Abstract
Drug delivery vehicles can influence the topical delivery and the efficacy of an active pharmaceutical ingredient (API). In this study, the influence of Pheroid™ technology, which is a unique colloidal drug delivery system, on the skin permeation and antimelanoma efficacy of 5-fluorouracil were investigated. Lotions containing Pheroid™ with different concentrations of 5-fluorouracil were formulated then used in Franz cell skin diffusion studies and tape stripping. The in vitro efficacy of 5-fluorouracil against human melanoma cells (A375) was investigated using a flow cytometric apoptosis assay. Statistically significant concentrations of 5-fluorouracil diffused into and through the skin with Pheroid™ formulations resulting in an enhanced in vitro skin permeation from the 4.0% 5-fluorouracil lotion (p < 0.05). The stratum corneum-epidermis and epidermis-dermis retained 5-fluorouracil concentrations of 2.31 and 6.69 μg/ml, respectively, after a diffusion study with the 4.0% Pheroid™ lotion. Subsequent to the apoptosis assay, significant differences were observed between the effect of 13.33 μg/ml 5-fluorouracil in Pheroid™ lotion and the effects of the controls. The results obtained suggest that the Pheroid™ drug delivery system possibly enhances the flux and delivery of 5-fluorouracil into the skin. Therefore, using Pheroid™ could possibly be advantageous with respect to topical delivery of 5-fluorouracil.
Similar content being viewed by others
INTRODUCTION
There are two categories of skin cancer which are melanoma and non-melanoma skin cancer (NMSC). Non-melanoma skin cancer is the most frequently diagnosed form of cancer, but it has the lower mortality rate while melanoma though infrequently diagnosed has a high mortality rate (1). Basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) are the NMSCs, and they originate from epidermal keratinocytes (2). Cutaneous malignant melanoma (CMM) originates from melanoma cells, which are also found in the epidermis (1). Actinic keratoses and Bowen’s disease though not true invasive carcinomas are usually included in discussions about skin cancer because of their relationship with skin cancers (3). Early detection of skin cancer is advocated for because neglected NMSCs may grow invasively and SCC may metastasize (1). Prompt detection will lead to early treatment and in turn improved prognoses (3). Currently, surgical treatment is the main recommendation for the treatment of skin cancer; however, cases do exist where surgery is not feasible and an alternative method must be used. Seeing as NMSC and CMM occur within the skin, it falls within reason that effective topical medicaments with low adverse effect profiles can be viable alternatives.
Cancer is characterized by evasion of apoptosis or defective apoptosis mechanisms which in turn allow uncontrollable development of cells (4). Chemotherapy of cancer is thus aimed at restoring the apoptosis balance or eliminating the rapidly dividing cells (5). 5-Fluorouracil is a pyrimidine antimetabolite which acts by inhibiting thymidylate synthase (TS). Thymidylate synthase is essential for the replication and repair of deoxyribonucleic acid (DNA), and its inhibition causes the induction of apoptosis and cell death (6). The unrestrained division of cancer cells is linked to insufficient apoptosis, so an increase in apoptosis should reflect antitumor activity.
In order to target tumorigenic cells within the skin and minimize systemic and topical adverse effects, 5-fluorouracil must penetrate into the skin layers and exert its effects within the epidermis and dermis. The available routes for administration of 5-fluorouracil are the intravenous and topical routes (6); in this study, the focus was on the topical route of administration. Formulation of topical treatment modalities is challenging due to the relatively impermeable nature and barrier properties of the skin (7). The outermost layer of the skin (the stratum corneum) is lipophilic, so it hinders the permeation of hydrophilic drugs such as 5-fluorouracil through the skin. The physicochemical properties of an API play a huge role in determining whether or not it will diffuse into and through the skin. According to Naik et al. (8), in order to allow for skin permeation, an API must have an aqueous solubility of at least 1 mg/ml, a molecular weight below 500 Da, a melting point below 200°C, and a partition coefficient (log P) between 1 and 3 (8). The values referred to by Naik et al. are not absolute values but merely give an indication of the optimal range of values, for example, Chandrashekar and Rani (9) reference values of molecular weight below 400, log P (octanol-water) between −1.0 and 4. Due to the introduction of various methods for enhancing skin permeation, new frontiers are being reached daily and the abovementioned values are constantly shifting. The log D (at 22°C, pH 7.4—acetate buffer) value of 5-fluorouracil (−0.98) as according to Buur et al. (10) does not lie within the required range and neither does the melting point of 282°C (11). It is not known which physicochemical properties have a greater influence on skin diffusion, so it is not possible to fully predict skin diffusion by the use of a few physicochemical properties. However, in light of the literature on hand, it was tentatively predicted that 5-fluorouracil would not easily penetrate the skin barrier. Due to the unfavorable skin permeation profile of 5-fluorouracil in conventional formulations, there has been an increased interest in the use of drug delivery systems to deliver 5-fluorouracil into the deeper layers of the skin. Research has been carried out on the topical delivery of 5-fluorouracil using drug delivery systems such as ethosomes (12) niosomes, liposomes, transfersomes (13), and nanogels (14). In these studies, it showed that the drug delivery systems resulted in an increase in either the flux or retention of API in the skin layers. Therefore, drug delivery systems are viable alternatives for the topical delivery of 5-fluorouracil.
In this study, a novel and patented form of technology that is used in the delivery of pharmaceutical actives, the Pheroid™ drug delivery system, was used to aid the delivery of 5-fluorouracil into the skin. Pheroid™ is composed of stable lipid-based submicron and micron-sized structures that form a unique colloidal system in a dispersion medium (15). The entrapment of APIs in Pheroid™ improves the control of size, charge, and the hydrophilic-lipophilic characteristics of APIs by a large margin thus altering their ability to permeate through membranes. The drug delivery system was employed to carry the API into the skin thus aiding the skin permeation of the API and simultaneously protecting the skin from direct contact with the API. The Franz cell diffusion experiments aimed to determine the topical and transdermal delivery of 5-fluorouracil and investigate the influence of Pheroid™ technology and the influence of a change in API concentration on the delivery of the drug into and through the skin. Skin diffusion studies were conducted with Pheroid™ and non-Pheroid™ formulations at four different concentrations of 5-fluorouracil.
