Abstract
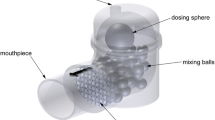
The routine of loading multiple capsules for delivery of high-dose antibiotics is time consuming, which may reduce patient adherence to inhaled treatment. To overcome this limitation, an investigation was carried out using four modified versions of the Aerolizer® that accommodate a size 0 capsule for delivery of high payload formulations. In some prototypes, four piercing pins of 0.6 mm each were replaced with a single centrally located 1.2-mm pin and one-third reduced air inlet of the original design. The performance of these inhalers was evaluated using spray-dried antibiotic powders with distinct morphologies: spherical particles with a highly corrugated surface (colistin and tobramycin) and needle-like particles (rifapentine). The inhalers were tested at capsule loadings of 50 mg (colistin), 30 mg (rifapentine) and 100 mg (tobramycin) using a multistage liquid impinger (MSLI) operating at 60 L/min. The device with a single pin and reduced air inlet showed a superior performance than the other prototypes in dispersing colistin and rifapentine powders, with a fine particle fraction (FPF wt% <5 μm in the aerosol) between 62 and 68%. Subsequently, an Aerolizer® with the same configuration (single pin and one-third air inlet) that accommodates a size 00 capsule was designed to increase the payload of colistin and rifapentine. The performance of the device at various inspiratory flow rates and air volumes achievable by most cystic fibrosis (CF) patients was examined at the maximum capsule loading of 100 mg. The device showed optimal performance at 45 L/min with an air volume of 1.5–2.0 L for colistin and 60 L/min with an air volume of 2.0 L for rifapentine. In conclusion, the modified size 00 Aerolizer® inhaler as a low-cost generic device demonstrated promising results for delivery of various high-dose formulations for treatment of lung infections.






Similar content being viewed by others
References
Agent P, Parrott H. Inhaled therapy in cystic fibrosis: agents, devices and regimens. Breathe. 2015;11(2):110–8.
González-Juarrero M, O’Sullivan MP. Optimization of inhaled therapies for tuberculosis: the role of macrophages and dendritic cells. Tuberculosis. 2011;91(1):86–92.
Karbasi-Afshar R, Aslani J, Ghanei M. Efficacy and safety of inhaler steroids in COPD patients: systematic review and meta-analysis of randomized placebo-controlled trials. Caspian J Intern Med. 2014;5(3):130–6.
Labiris NR, Dolovich MB. Pulmonary drug delivery. Part II: the role of inhalant delivery devices and drug formulations in therapeutic effectiveness of aerosolized medications. Br J Clin Pharmacol. 2003;56(6):600–12.
Geller DE. Comparing clinical features of the nebulizer, metered-dose inhaler, and dry powder inhaler. Respir Care. 2005;50(10):1313–22.
Zeidler M, Corren J. Hydrofluoroalkane formulations of inhaled corticosteroids for the treatment of asthma. Treat Respir Med. 2012;3(1):35–44. doi:10.2165/00151829-200403010-00005.
Islam N, Gladki E. Dry powder inhalers (DPIs)—a review of device reliability and innovation. Int J Pharm. 2008;360(1–2):1–11.
Agarkhedkar S, Kulkarni PS, Winston S, Sievers R, Dhere RM, Gunale B, et al. Safety and immunogenicity of dry powder measles vaccine administered by inhalation: a randomized controlled phase I clinical trial. Vaccine. 2014;32(50):6791–7.
Dharmadhikari AS, Kabadi M, Gerety B, Hickey AJ, Fourie PB, Nardell E. Phase I, single-dose, dose-escalating study of inhaled dry powder capreomycin: a new approach to therapy of drug-resistant tuberculosis. Antimicrob Agents Chemother. 2013;57(6):2613–9.
Novartis Pharmaceuticals UK Ltd. TOBI Podhaler 28 mg inhalation powder, hard capsules. 2015.
Elkins MR, Robinson P, Anderson SD, Perry CP, Daviskas E, Charlton B. Inspiratory flows and volumes in subjects with cystic fibrosis using a new dry powder inhaler device. Open Respir Med J. 2014;8:1–7.
