Abstract
Researchers have adopted a variety of analytical techniques to examine the collective influence of 24-h movement behaviors (i.e., physical activity, sedentary behaviors, sleep) on mental health, but efforts to synthesize this growing body of literature have been limited to studies of children and youth. This systematic review investigated how combinations of 24-h movement behaviors relate to indicators of mental ill-being and well-being across the lifespan. A systematic search of MEDLINE, PsycINFO, Embase, and SPORTDiscus was conducted. Studies were included if they reported all three movement behaviors; an indicator of mental ill-being or well-being; and were published in English after January 2009. Samples of both clinical and non-clinical populations were included. A total of 73 studies (n = 58 cross-sectional; n = 15 longitudinal) met our inclusion criteria, of which 47 investigated children/youth and 26 investigated adults. Seven analytical approaches were used: guideline adherence (total and specific combinations), movement compositions, isotemporal substitution, profile/cluster analyses, the Goldilocks method and rest-activity rhythmicity. More associations were reported for indicators of mental ill-being (n = 127 for children/youth; n = 53 for adults) than well-being (n = 54 for children/youth; n = 26 for adults). Across the lifespan, favorable benefits were most consistently observed for indicators of mental well-being and ill-being when all three components of the 24-h movement guidelines were met. Movement compositions were more often associated with indicators of mental health for children and youth than adults. Beneficial associations were consistently observed for indicators of mental health when sedentary behavior was replaced with sleep or physical activity. Other analytic approaches indicated that engaging in healthier and more consistent patterns of movement behaviors (emphasizing adequate sleep, maximizing physical activity, minimizing sedentary behaviors) were associated with better mental health. Favorable associations were reported less often in longitudinal studies. Collectively, these findings provide further support for adopting an integrative whole day approach to promote mental well-being and prevent and manage mental ill-being over the status quo of focusing on these behaviors in isolation. This literature, however, is still emerging—for adults in particular—and more longitudinal work is required to make stronger inferences.
Similar content being viewed by others
Introduction
Poor mental health and high rates of mental illness are major concerns across the lifespan in society today. Findings from the 2019 Global Burden of Disease Study estimated that roughly one in eight adults have a mental disorder [1], whereas the prevalence is slightly lower among children and adolescents at one in twelve individuals [2]. Depression and anxiety represent the most common mental health problems, and rates of these disorders have risen further since the onset of the COVID-19 pandemic [3]. Beyond clinically diagnosed mental disorders, recent evidence has also found overall declines in mental health and well-being across the lifespan [4, 5]. Collectively, the impacts of poor mental health and mental illness are felt at many levels in our society—whether it be at the individual, family, school or workplace—and place a considerable burden on health care systems and the economy [6, 7]. The economic burden of mental disorders is only expected to rise, with projections estimating an economic burden of $6 trillion by 2030 [8]. Such evidence underscores the need to better understand the etiology of mental well-being and mental disorders.
Historically, mental health research has predominantly focused on psychopathology and distress, adopting a pathogenic perspective based on the medical model of disease. This model views mental health as merely the absence of mental illness, such as depression or anxiety. However, recent developments have brought forth the dual continua model of mental illness and health [9]. This model recognizes that mental illness and mental health are related but distinct dimensions. Keyes' [9] seminal research provided robust evidence for this model, suggesting that individuals range from languishing to flourishing on a mental health continuum, while also existing on a parallel continuum of mental illness, characterized by the presence or absence of psychopathological symptoms. The dual continua model thus offers a more holistic understanding of mental health, promoting a refined view that covers the entire spectrum from dysfunction to optimal mental well-being. It has been proposed that widespread and systematic adoption of the dual-continua model would inspire significant reform to the mental health care system, which may better prepare systems for the overwhelming burden of mental illness [10]. It is therefore imperative that we identify cost-effective strategies that can not only assist in the prevention and/or management of mental ill-being, but also promote mental well-being.