An API must undoubtedly be able to exert its clinical action after incorporation into a formulation, so we decided to conduct drug efficacy tests to ensure that 5-fluorouracil still possessed its anticancer activity after formulation. Drug efficacy tests were conducted utilizing the different active pharmaceutical ingredient (API) concentrations in solution, non-Pheroid™, and Pheroid™ lotions in order to also determine variations due to the differing drug delivery systems. The aim was to observe the in vitro efficacy of 5-fluorouracil on human melanoma cells and investigate the influence of drug delivery vehicles on the API efficacy. Cells were subjected to various concentrations of 5-fluorouracil in three different vehicles (lotion, Pheroid™ lotion, and 0.0067 M phosphate-buffered saline (PBS)) and analyzed for occurrence of apoptosis using flow cytometry. Tsuji and Karasek (16) investigated the effect of 5-fluorouracil on human melanocytes and malignant melanoma cells, where they discovered that concentrations of 1.92 × 10−5–3.84 × 10−4 M (2.50–49.95 μg/ml) resulted in cell death after 5 weeks. This concentration range was used as a guideline. To determine the concentrations of 5-fluorouracil that result in the required response within 24 h in vitro, three concentrations within the lower end of the range by Tsuji and Karasek (16) and one concentration below the minimum concentration were used. Concentrations of 1.67, 3.33, 6.67, and 13.3 μg/ml 5-fluorouracil were deemed as appropriate. Therefore, the effects of concentration and Pheroid™ technology on topical and transdermal drug delivery and on the in vitro efficacy of 5-fluorouracil were investigated.
MATERIALS AND METHODS
Materials
The API, 5-fluorouracil, was obtained from DB Fine Chemicals (Johannesburg, South Africa). Cetyl alcohol, liquid paraffin, span 60, tween 80, potassium dihydrogen orthophosphate (KH2PO4), and the sodium hydroxide (NaOH) were purchased form Merck (Darmstadt, Germany), 96% ethanol from Rochelle Chemicals (Johannesburg, South Africa), and dl-α-tocopherol from Chempure (Pretoria, South Africa). Deionized HPLC-grade water was used throughout the whole study.
The human melanoma cells (A375) for cell culture were obtained from American Type Culture Collection (Manassas, VA). The culture media for cell cultivation consisted of Dulbecco’s Modified Eagle Medium (DMEM), fetal bovine serum (FBS), and Pen-Strep, which were all obtained from Sigma-Aldrich (St Louis, MO). Other materials that were used for the cell cultivation and drug efficacy tests are PBS 0.0067 M (Thermo Scientific, West Palm Beach, FL), dimethylsulphoxide (DMSO), and 96% ethanol obtained from Merck (Darmstadt, Germany). The Single Channel Annexin V/Dead Cell Apoptosis Kit with Alexa Fluor® 488 annexin V and SYTOX® Green for Flow Cytometry and trypsin-EDTA 25% were purchased from Life Technologies (Grand Island, NY).
Formulation of Semi-Solid Dosage Forms
Lotions were formulated with and without Pheroid™, containing 5-fluorouracil concentrations of 0.5, 1.0, 2.0, and 4.0% (w/w). Eight formulations were thus used in the in vitro drug efficacy tests and skin diffusion studies. The composition of the formulations is seen in Table I. The oil phase and aqueous phase with exclusion of ethanol were separately heated to 80°C. The oil phase was then added to the aqueous phase, and the mixture homogenized at 12,500 rpm until a temperature of 40°C was reached. Ethanol was added, and homogenization continued until room temperature was reached. With respect to the Pheroid™ lotions, distilled water was saturated with nitrous oxide gas then used in the place of normal distilled water during formulation. This method produced smooth lotions with a homogenous white appearance.
Physicochemical Characterization of Formulations
The pH of the formulations was measured immediately after formulation using a Mettler Toledo pH meter (Greifensee, Switzerland). Average droplet size of the formulations was determined using the Malvern Mastersizer 2000, with a wet cell Hydro 2000 MU dispersion unit (Malvern Instruments, Worcestershire, UK). Freshly prepared Pheroid™ and non-Pheroid™ formulations were diluted with distilled water, and measurements were taken when an obscuration of approximately 15% was achieved. The zeta potential of the formulations was determined using a Zetasizer Nano ZS (Malvern Instruments, Worcestershire, UK). Freshly prepared samples were diluted to 1.0% with distilled water (1 g of formulation in 100 ml of distilled water). A volume of approximately 1.5 ml of the formulation suspension was added to a disposable cuvette, and the zeta potential was measured.
The viscosity of the formulations was determined using a small sample adapter on a Brookfield DV-II+ Viscometer+ (Middleboro, MA, USA). The viscosity was measured at room temperature every 10 s for up to 30 measurements. The average of the 30 readings taken for each emulsion was calculated. The percentage torque for all measurements was between 21 and 37%.
Cell Cultivation
A cell culture model was utilized in this study to determine the efficacy of 5-fluorouracil in inducing apoptosis in human melanoma cells (A375) in vitro. The A375 cells were cultivated in 75 cm2 flasks; the culture media consisted of 10% FBS and 1% Pen-Strep in DMEM. The cells were fed with fresh media every day and split when ∼80% confluency was reached (17).
Cell viability was determined with a Countess automated cell counter (hemocytometer). A uniform cell suspension (10 μl) was mixed with 10 μl of 0.4% trypan blue (18). The cells were left for ∼3 min for the cells to stain and loaded onto a chamber of a Countess slide for examination. The total number of cells, viable cells, and dead cells and the percentage viability were then determined.