Hodder R, Price D. Patient preferences for inhaler devices in chronic obstructive pulmonary disease: experience with Respimat(®) Soft Mist(™) Inhaler. Int J Chron Obstruct Pulmon Dis. 2009;4:381–90.
Moore AC, Stone S. Meeting the needs of patients with COPD: patients’ preference for the Diskus inhaler compared with the Handihaler. Int J Clin Pract. 2004;58(5):444–50.
Young PM, Crapper J, Philips G, Sharma K, Chan H-K, Traini D. Overcoming dose limitations using the Orbital® multi-breath dry powder inhaler. J Aerosol Med Pulm Drug Deliv. 2013;27(2):138–47.
Young PM, Salama RO, Zhu B, Phillips G, Crapper J, Chan H-K, et al. Multi-breath dry powder inhaler for delivery of cohesive powders in the treatment of bronchiectasis. Drug Dev Ind Pharm. 2014;41(5):859–65.
Zhou Q, Tong Z, Tang P, Citterio M, Yang R, Chan H-K. Effect of device design on the aerosolization of a carrier-based dry powder inhaler—a case study on Aerolizer(®) Foradile (®). AAPS J. 2013;15(2):511–22.
Coates M, Chan H-K, Fletcher D, Raper J. Influence of air flow on the performance of a dry powder inhaler using computational and experimental analyses. Pharm Res. 2005;22:1445–53.
Coates M, Fletcher D, Chan H-K, Raper J. The role of capsule on the performance of a dry powder inhaler using computational and experimental analyses. Pharm Res. 2005;22(6):923–32.
Chew NYK, Chan H-K, Bagster DF, Mukhraiya J. Characterization of pharmaceutical powder inhalers: estimation of energy input for powder dispersion and effect of capsule device configuration. J Aerosol Sci. 2002;33(7):999–1008.
Coates MS, Chan H-K, Fletcher DF, Raper JA. Effect of design on the performance of a dry powder inhaler using computational fluid dynamics. Part 2: air inlet size. J Pharm Sci. 2006;95(6):1382–92.
Wong WH, Crapper J, Chan H-K, Traini D, Young P. Pharmacopeial methodologies for determining aerodynamic mass distributions of ultra-high dose inhaler medicines. J Pharm Biomed Anal. 2010;51:853–7.
Gurjar M. Colistin for lung infection: an update. J Intensive Care. 2015;3(1):3. doi:10.1186/s40560-015-0072-9.
Chan JGY, Bai X, Traini D. An update on the use of rifapentine for tuberculosis therapy. Expert Opin Drug Deliv. 2014;11(3):421–31. doi:10.1517/17425247.2014.877886.
McKeage K. Tobramycin inhalation powder: a review of its use in the treatment of chronic Pseudomonas aeruginosa infection in patients with cystic fibrosis. Drugs. 2013;73(16):1815–27.
Selvam P, McNair D, Truman R, Smyth HDC. A novel dry powder inhaler: effect of device design on dispersion performance. Int J Pharm. 2010;401(1–2):1–6.
Zhou Q, Morton D, Yu H, Jacob J, Wang J, Li J, et al. Colistin powders with high aerosolisation efficiency for respiratory infection: preparation and in vitro evaluation. Immunol Rev. 2013;102(10):3736–47.
Chan JGY, Duke CC, Ong HX, Chan JCY, Tyne AS, Chan H-K, et al. A novel inhalable form of rifapentine. J Pharm Sci. 2014;103(5):1411–21.
ChemNet. 32986-56-4 tobramycin. 2016 [cited 30/06/2016].
Tiddens HA, Geller DE, Challoner P, Speirs RJ, Kesser KC, Overbeek SE, et al. Effect of dry powder inhaler resistance on the inspiratory flow rates and volumes of cystic fibrosis patients of six years and older. J Aerosol Med. 2006;19(4):456–65.
U.S. Pharmacopeial Convention. Tobamycin inhalation solution In: The tobramycin inhalation solution revision bulletin. The United States Pharmacopeial Convention; 2015.