Mental health promotion efforts targeting modifiable lifestyle behaviors are receiving growing interest as a potential low-cost alternative to traditional psychotherapy and pharmacological interventions [11, 12]. Among these behaviors there has been considerable recent attention paid to how much we move, remain stationary, and sleep over the course of a 24-h period. While there is no consensus terminology for referring to these behaviors collectively [13], they are most commonly referred to as 24-h movement behaviors, the 24-h activity cycle, physical behaviors, time-use behaviors or time-use activity behaviors. We will use the term 24-h movement behaviors for the purpose of this review. Prior to the emergence of the notion that all movement behaviors we engage in over the course of a whole day are important for health [14], researchers generally examined physical activity, sedentary behaviors and sleep independently. Reviews of observational studies have generally shown that engaging in greater amounts of moderate-to-vigorous intensity physical activity [12, 15,16,17,18,19,20,21,22] and lower amounts of sedentary behavior, including recreational screen time [23,24,25,26,27,28,29], are associated with greater mental well-being and reduced risk of mental ill-being among children and youth as well as adults. It should be noted that context has been acknowledged to play an influential role in these relationships [20, 30], although existing literature has arguably placed a greater emphasis on duration, volume or intensity-based metrics. Studies investigating sleep duration, on the other hand, have suggested an optimal range may exist wherein too much or too little sleep is associated with poorer scores on indicators of mental health and greater risk of mental disorders [12, 31,32,33]. This siloed approach neglected the fact that movement behaviors are co-dependent (i.e., time spent engaging in one behavior reduces time available for other behaviors) and interact to influence health [34]. This was the impetus for development of 24-Hour Movement Guidelines, which were first released in Canada in 2016 with recommendations specific to children and youth [35]. Several countries have since adopted 24-Hour Movement Guidelines (e.g., [36,37,38]), and these recommendations have been tailored for other segments of the population (e.g., early childhood, adults, older adults) [39, 40]. Consequently, the release of these integrative guidelines has sparked an emergence of studies seeking to answer different research questions regarding how combinations of 24-h movement behaviors relate to a variety of health outcomes [41, 42].
To date, two systematic reviews and one scoping review have investigated associations between 24-h movement behaviors and indicators of mental health [43,44,45]. These reviews focused strictly on children and youth, which is likely attributable to the 24-Hour Movement Guidelines for Children and Youth being published first in 2016 [35]. Nevertheless, evidence from the systematic reviews generally suggested that adhering to an increasing number of the 24-h movement guidelines or all three guidelines (compared to none) were associated with favorable benefits for several indicators of mental health, risk of depression and depressive symptoms in particular [44, 45]. It is important to acknowledge, however, that the studies included in the systematic reviews were largely cross-sectional and analyses tended to focus on guideline adherence as opposed to other approaches such as compositional data analysis techniques, which are particularly appropriate for analyzing whole day time-use data given the approach takes the co-dependent nature of these behaviors into consideration, ultimately reducing bias in estimates [46]. The more recent scoping review by de Lannoy et al. [43] captured many more articles (n = 42) that examined associations between 24-h movement behaviors and mental health, including eight studies using compositional data analysis techniques. Among the studies included in their review, 21/27 (78%) and 23/27 (85%) studies that investigated indicators of mental well-being and ill-being [12], respectively, reported favorable associations with 24-h movement behaviors when assessed collectively. However, findings across analytic approaches were amalgamated, which fails to convey important insights from the different research questions examined. Beyond the literature focused on children and youth, new evidence is emerging rapidly for adults, but these findings have yet to be synthesized to gain a more comprehensive understanding of how combinations of 24-h movement behaviors relate to mental health during adulthood. If the favorable associations observed among young people extend across the broader lifespan, such findings would further support the importance of adopting the integrative whole day approach to health over the status quo of examining these behaviors in isolation. Therefore, the purpose of this study was to conduct a systematic review to examine how combinations of 24-h movement behaviors relate to indicators of mental ill-being and well-being across the lifespan.