Optimization of Lotion Concentration
The lotion and Pheroid™ lotion both had oil components among other things which could have been potentially harmful to the cells and in turn resulted in cell death (the terms lotion and non-Pheroid™ lotion have been used interchangeably in the text). It was decided to dilute the placebo lotion and the placebo Pheroid™ lotion (0.1,1.0, 12.5, 25.0, 50.0, and 100.0%) with PBS, and note the effects of the different placebo dilutions on cell viability. An appropriately selected dilution of the lotions together with API was utilized in the assays to rule out cell death due to the effects of the lotion components and not the API.
On the first day, 2 ml each of a 1 × 105 cells/ml cell suspension was seeded into 48 wells of 6-well multiwell culture plates. After a 24-h incubation period (37°C and 5.0% CO2), 1 ml of a test solution or control (PBS, culture media, ethanol, or 0.5% 5-fluorouracil solution) was added to three wells each. On the third day, the cells were detached, the trypan blue test was performed, and cell viability was determined using a hemocytometer.
Drug Efficacy Analytical Assay
A cell suspension (500 μl) containing 1 × 105 cells/ml was seeded into 48 wells of 24-well multiwell culture plates. The cells were incubated for 24 h at a temperature of 37°C and in an atmosphere of 5.0% CO2. The 0.5, 1.0, 2.0, and 4.0% 5-fluorouracil formulated lotions were diluted by 1000 (dilution factor was determined by the optimization) to give final concentrations of 5.0, 10.0, 20.0, and 40.0 μg/ml 5-fluorouracil, respectively. Each lotion dilution (250 μl) was added to three wells each, and the cells were incubated for another 24 h. The final API concentrations in the wells became 1.67, 3.33, 6.67, and 13.30 μg/ml 5-fluorouracil due to the dilution rendered by the 500 μl of cell suspension already present. The Single Channel Annexin V/Dead Cell Apoptosis assay with Alexa Fluor® 488 annexin V and SYTOX® Green for Flow Cytometry (Invitrogen, USA) was performed according to the instructions provided for the kit. The A375 cells were analyzed by a fluorescence-activated cell sorter (FACSCalibur, Becton Dickinson, San Jose, CA). Cells were analyzed at a flow rate of 1000 events per second. A 488-nm argon laser was used for excitation. Forward and side scatter were collected on a log scale, and 100,000 events were collected for each sample. Cells labeled with annexin V and SYTOX® green were detected by FL1 photomultiplier tube (PMT) using log amplification. For every assay unstained cells, both treated and untreated were used as controls. Data was acquired using CELLQuest PRO (Becton Dickinson, San Jose, CA) and analyzed by FCS Express (version 4, De Novo Software, Los Angeles, CA). During analysis, a gate was set on the dot plot forward and side scatter to include cells and to exclude debris. Mean fluorescence intensities (MFI) were calculated from the respective histograms for annexin V and SYTOX® green.
High-Performance Liquid Chromatography Analytical Method
An Agilent® 1100 series (Agilent Technologies, Palo Alto, CA) which consists of a quaternary pump, a degasser, an auto-sampler injection mechanism, and a diode array detector was used with a Phenomenex® Synergi Fusion Reversed-Phase column (4.6 × 250.0 mm), with a 4-μm particle size (Phenomenex®, Torrance, CA). The mobile phase (4% acetonitrile) consisted of 40 ml acetonitrile, 1 ml orthophosphoric acid, and HPLC-grade water to make it 1000 ml. The analysis was done at a wavelength of 266 nm with a flow rate of 1 ml/min and an injection volume of 50 μl. The API eluted at approximately 4.6 min, so the stop time was set to 6.0 min. Data acquisition and analysis of 5-fluorouracil peak areas in samples were done with ChemStation Rev. A.10.02 software (Santa Clara, CA). The calibration curve had a regression coefficient of 0.999 showing that the method was stable, reliable, and accurate. The limit of detection and lower limit of quantification (LLOQ) for this method were observed to be 0.005 and 0.012 μg/ml, respectively. If a concentration below the LLOQ was detected during any of the analyses, the results were deemed as unreliable and therefore rejected.
Aqueous Solubility Determination
An excess of 5-fluorouracil was added to 5 ml of phosphate buffer solution (0.06 M NaOH and 0.08 M KH2PO4, pH 7.4) in order to make a super-saturated solution. The super-saturated solution was constantly stirred by a magnetic stirrer and maintained at 32°C (temperature at the surface of the skin) using a JB Grant® constant temperature water bath (19,20). After 24 h, the supersaturated sample was filtered, diluted, and analyzed in duplicate by HPLC. The experiment was conducted in triplicate.
Octanol-Buffer Distribution Coefficient (log D) Determination
Pre-saturated n-octanol and buffer were prepared by mixing equal volumes of phosphate buffer solution (pH 7.4) and n-octanol. The mixture was stirred vigorously and left to equilibrate for 24 h. The two layers were separated, and 5 mg of 5-fluorouracil was dissolved in a tube with 5 ml of pre-saturated n-octanol. Pre-saturated buffer (5 ml) was then added to the 5-fluorouracil in n-octanol. The tube was placed in a temperature-controlled (32°C) auto-rotator for 24 h. The solution was centrifuged for 15 min at 5000 rpm with an Eppendorf Centrifuge 5804 R. The whole experiment was done in triplicate. Aqueous phases were then extracted from each tube and analyzed in duplicate using HPLC. The log D value was calculated as the logarithmic ratio of the concentration of 5-fluorouracil in the n-octanol phase relative to the concentration in the buffer phase.
Preparation of Skin for the Skin Diffusion Experiments
The in vitro skin diffusion studies made use of female abdominal human skin obtained from Caucasian cosmetic abdominoplasty surgery patients. Ethical approval for the obtaining, preparing, and using of human skin in the research was obtained from the Research Ethics Committee of the North-West University (Ethical approval number—NWU-00114-11-A5). Permission was obtained from the surgeons and informed consent from the participating anonymous patients, allowing the use of the excised skin in the research. The excised skin was prepared and then frozen within 24 h of the surgery. The skin samples were prepared using an electric Zimmer® dermatome (Zimmer, Ohio, USA) at a thickness of 400 μm. This thickness included the epidermis and part of the dermis. The dermatomed skin was placed on top of a Whatman® filter paper, and circles with a diameter of approximately 15 mm were punched into the skin. It was ensured that each circle of the skin on the filter paper was big enough to cover the diffusion area. The skin circles were wrapped in foil, placed in a Ziploc® bag and then frozen at −20°C until needed.
