Abstract
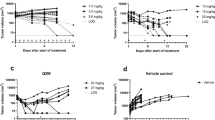
A single efficacy metric quantifying anti-tumor activity in xenograft models is useful in evaluating different tumors’ drug sensitivity and dose-response of an anti-tumor agent. Commonly used metrics include the ratio of tumor volume in treated vs. control mice (T/C), tumor growth inhibition (TGI), ratio of area under the curve (AUC), and growth rate inhibition (GRI). However, these metrics have some limitations. In particular, for biologics with long half-lives, tumor volume (TV) of treated xenografts displays a delay in volume reduction (and in some cases, complete regression) followed by a growth rebound. These observed data cannot be described by exponential functions, which is the underlying assumption of TGI and GRI, and the fit depends on how long the tumor volumes are monitored. On the other hand, T/C and TGI only utilizes information from one chosen time point. Here, we propose a new metric called Survival Prolongation Index (SPI), calculated as the time for drug-treated TV to reach a certain size (e.g., 600 mm3) divided by the time for control TV to reach 600mm3 and therefore not dependent on the chosen final time point tf. Simulations were conducted under different scenarios (i.e., exponential vs. saturable growth, linear vs. nonlinear kill function). For all cases, SPI is the most linear and growth-rate independent metric. Subsequently, a literature analysis was conducted using 11 drugs to evaluate the correlation between pre-clinically obtained SPI and clinical overall response. This retrospective analysis of approved drugs suggests that a predicted SPI of 2 is necessary for clinical response.







Similar content being viewed by others
References
Voskoglou-Nomikos T, Pater J, Seymour L. Clinical predictive value of the in vitro cell line, human xenograft, and mouse allograft preclinical cancer models. Clin Cancer Res. 2003;9:4227–39.
Lai Y, Wei X, Lin S, Qin L, Cheng L, Li P. Current status and perspectives of patient-derived xenograft models in cancer research. J Hematol Oncol. 2017;10:106.
Morgan K, Riedlinger G, Rosenfeld J, et al. Patient-derived xenograft models of non-small cell lung cancer and their potential utility in personalized medicine. Front Oncol. 2017;7:2.
Zhu A. Quantitative translational modeling to facilitate preclinical to clinical efficacy and toxicity translation in oncology. Future Sci OA. 2018;4:FSO306.
Simeoni M, Magni P, Cammia C, de Nicolao G, Croci V, Pesenti E, et al. Predictive pharmacokinetic-pharmacodynamic modeling of tumor growth kinetics in xenograft models after administration of anticancer agents. Cancer Res. 2004;64:1094–101.
Singh A, Shah D. Application of a PK-PD modeling and simulation-based strategy for clinical translation of antibody-drug conjugates: a case study with trastuzumab-emtansine (T-DM1). AAPS J. 2017;19:1054–70.
Haddish-Berhane N, Shah D, Ma D, et al. On translation of antibody drug conjugates efficacy from mouse experimental tumors to the clinic: a PK/PD approach. J Pharmacokinet Pharmacodyn. 2013;40:557–71.
Duan F, Simeone S, Wu R, Grady J, Mandoiu I, Srivastava PK. Area under the curve as a tool to measure kinetics of tumor growth in experimental animals. J Immunol Methods. 2012;382:224–8.
Judde J, Rebucci M, Vogt N, et al. Gefitinib and chemotherapy combination studies in five novel human non small cel lung cancer xenografts. Evidence linking EGFT signaling to gefitinib antitumor response. Int J Cancer. 2007;120:1579–90.
Wu W, Bi C, Credille KM, Manro JR, Peek VL, Donoho GP, et al. Inhibition of tumor growth and metastasis in non-small cell lung cancer by LY2801651, an inhibitor of several oncokinases, including MET. Clin Cancer Res. 2013;19:5699–710.
Hather G, Liu R, Bandi S, et al. Growth rate analysis and efficient experimental design for tumor xenograft studies. Cancer Informat. 2014;13(S4):65–72.
Jumbe N, Xin Y, Leipold D, et al. Modeling the efficacy of trastuzumab-DM1, an antibody drug conjugate, in mice. J Pharmacokinet Pharmacodyn. 2010;37:221–42.
Wong H, Choo E, Alicke B, et al. Antitumor activity of targeted and cytotoxic agents in murine subcutaneous tumor models correlates with clinical response. Clin Cancer Res. 2012;18:3846–55.
Perez E, Barrios C, Eiermann W, et al. Trastuzumab emtansine with or without pertuzumab versus trastuzumab plus taxane for human epidermal growth factor receptor 2-positive, advanced breast cancer: primary results from the phase III MARIANNE study. J Clin Oncol. 2017;35:141–8.