Miller DP, Tan T, Tarara TE, Nakamura J, Malcolmson RJ, Weers JG. Physical characterization of tobramycin inhalation powder: I. rational design of a stable engineered-particle formulation for delivery to the lungs. Mol Pharm. 2015;12(8):2582–93. doi:10.1021/acs.molpharmaceut.5b00147.
Dash AK, Suryanayanan R. Solid-state properties of tobramycin. Pharm Res. 1991;8(9):1159–65.
Srichana T, Martin GP, Marriott C. Dry powder inhalers: the influence of device resistance and powder formulation on drug and lactose deposition in vitro. Eur J Pharm Sci. 1998;7(1):73–80.
Dal Negro RW. Dry powder inhalers and the right things to remember: a concept review. Multidiscip Respir Med. 2015;10(1):13.
Clark AR, Hollingworth AM. The relationship between powder inhaler resistance and peak inspiratory conditions in healthy volunteers—implications for in vitro testing. J Aerosol Sci. 1993;6(2):99–110.
Kruse M, Rosenkranz B, Dobson C, Ayre G, Horowitz A. Safety and tolerability of high-dose formoterol (Aerolizer) and salbutamol (pMDI) in patients with mild/moderate, persistent asthma. Pulm Pharmacol Ther. 2005;18(3):229–34.
Adams WP, Lee SL, Plourde R, Lionberger RA, Bertha CM, Doub WH, et al. Effects of device and formulation on in vitro performance of dry powder inhalers. AAPS J. 2012;14(3):400–9.
Hassan MS, Lau RWM. Effect of particle shape on dry particle inhalation: study of flowability, aerosolization, and deposition properties. AAPS PharmSciTech. 2009;10(4):1252–62.
Vehring R. Pharmaceutical particle engineering via spray drying. Pharm Res. 2008;25(5):999–1022.
Chan J, Tyne A, Pang A, Chan H-K, Young P, Britton W, et al. A rifapentine-containing inhaled triple antibiotic formulation for rapid treatment of tubercular infection. Pharm Res. 2013;31(5):1239–53. doi:10.1007/s11095-013-1245-7.
Vanbever R, Mintzes JD, Wang J, Nice J, Chen D, Batycky R, et al. Formulation and physical characterization of large porous particles for inhalation. Pharm Res. 1999;16(11):1735–42. doi:10.1023/a:1018910200420.
Tong ZB, Zheng B, Yang RY, Yu AB, Chan HK. CFD-DEM investigation of the dispersion mechanisms in commercial dry powder inhalers. Powder Technol. 2013;240:19–24. doi:10.1016/j.powtec.2012.07.012.
Kondo T, Tanigaki T, Hibino M, Ohe M, Kato S. Resistances of dry powder inhalers and training whistles and their clinical significance. Arerugi. 2014;63(10):1325–9.
Lavorini F. The challenge of delivering therapeutic aerosols to asthma patients. ISRN Allergy. 2013;2013:17.
Acknowledgments
Thaigarajan Parumasivam is a recipient of the Malaysian Government Scholarship. Sharon Leung is a research fellow supported by the University of Sydney. The authors wish to acknowledge the technical support of Australian Microscopy & Microanalysis Research Facility at the Australian Centre for Microscopy and Microanalysis, The University of Sydney. The work was supported by the Australian Research Council’s Discovery Project (DP150103953), the National Health and Medical Research Council Centre of Research Excellence in Tuberculosis Control (APP1043225) and Project grant (APP104434) and the NSW Government Infrastructure Grant to the Centenary Institute.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material Fig. 1
(DOCX 46 kb)
Supplementary material Fig. 2
(DOCX 21 kb)
Supplementary material Fig. 3
(DOCX 16 kb)
Supplementary material Table I
(DOCX 14 kb)
Supplementary material Table II
(DOCX 15 kb)
Supplementary material Table III
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Parumasivam, T., Leung, S.S.Y., Tang, P. et al. The Delivery of High-Dose Dry Powder Antibiotics by a Low-Cost Generic Inhaler. AAPS J 19, 191–202 (2017). https://doi.org/10.1208/s12248-016-9988-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12248-016-9988-9