Franz Cell Diffusion Studies
Vertical Franz cells were used for the diffusion studies. The Franz cells had a receptor volume capacity of approximately 2 ml and a diffusion area of 1.075 cm2. Twelve Franz cells were used for each experiment, ten with the test formulation and two control cells. The buffer (pH 7.4) was pre-warmed to 37°C (physiological temperature) in a water bath an hour before the experiment commenced. The donor phase formulation was placed in a 32°C (temperature at the skin surface) water bath for at least an hour. The donor and receptor compartments of a Franz cell were greased with Dow Corning® vacuum grease, and a magnetic stirring rod was placed into the receptor compartment. A circle of skin (stratum corneum facing up towards the donor compartment) or a polytetrafluoroethylene (PTFE) membrane was placed onto the lower half (receptor) of the Franz cell. The PTFE membrane filters were used in the drug release studies as the aim was to merely determine whether 5-fluorouracil was released from the formulations. Skin samples were used in the skin diffusion studies as the aim was now to determine the diffusion of 5-fluorouracil into and through the skin. The two compartments of the Franz cell were placed together, sealed with vacuum grease to prevent leakage, and secured together with a horseshoe clamp. Phosphate buffer solution (2 ml), pH 7.4, was added to the receptor compartment, and 1 ml of the semi-solid formulation under investigation was placed into the donor phase. An infinite dose was used in order to ensure that there was a drug reservoir in the donor phase over the 12 h period, and the drug concentration in the donor phase would not be the rate-limiting step in the diffusion process. The donor compartment was covered to avoid the loss of constituents by evaporation. The assembled Franz cells were placed on a Franz cell stand and placed in a water bath with a Variomag® magnetic stirrer (mixed receptor phase contents to maintain homogeneity) ensuring that only the receptor compartment of the Franz cell was immersed. This was recorded as time 0.0 h. The entire receptor buffer phase was removed at predetermined time intervals and replaced with fresh buffer to maintain sink conditions. The extracted samples were immediately analyzed by HPLC.
In vitro drug release studies were conducted with 0.45 μm PTFE membrane filters to determine if 5-fluorouracil was released from the formulations. The receptor phase was extracted every hour for 6 h, giving extraction times of 1, 2, 3, 4 5, and 6 h.
Thereafter, 12 h skin diffusion studies were done and the amount of 5-fluorouracil that diffused through the skin in vitro was determined. It was observed during a pilot study that very low amounts of 5-fluorouracil permeated through the skin for the greater duration of the experiments, leading to problems with accurate detection and quantification. So for the skin diffusion experiments it was decided to do a single extraction after 12 h, thus analyzing only the total amount of 5-fluorouracil that diffused through the skin. Tape stripping was performed on the skin after the 12 h diffusion.
Tape Stripping Procedure
The tape stripping technique is useful in dermatopharmacological research for selectively removing the skin’s outermost layer, the stratum corneum (21). This study focused on topical drug delivery, so tape stripping was performed in order to determine the amount of drug that was retained in the layers of the skin. After completion of the diffusion study, the tape stripping technique as described by Pellet et al. (22) was followed, but phosphate buffer solution, pH 7.4, was used as the solvent and the samples in buffer were stored overnight at 4°C. The diffusion cells were cautiously separated, and the skin was pinned onto Whatman® filter paper and stapled to a hard board. The skin was cleaned by gently wiping it with tissue paper in order to remove excess drug. Thereafter, one strip of 3M Scotch® Magic™ tape was applied with uniform pressure over the clearly marked diffusion area and discarded as it represented unabsorbed drug on the skin surface. Contrary to the above described procedure, some researchers prefer to wash the skin surface with water and with ethanol in order to efficiently remove the remaining formulation and therefore use all the tape strips for analysis (23). In this study, it was decided to wipe off the excess semi-solid formulation and use the first tape strip to represent the unabsorbed drug in order to ensure that any remaining formulation is removed as these were semi-solid formulations and not liquid formulations. This helped to maintain uniformity in treatment of samples as the stratum corneum becomes very tender and easily tears after a diffusion study possibly altering results.
This procedure was repeated with 15 more tape strips for each Franz cell, but these strips were placed in a clearly labeled vial containing 5 ml buffer and kept overnight at 4°C. An indication of the complete removal of the stratum corneum was when the viable epidermal layer glistened. The remaining skin was cut into pieces to enlarge surface area and placed into appropriately labeled vials. A volume of buffer (5 ml) was added, and the samples were kept overnight at 4°C. On the following day, the tape strip samples (represented the stratum corneum-epidermis) and skin samples (represented the epidermis-dermis) in buffer were filtered then analyzed by HPLC. Seeing as the abdominal skin samples used were 400 μm thick, it was presumed that the skin samples left after the tape stripping would constitute part of both the epidermal and dermal skin layers.
Statistical Analysis
The Shapiro-Wilk test and quantile-quantile (q-q) plots were used to determine the normality of the data with the Statistica software package from StatSoft (Tulsa, OK). It was decided that the data had a sufficiently normal distribution for the performance of one-way analysis of variance (ANOVA). To uncover the individual differences, the Games-Howell for unequal variances and Tukey’s B post hoc tests were conducted.
RESULTS
Physicochemical Characterization of Formulations
The average values that were obtained for the different physicochemical parameters are shown in Table II.
Optimization of Lotion Concentration
The 0.1% dilution of the formulations gave the best results as tabulated in Table III.