Siddik Z, Jones M, Boxall F, Harrap K. Comparative distribution and excretion of carboplatin and cisplatin in mice. Cancer Chemother Pharmacol. 1988;21:19–24.
Van Kuilenburg A, Maring J. Evaluation of 5-fluorouracil pharmacokinetic models and therapeutic drug monitoring in cancer patients. Pharmacogenomics. 2013;14:799–811.
Slaviero K, Clarke S, McLachlan A, et al. Population pharmacokinetics of weekly docetaxel in patients with advanced cancer. Br J Clin Pharm. 2003;57:44–53.
Demetri G, Russo P, MacPherson I, et al. Phase I dose-escalation and pharmacokinetic study of dasatinib in patients with advanced solid tumors. Clin Cancer Res. 2009;15:6232–40.
Lu T, Wang B, Gao Y, Dresser M, Graham RA, Jin JY. Semi-mechanism-based population pharmacokinetic modeling of the hedgehog pathway inhibitor vismodegib. CPT Pharmacometrics Syst Pharmacol. 2015;4:680–9.
Wu Q, Li M, Li H, Deng CH, Li L, Zhou TY, et al. Pharmacokinetic-pharmacodynamic modeling of the anticancer effect of erlotinib in a human non-small cell lung cancer xenograft mouse model. Acta Pharmacol Sin. 2013;34:1427–36.
Lu J, Eppler S, Wolf J, et al. Clinical pharmacokinetics of erlotinib in patients with solid tumors and and exposure-safety relationship in patients with non-small cell lung cancer. Clin Pharmacol Ther. 2006;80:136–45.
Hurst S, Ryan A, Ng C. Comparative nonclinical assessments of the proposed biosimilar PF-05280014 and Trastuzumab (Herceptin). BioDrugs. 2014;28:451–9.
Quartino A, Hillenbach C, Li J, et al. Population pharmacokinetic and exposure-response analysis for trastuzumab administered using a subcutaneous ‘manual syringe’ injection or intravenously in women with HER2-positive early breast cancer. Cancer Chemother Pharmacol. 2016;77:77–88.
Li J, Ren Y, Yuan Y, Ji SM, Zhou SP, Wang LJ, et al. Preclinical PK/PD model for combined administration of erlotinib and sunitinib in the treatment of A549 human NSCLC xenograft mice. Acta Pharmacol Sin. 2016;37:930–40.
Faivre S, Delbaldo C, Vera K, Robert C, Lozahic S, Lassau N, et al. Safety, pharmacokinetic, and antitumor activity of SU11258, a novel oral multitarget tyrosine kinase inhibitor, in patients with cancer. J Clin Oncol. 2006;24:25–35.
Van der Vijgh W. Clinical pharmacokinetics of carboplatin. Clin Pharm. 1991;21:242–61.
Bradshaw-Pierce E, Eckhardt S, Gustafson D. A physiologically based pharmacokinetic model of docetaxel disposition: from mouse to man. Clin Cancer Res. 2007;13:2768–76.
Luo R, Yang Z, Camuso A, et al. Dasatinib (BMS-354825) pharmacokinetics and pharmacodynamic biomarkers in animal models predict optimal clinical exposure. Clin Cancer Res. 2006;12:7180–6.
Graham R, Lum B, Cheeti S, et al. Pharmacokinetics of hedgehog pathway inhibitor vismodegib (GDC-0449) in patients with locally advanced or metastatic solid tumors: the role of alpha-1-acid glycoprotein binding. Clin Cancer Res. 2013;17:2512–20.
Wattanatorn W, McLeod H, Macklon F, et al. Comparison of 5-fluorouracil pharmacokinetics in whole blood, plasma, and red blood cells in patients with colorectal cancer. Pharmacotherapy. 1997;17:881–6.
Van der Lee M, Groothuis P, Ubink R, et al. The preclinical profile of the duocarmycin-based HER2-targeting ADC SYD985 predicts for clinical benefit in low HER2-expressing breast cancers. Mol Cancer Ther. 2015;14:692–703.
Gao H, Korn J, Ferretti S, et al. High-throughput screening using patient-derived tumor xenografts to predict clinical trial drug response. Nat Med. 2015;21:1318–25.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 93 kb)
Rights and permissions
About this article
Cite this article
Chandra, F., Zaks, L. & Zhu, A. Survival Prolongation Index as a Novel Metric to Assess Anti-Tumor Activity in Xenograft Models. AAPS J 21, 16 (2019). https://doi.org/10.1208/s12248-018-0284-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12248-018-0284-8