using the dissolution chamber and a commercially available long-acting periodontal insert product, PerioChip®. Similar experiments were performed under more traditional larger volume bulk solution conditions for comparison. Computer simulations and experimental results showed that drug clearance from the dissolution chamber was fast compared to drug release from the periodontal product. Drug clearance from the flow-through dissolution chamber and drug release from the sustained release product in the chamber were related to the dissolution medium flow rate and chamber volume. Drug release in the flow-through chamber was slower than that observed in bulk solution, but approached it when the medium flow rate increased. The presence of trypsin in the dissolution medium enhanced drug release from the product. A flow-through dissolution system was constructed that could evaluate drug release from a sustained release product in a small dimension environment by modifying the flow rate and composition of the dissolution medium.







Similar content being viewed by others
References
Dressman JB, Amidon GL, Reppas C, Shah VP. Dissolution testing as a prognostic tool for oral drug absorption: immediate release dosage forms. Pharm Res. 1998;15:11–22.
Hermans A, Abend AM, Kesisoglou F, Flanagan T, Cohen MJ, Diaz DA, et al. Approaches for establishing clinically relevant dissolution specifications for immediate release solid oral dosage forms. AAPS J. 2017;19:1537–49.
Seidlitz A, Weitschies W. In-vitro dissolution methods for controlled release parenterals and their applicability to drug-eluting stent testing. J Pharm Pharmacol. 2012;64:969–85.
Dickinson PA, Lee WW, Stott PW, Townsend AI, Smart JP, Ghahramani P, et al. Clinical relevance of dissolution testing in quality by design. AAPS J. 2008;10:380–90.
Ghosh P, Milewski M, Paudel K. In vitro/in vivo correlations in transdermal product development. Ther Deliv. 2015;6:1117–24.
Friedman M, Golomb G. New sustained release dosage form of chlorhexidine for dental use. I. Development and kinetics of release. J Periodontal Res. 1982;17:323–8.
Golomb G, Friedman M, Soskolne A, Stabholz A, Sela MN. Sustained release device containing metronidazole for periodontal use. J Dent Res. 1984;63:1149–53.
Elkayam R, Friedman M, Stabholz A, Soskolne AW, Sela MN, Golub L. Sustained release device containing minocycline for local treatment of periodontal disease. J Control Release. 1988;7:231–6.
Steinberg D, Friedman M, Soskolne A, Sela MN. A new degradable controlled release device for treatment of periodontal disease: in vitro release study. J Periodontol. 1990;61:393–8.
Kassem AA, Ismail FA, Naggar VF, Aboulmagd E. Comparative study to investigate the effect of meloxicam or minocycline HCl in situ gel system on local treatment of periodontal pockets. AAPS PharmSciTech. 2014;15:1021–8.
Zupancic S, Potrc T, Baumgartner S, Kocbek P, Kristl J. Formulation and evaluation of chitosan/polyethylene oxide nanofibers loaded with metronidazole for local infections. Eur J Pharm Sci. 2016;95:152–60.
Khan G, Yadav SK, Patel RR, Nath G, Bansal M, Mishra B. Development and evaluation of biodegradable chitosan films of metronidazole and levofloxacin for the management of periodontitis. AAPS PharmSciTech. 2016;17:1312–25.
Yadav NK, Nanda S, Sharma G, Katare OP. Systematically optimized ketoprofen-loaded novel proniosomal formulation for periodontitis: in vitro characterization and in vivo pharmacodynamic evaluation. AAPS PharmSciTech. 2017;18:1863–80.
USP711. Dissolution. The United States Pharmacopeial Convention Pharmacopeial Forum. 2009.
USP724. Drug release. The United States Pharmacopeial Convention Pharmacopeial Forum. 2013.
Dexcel-Pharma-Technologies. PerioChip product insert. 2010.
Killoy WJ. The use of locally delivered chlorhexidine in the treatment of periodontitis. Clinical results. J Clin Periodontol. 1998;25:953–8.
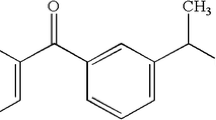
Murawsky M, Kelm GR, Kozak D, Qin B, Zou Y, Li SK. Influencing factors on gelatin matrix for chlorhexidine delivery. Drug Dev Ind Pharm. 2019;45:314–22.
Nassrawin NA. Changes in gingival crevicular fluid volume and flow rate during orthodontic treatment. J Dent Oral Implants. 2016;1:20–9.
Khurshid Z, Mali M, Naseem M, Najeeb S, Zafar MS. Human gingival crevicular fluids (GCF) proteomics: an overview. Dent J (Basel). 2017;5.
Misra DN. Interaction of chlorhexidine digluconate with and adsorption of chlorhexidine on hydroxyapatite. J Biomed Mater Res. 1994;28:1375–81.
Zeng P, Rao A, Wiedmann TS, Bowles W. Solubility properties of chlorhexidine salts. Drug Dev Ind Pharm. 2009;35:172–6.
Barry PH, Diamond JM. Effects of unstirred layers on membrane phenomena. Physiol Rev. 1984;64:763–872.
Siepmann J, Siepmann F. Mathematical modeling of drug dissolution. Int J Pharm. 2013;453:12–24.
Barros SP, Williams R, Offenbacher S, Morelli T. Gingival crevicular fluid as a source of biomarkers for periodontitis. Periodontol 2000. 2016;70:53–64.
Sorsa T, Tervahartiala T, Leppilahti J, Hernandez M, Gamonal J, Tuomainen AM, et al. Collagenase-2 (MMP-8) as a point-of-care biomarker in periodontitis and cardiovascular diseases. Therapeutic response to non-antimicrobial properties of tetracyclines. Pharmacol Res. 2011;63:108–13.
Jin L, Yu C, Corbet EF. Granulocyte elastase activity in static and flow gingival crevicular fluid. J Periodontal Res. 2003;38:303–10.
Araujo J. Evaluation of the ex vivo release profile of a long-acting biodegradable periodontal dosage form in a canine periodontal disease model. FDA Contract: HHSF223201510771P.
Soskolne WA, Chajek T, Flashner M, Landau I, Stabholtz A, Kolatch B, et al. An in vivo study of the chlorhexidine release profile of the PerioChip in the gingival crevicular fluid, plasma and urine. J Clin Periodontol. 1998;25:1017–21.
Goodson JM. Pharmacokinetic principles controlling efficacy of oral therapy. J Dent Res. 1989;68:1625–32.
Bickel M, Munoz JL, Giovannini P. Acid-base properties of human gingival crevicular fluid. J Dent Res. 1985;64:1218–20.
Acknowledgements
Funding for this project was made possible, in part, by the U.S. Food and Drug Administration (FDA) through a cooperative agreement (Research Award U01 FD005446). The views expressed in this paper do not reflect the official policies of the Department of Health and Human Services; nor does any mention of trade names, commercial practices, or organization imply endorsement by the United States Government. The authors thank Yuchan Yuan, Dr. Phillip Simmers, and Dr. Jason Heikenfeld for their assistance in 3D printing, Sarah R. Li for her help in the preliminary study of Comsol modeling, and Dr. Yuan Zou and Dr. Ross Walenga for helpful discussion.
Disclaimer
This article reflects the views of the authors and should not be construed to represent the U.S. Food and Drug Administration’s views or policies.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ren, W., Murawsky, M., La Count, T. et al. Dissolution Chamber for Small Drug Delivery System in the Periodontal Pocket. AAPS J 21, 51 (2019). https://doi.org/10.1208/s12248-019-0317-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-019-0317-y