Drug Efficacy Testing
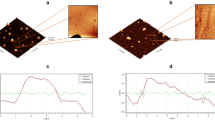
The geometric mean fluorescence intensity (MFI) was utilized for the data analysis. The MFI for each treatment was averaged and expressed as a percentage of the positive control (ethanol) MFI. Line graphs of 5-fluororacil concentration versus percentage MFI (%MFI) were drawn for each of the drug delivery vehicles (lotion, Pheroid™ lotion, and API solution), and they are shown in Fig. 1. Early signs of apoptosis were evident after the 24 h incubation period with the treatments.
Aqueous Solubility
The aqueous solubility of 5-fluorouracil in PBS was determined to be 17.6 mg/ml which is acceptable although slightly higher than the value of 12.5 mg/ml obtained in literature (24). The higher solubility value may have been due to the fact in this case, the aqueous solubility was determined in PBS at a slightly higher pH than that of water. The ions present and pH difference in PBS may have aided the dissolution of 5-fluorouracil due to salt formation. An aqueous solubility above 1 mg/ml is ideal for optimum skin permeability (8); therefore, the aqueous solubility of 5-fluorouracil was relatively ideal for skin permeation.
Octanol-Buffer Distribution Coefficient (log D)
A log D value of −1.15 was obtained for 5-fluorouracil in this study, which is close to the log P value of −0.83 as reported by Buur et al. (10). A log P value between 1 and 3 is required for optimum skin permeability (8), so from these results, it was tentatively predicted that 5-fluorouracil would not easily permeate through the skin.
The Release of 5-Fluorouracil from Formulations
The percentage of 5-fluorouracil that was released from the formulations did not remain constant with a change in formulation and/or initial concentration as seen in Table IV. When comparisons were made between a lotion and a Pheroid™ lotion of the same concentration level, it was revealed that the presence of Pheroid™ resulted in an increased average percentage of API release.
Skin Diffusion Studies
The Pheroid™ lotions resulted in higher 5-fluorouracil amounts diffused than their lotion counterparts at the same concentration. From an overall perspective, all the Pheroid™ lotions had higher total amounts diffused than all the lotions. Figure 2 shows the average amounts of 5-fluorouracil that diffused through the skin after 12 h from the different formulations.
Comparisons of the average amount of 5-fluorouracil (in μg/cm2) that diffused through human skin after 12 h from each lotion with the amounts diffused from the respective Pheroid™ lotion of the same concentration (n = 10) (*statistically significant difference between Pheroid™ and non-Pheroid™ formulations p < 0.05)
The 4.0% Pheroid™ lotion had the highest total amount diffused (57.6 μg/cm2), and the 0.5% Pheroid™ lotion had the second highest total amount diffused (31.6 μg/cm2). These results revealed that a low concentration of 5-fluorouracil in the formulations (as shown by the 0.5% Pheroid™ lotion) can result in a relatively high concentration of 5-fluorouracil diffusing through the skin. A statistically significant difference (p < 0.05) in the total amount diffused per unit area existed between the lotions and their Pheroid™ lotion counterparts at three of the four concentrations (0.5, 2.0, and 4.0%). The comparison between 1.0% lotion and 1.0% Pheroid™ lotion was not statistically significant (Fig. 2).
The total amount diffused per unit area from each lotion was compared with the total amount diffused per unit area from the Pheroid™ lotion of the same concentration. This was done in order to observe the effect of Pheroid™ on the transdermal delivery of 5-fluorouracil. Figure 2 shows the total amount diffused per unit area from the lotions and Pheroid™ lotions, with the same concentrations adjacent to each other.
Tape Stripping Study
The results from the tape stripping experiment are shown in Table V. The Pheroid™ lotions all resulted in a higher average concentration of 5-fluorouracil in the stratum corneum-epidermis and epidermis-dermis than their corresponding lotions of the same concentration. The only exception was the epidermis-dermis comparison at the 1.0% concentration.
DISCUSSION
Physicochemical Characterization of Formulations
The average values obtained from the physicochemical characterization of the freshly prepared lotions were within close range of each other for all the formulations. The droplet sizes in the formulations fell within the nanorange with the Pheroid™ lotions having a 50% smaller average size in comparison to the normal lotions. An inverse relationship exists between the size of the diffusing particle and flux; therefore, the difference in size may have had an influence in the differences in the various results obtained for skin diffusion (25). For a dispersion to be considered stable, the zeta potential values must be more positive than +30 mV or less negative than −30 mV; therefore, dispersions with a zeta potential between +30 and −30 mV are considered to be unstable due to a high possibility of aggregation occurring. In this study, the average zeta potential values obtained for the 5-fluorouracil lotions and 5-fluorouracil Pheroid™ lotions were −26.8 and −29.8, respectively. This reflects that the formulations were slightly unstable. The average pH values were acidic and within a range acceptable for topical application. This was a favorable pH as 5-fluorouracil is a weakly acidic drug with an acid dissociation constant (pKa) of 8.0 (26). As calculated according to the Henderson-Hasselbalch equation, 98% of the drug in the 5-fluorouracil lotions was unionized and 96% of the drug in the 5-fluorouracil Pheroid™ lotions was unionized at the pH of the formulations. This led to the assumption that the drug would be able to penetrate the skin membrane as drugs are more easily absorbed when in the unionized form. All the formulations had relatively small droplet sizes, with the Pheroid lotions having smaller droplet sizes than the normal 5-fluorouracil lotions.
Optimization of Lotion Concentration
The concentrated dilutions did not mix well with the cell suspensions and gave either erratic results or percentage viability values within the range of the ethanol positive control. The 0.1% dilutions of the placebo lotion and placebo Pheroid™ lotion treatments resulted in 94.3 and 95.0% cell viability, respectively. This was acceptable because they were in close range of the cell viability due to treatment with the positive controls (PBS and complete culture media) which meant that they were essentially harmless. Therefore, the 0.1% dilutions together with different API concentrations were utilized in the apoptosis assay.
Drug Efficacy Testing
All the Pheroid™ lotion treatments except the 3.33 μg/ml treatment resulted in higher %MFI values than the corresponding lotion and solution treatments. The 13.30 μg/ml resulted in a statistically significant increase in apoptosis, compared to the control and the lotion. This may be due to the fact that Pheroid™ is composed of fatty acids, and therefore, an affinity exists between Pheroid™ and cell membranes, resulting in more effective and fast uptake of Pheroid™ by cells (15). The presence of tocopherol in the Pheroid™ formulations may have played a role as it has been shown that tocopherol as an antioxidant has radical scavenging properties, and free radicals are associated with cancer development (27). The solution treatments produced the lowest %MFI in the cells in comparison to the lotion and Pheroid™ lotion treatments at the same concentrations. The %MFI produced by the lotion-treated cells increased with increase in concentration in a relatively linear manner. The Pheroid™ lotion treatments resulted in a lower %MFI in the 3.33 μg/ml treatment than in the 1.67 μg/ml. From the 3.33 μg/ml treatment to the 13.30 μg/ml treatment of the Pheroid™ lotion, the %MFI increased with concentration. A trend similar to that of the Pheroid™ lotions was observed with the API solutions. The effects of Pheroid™ and of increasing the concentration became clearer at the higher concentrations than at the lower concentrations. A similar trend has been demonstrated with 5-fluorouracil bola-surfactant niosomes and selenium nanoparticles, whereby the drug in niosomes resulted in a stronger cytotoxic effect in comparison to the free drug (28,29).
The results obtained in this study confirmed that 5-fluorouracil does result in apoptotic cell death and is effective against human melanoma (A375) cells. In a previous study, 5-fluorouracil loaded chitin nanogels resulted in only a mild cytotoxic effect against A375 cells after a 3-[4,5-dimethylthiazol-2-yl]-2,5 diphenyl tetrazolium bromide assay (14). This further demonstrates the proposition that the apoptosis-inducing effect of 5-fluorouracil seems to differ according to the vehicle that the API has been incorporated into.
Vesicle encapsulated 5-fluorouracil has been seen to have a reduced in vivo toxicity when used in combination with other anticancer therapies (30). In vivo studies were not conducted in this study, but it is possible that encapsulation of 5-fluorouracil with Pheroid™ may result in reduced toxicity and in turn reduced side effect profile. This is supported by the fact that the Pheroid™ encapsulated 5-fluorouracil resulted in increased apoptotic cell death as compared to the non-encapsulated drug which may reflect a reduced minimum effective concentration.
The Release of 5-Fluorouracil from Formulations
The penetration-enhancing effect of Pheroid™ vesicles has been documented by Grobler et al. (15), and these results concur with the results expected with the use of Pheroid™. An enhanced release from formulations results in a higher amount of 5-fluorouracil available on the skin surface for skin penetration.
The average cumulative amount released per unit area from the lotions generally increased with an increase in concentration, and the same is true of the Pheroid™ lotions. The conclusions were that 5-fluorouracil was released from all the formulations and Pheroid™ resulted in an increased release of 5-fluorouracil from the formulations.
Skin Diffusion Studies
All the Pheroid™ lotions resulted in a higher total amount diffused than the lotions without Pheroid™. This illustrates the enhancing effect of Pheroid™ on skin penetration as noted in studies done by Kilian (31) and van Dyk (32). It is possible that due to the lipophilic nature of Pheroid™ vesicles, 5-fluorouracil was easily carried into the skin while encapsulated in Pheroid™. Pheroid™ contains essential fatty acids, and these fatty acids help increase the fluidity of the stratum corneum and therefore transiently reduce the barrier function of the skin. Fatty acids insert themselves between the hydrophobic tails of the stratum corneum lipid bilayer which disturbs the arrangement of the lipids and in turn increases membrane fluidity. This decreases the resistance of the stratum corneum to permeants (33). However, 5-fluorouracil is hydrophilic in nature which means that it is “water loving,” so after reaching the dermis of the skin, the API could easily diffuse into the aqueous receptor phase. Without the aid of enhancers, a hydrophilic drug such as 5-fluorouracil is less likely to diffuse into or remain in the skin because the skin is a lipophilic membrane. Therefore, a low percentage of 5-fluorouracil was likely to diffuse into the skin alone and in turn into the aqueous receptor phase. This may explain why the amounts diffused from the non-Pheroid™ lotions were lower than those from the corresponding Pheroid™ lotions. Furthermore, the difference in droplet size may have attributed to the differences seen in skin permeation as nanosized particles have been found to be efficient drug carriers through hair follicles thus enhancing drug delivery (34). Vermaas (35) performed skin diffusion studies with 0.5% 5-fluorouracil lotions (with and without Pheroid™) and found that the Pheroid™ lotion resulted in a slightly higher amount diffused (10.01 µg/cm2) than the non-Pheroid™ lotion (9.06 μg/cm2), which is consistent with the results found in this study). The lotions that were formulated by Vermaas (35) had a composition similar to the lotions that were utilized in this study with the exception of 15.0% ethanol which was used as a preservative in this study instead of the parabens. Ethanol is also known to act as cosolvent and permeation enhancer, and it very well may have had a role in the higher concentrations diffused that were observed in this study (36). The mechanism by which ethanol acts is by disordering the stratum corneum’s lipid structure and giving the skin a more fluid structure thus allowing for easier drug penetration (37). When taking into consideration the rest of the results found by Vermaas (35), we see that the penetration-enhancing effect of Pheroid™ may depend on the nature of the formulation into which Pheroid™ is incorporated.
Tape Stripping Study
The overall observed effect of Pheroid™ in the tape stripping study could have been due to the lipophilicity rendered to the formulations by the presence of Pheroid™ which resulted in the vesicle entrapped 5-fluorouracil being retained in the lipophilic epidermis. Another possibility is that a higher concentration of 5-fluorouracil was able to penetrate into the skin layers from the Pheroid™ lotion than from the lotion, so consequentially, a higher concentration of 5-fluorouracil was available to remain in the skin. The concentration of 5-fluorouracil in the lotions had an effect on the epidermal concentration of 5-fluorouracil; this is implied by the increase in epidermal concentrations with increase in API concentration in formulation. For the 5-fluorouracil concentrations in the epidermis-dermis, a statistically significant result was only obtained with the comparison of the 4.0% lotion with the 4.0% Pheroid™ lotion. Pheroid™ had a practically significant influence on the epidermis-dermis values resulting from the 0.5 and 4.0% lotions (Pheroid™ vs. non-Pheroid™).
An ideal topical anticancer formulation would result in release of the API from the formulation, penetration of the API into the skin, diffusion of the API within the skin, and its retainment within the skin layers. In this study, the formulation which showed such optimal characteristics was the 2.0% lotion because a relatively low amount of 5-fluorouracil diffused through the skin per unit area (9.71 μg/cm2), but relatively high concentrations of 5-fluorouracil, was detected in the stratum corneum-epidermis (2.63 μg/ml) and epidermis-dermis (2.27 μg/ml). The results obtained suggest that 5-fluorouracil (1.67 – 13.33 μg/ml) can induce apoptosis in human melanoma (A375) cells in vitro, and this effect is possibly enhanced by Pheroid™. It could therefore follow that a 5-fluorouracil formulation resulting in apoptosis-inducing concentrations of 5-fluorouracil in the stratum corneum-epidermis and epidermis-dermis will result in death of melanoma cells within the skin layers.
The lotions prepared and used in this study all had 5-fluorouracil concentrations that are below the 5.0% 5-fluorouracil market product concentration. According to Vermaas (35), the total API diffused after 12 h from the commercial product was 2.52 μg/cm2, the concentration in the stratum corneum-epidermis was 0.12 μg/ml, and the concentration in the epidermis-dermis was 0.05 μg/ml. The results that were obtained from the commercial product are lower than all the results that were obtained in this study at the different concentrations. It can be tentatively predicted that therapeutic use of any one of the formulations from this study will result in a clinical effect similar to or better than the clinical effect of the commercial product. Huang et al. (38) reported that a 0.2% submicron emulsion of 5-fluorouracil was able to deliver 5-fluorouracil to the skin layers at concentrations similar to the 5.0% market production. This further shows that it is possible to deliver 5-fluorouracil to the skin at lower formulation concentrations in order to achieve a therapeutic effect that is comparable to the 5.0% market product with probably fewer side effects.
In the study by Sabitha et al. (14), the retention of 5-fluorouracil within the skin was greatly enhanced using 5-fluorouracil loaded chitin nanogels; however, the chitin nanogel formulations resulted in relatively mild cytotoxic activity against A375 cells. This highlights the need for an API which is both therapeutically effective against melanoma and is efficiently delivered to the epidermis and dermis.
CONCLUSION
The proposed influence of Pheroid™ on 5-fluorouracil efficacy will prove to be advantageous as a lower concentration of 5-fluorouracil will be required to exert a therapeutic effect. The use of lower concentrations should result in an improved side effect profile after application of 5-fluorouracil to the skin. In this case, Pheroid™ would be advantageous as it would decrease the concentration of API required for efficacy while increasing the amount of drug reaching the target site. Further research shall need to be done with a wider variation of 5-fluorouracil concentrations to confirm and fully characterize the effect of Pheroid™ on in vitro apoptosis induction by 5-fluorouracil.
REFERENCES
De Gruijl FR. Skin cancer and solar UV radiation. Eur J Cancer. 1999;35:2003–9.
Marks VJ, Hanson NW. Non-melanoma skin cancer. In: Hall BJ, Hall JC, editors. Sauer’s manual of diseases. 10th ed. Philadelphia: Wolters Kluwer Health; 2010. p. 305–12.
Marks R. An overview of skin cancers: incidence and causation. Cancer. 1995;75:607–12.
Erb P, Ji J, Wernli M, Kump E, Glaser A, Büchner SA. Role of apoptosis in basal cell and squamous cell carcinoma formation. Immunol Lett. 2005;100:68–72.
Lippens S, Hoste E, Vandenabeele P, Declercq W. Cell death in skin. In: Reed JC, Green DR, editors. Apoptosis: physiology and pathology. Cambridge: Cambridge University Press; 2011. p. 323–32.
Chu E, Sartorelli AC. Cancer chemotherapy. In: Katzung BG, Masters SB, Trevor AJ, editors. Basic and clinical pharmacology. 11th ed. New York: McGraw-Hill; 2009. p. 935–61.
Patzelt A, Antoniou C, Sterry W, Lademann J. Skin penetration from the inside to the outside: a review. Drug Discov Today Dis Mech. 2008;5:e229–35.
Naik A, Kalia YN, Guy RH. Transdermal drug delivery: overcoming the skin’s barrier function. Pharm Sci Technol Today. 2000;3:318–26.
Chandrashekar NS, Shobha Rani RH. Physicochemical and pharmacokinetic parameters in drug selection and loading for transdermal drug delivery. Indian J Pharm Sci. 2008;70:94–6.
Buur A, Bundgaard H, Falch E. Prodrugs of 5-fluorouracil. IV. Hydrolysis kinetics, bioactivation and physicochemical properties of various N-acyloxymethyl derivatives of 5-fluorouracil. Int J Pharm. 1985;24:43–60.
Rudy BC, Senkowski BZ. Fluorouracil. In: Florey K, editor. Analytical profiles of drug substances. New York: Academic; 1973. p. 221–44.
Puri R, Jain S. Ethogel topical formulation for increasing the local bioavailability of 5-fluorouracil: a mechanistic study. Anti-Cancer Drugs. 2012;23:923–34.
Alvi IA, Madan J, Kaushik D, Sardana S, Pandey RS, Ali A. Comparative study of transfersomes, liposomes, and niosomes for topical delivery of 5-fluorouracil to skin cancer cells: preparation, characterization, in vitro release, and cytotoxicity analysis. Anti-Cancer Drugs. 2011;22:774–82.
Sabitha M, Rejinold NS, Nair A, Lakshmanan V, Nair SV, Jayakumar R. Development and evaluation of 5-fluorouracil loaded chitin nanogels for treatment of skin cancer. Carbohydr Polym. 2012;91:48–57.
Grobler A, Kotze A, du Plessis J. The design of a skin-friendly carrier for cosmetic compounds using Pheroid™ technology. In: Wiechers J, editor. Science and applications of skin delivery systems. Wheaton: Allured Publishing; 2008. p. 283–311.
Tsuji T, Karasek MA. Differential effects of 5-fluorouracil on human skin melanocytes and malignant melanoma cells in vitro. Acta Derm Venereol. 1986;66:474–8.
ATCC: Product information. http://www.atcc.org/Products/All/CRL-1619.aspx#culturemethod (2012). Accessed 12 Dec 2014.
Phelan MC. Basic techniques for mammalian cell tissue culture. In: Bonifacino JS, Dasso M, Harford JB, Lippincott-Schwartz J, Yamada KM, editors. Current protocols in cell biology. New York: Wiley; 1998. p. 1–10.
Williams AC. Transdermal and topical drug delivery. London: Pharmaceutical Press; 2003.
Manconi M, Caddeo C, Sinico C, Valenti D, Mostallino MC, Lampis S, et al. Penetration enhancer-containing vesicles: composition dependence of structural features and skin penetration ability. Eur J Pharm Biopharm. 2012;82:352–9.
Surber C, Schwarb FP, Smith EW. Tape-stripping technique. In: Bronaugh RL, Maibach HI, editors. Percutaneous absorption: drugs-cosmetics-mechanisms-methodology. 3rd ed. New York: Marcel Dekker; 1999. p. 395–409.
Pellett MA, Roberts MS, Hadgraft J. Supersaturated solutions evaluated with an in vitro stratum corneum tape stripping technique. Int J Pharm. 1997;151:91–8.
Ge S, Lin Y, Lu H, Li Q, He J, Chen B, et al. Percutaneous delivery of econazole using microemulsion as vehicle: formulation, evaluation and vesicle-skin interaction. Int J Pharm. 2014;465:120–31.
Troy DB, editor. Remington: the science and practice of pharmacy. 21st ed. Philadelphia: Lippincott Williams and Wilkins; 2006.
Barry BW. Transdermal drug delivery. In: Aulton ME, editor. Pharmaceutics: the design and manufacture of medicines. 3rd ed. Edinburgh: Churchill Livingston; 2007. p. 565–97.
Kosjek T, Perko S, Zigon D, Heath E. Fluorouracil in the environment: analysis, occurrence, degradation and transformation. J Chromatogr A. 2013;1290:62–72.
Tavano L, Muzzalupo R, Picci N, de Cindio B. Co-encapsulation of lipophilic antioxidants into niosomal carriers: percutaneous permeation studies for cosmeceutical applications. Colloids Surf B: Biointerfaces. 2014;114:144–9.
Paolino D, Cosco D, Muzzalupo R, Trapasso E, Picci N, Fresta M. Innovative bola-surfactant niosomes as topical delivery systems of 5-fluorouracil for the treatment of skin cancer. Int J Pharm. 2008;353:233–42.
Liu W, Li X, Wong YS, Zheng W, Zhang Y, Cao W, et al. Selenium nanoparticles as a carrier of 5-fluorouracil to achieve anticancer synergism. ACS Nano. 2012;6:6578–91.
Zhou T, Xiao C, Fan J, Chen S, Shen J, Wu W, et al. A nanogel of on-site tunable pH-response for efficient anti-cancer drug delivery. Acta Biomater. 2013;9:4546–57.
Kilian D.: A comparative study between two lamellar gel phase systems and Emzaloids® as delivery vehicles for transdermal delivery of 5-fluorouracil and idoxuridine. http://dspace.nwu.ac.za/handle/10394/602 (2004).
Van Dyk C.: Transdermal delivery of 5-fluorouracil with Pheroid™ technology. http://dspace.nwu.ac.za/handle/10394/1905 (2008).
Uchechi O, Ogbonna JDN, Attama AA. Nanoparticles for dermal and transdermal drug delivery. In: Sezer AD, editor. Application of nanotechnology in drug delivery. Rijeka: InTech; 2014. p. 193–235.
Cheong-Weon C, Jun-Shik K, Seong-Jin K, Sang-Chul S. Enhanced transdermal delivery of loratadine from the EVA matrix. Drug Deliv. 2009;16:230–5.
Vermaas M.: Formulation of 5-fluorouracil for transdermal delivery. http://dspace.nwu.ac.za/handle/10394/6977 (2010).
Alexander A, Dwivedi S, Ajazuddin, Giri TK, Saraf S, Saraf S, et al. Approaches for breaking the barriers of drug permeation through transdermal drug delivery. J Control Release. 2012;164:26–40.
Benson HAE. Transdermal drug delivery: penetration enhancement techniques. Curr Drug Deliv. 2005;2:23–33.
Huang YB, Huang CT, Tsou HY, Fu LT, Fu YS, Tsai YH, et al. The transport effect of submicron emulsions on 5-fluorouracil topical application. J Microencapsul. 2013;30:425–31.
ACKNOWLEDGMENTS
The authors would like to express their sincere gratitude towards the National Research Foundation (NRF) of South Africa and the Centre of Excellence for Pharmaceutical Sciences (North-West University, Potchefstroom, South Africa) for the financial support. Any opinion, findings, and conclusions or recommendations expressed in this material are those of the authors, and therefore, the NRF does not accept any liability in regard thereto. Special thanks to Mrs Mari van Reenan for the statistical analysis of the experimental data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chinembiri, T.N., Gerber, M., du Plessis, L. et al. Topical Delivery of 5-Fluorouracil from Pheroid™ Formulations and the In Vitro Efficacy Against Human Melanoma. AAPS PharmSciTech 16, 1390–1399 (2015). https://doi.org/10.1208/s12249-015-0328-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12249-015-0328-7