Methods
Protocol and registration
This review was prospectively registered with the International Prospective Register of Systematic Reviews (PROSPERO; submitted July 13, 2022; ID: CRD42022345672). The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed [47], and items are reported using the PRISMA Checklist (see Additional file 1).
Inclusion criteria
We included studies that met the following criteria: (a) measured all three movement behaviors (i.e., physical activity, sedentary/screen time, sleep duration); (b) assessed at least one emotional or psychological indicator of mental well-being (e.g., flourishing, life satisfaction, self-esteem) or ill-being (e.g., depressive symptoms, psychological distress, suicidal ideation); (c) examined the effect sizes of associations between 24-h movement behavior combinations with at least one mental health indicator (e.g., regression coefficients, odds ratios, risk ratios, etc.); (d) were published after 2009; and (e) were published in the English language. Mental health was operationalized as a multidimensional construct involving facets of either mental well-being or ill-being based on Keyes’ [9] dual continua model. Emotional and psychological indicators of mental health were focused on given their introspective and interconnected nature (e.g., emotional states can influence mental functioning related to thought patterns and behaviors, and vice versa). For measures of mental ill-being, these included psychiatric symptoms as well as disorders (e.g., depressive symptoms, risk of being diagnosed with depression). Measures of well-being involved a focus on positive attributes of mental health (e.g., flourishing, self-esteem) and emotions (e.g., affect, happiness). Items/scales that measured quality of life were included as an indicator of mental health if they assessed happiness or life satisfaction, which are considered aspects of mental well-being [48]. In contrast, measures of health-related quality of life (HRQoL) were excluded based on the premise that they assess health-related aspects of life quality beyond strictly mental health (e.g., physical, motor skills, social, etc.). The year 2009 was selected as the start date of our search given it preceded the first paper (to our knowledge) which acknowledged the co-dependence between movement behaviors by five years [49], and thus was expected to capture all studies that examined how combinations of 24-h movement behaviors relate to mental health. Studies were excluded if they (a) were not a peer-reviewed article (i.e., Masters thesis, PhD dissertations, conference abstracts); (b) assessed health-related quality of life or cognitive-based indicators of brain health; and (c) specified 24-h movement behaviors as the outcome as opposed to the exposure in the statistical model.
Search strategy, data extraction, and data synthesis
An electronic search was conducted in the MEDLINE, PsycINFO, Embase, and SPORTDiscus databases in July 2022 and subsequently updated in February 2023 and August 2023. These databases were searched based on their relevance to the review topic and for consistency with previous reviews examining associations between 24-h movement behaviors and mental health among children and youth that also searched these databases. A manual search of the new non-indexed Journal of Activity, Sedentary and Sleep Behaviors was also performed given the relevance of its scope to the purpose of the present review. Search terms can be found in Additional file 2. The search strategy did not specify indicators of mental health as the language used to describe such measures tends to be heterogenous and some studies simply state “health outcomes”, which would have led to exclusion at the title and abstract stage when mental health may have been assessed. References were imported to the review management software Covidence (Evidence Partners, Ottawa, ON, Canada), where duplicates were removed and titles/abstracts reviewed by two independent reviewers for initial inclusion. After initial screening, full-texts were retrieved and independently examined for final inclusion. Any conflicts during each stage were resolved through discussion amongst the research team. References of included articles and relevant reviews were further searched to identify studies which may have been missed by the database searches. Data extraction was performed independently by two reviewers and a third reviewer examined the data for consensus, and included: (a) publication year; (b) demographic measures (e.g., age, sex, country); (c) sample size; (d) measure of movement behaviors; (e) measure(s) of mental health; (f) the statistical analysis employed; and (g) key findings.
Given the heterogeneity in the samples and statistical analysis techniques used to examine the relationships between 24-h movement behaviors and indicators of mental health, a quantitative synthesis (i.e., meta-analysis) was not conducted. Therefore, we proceeded with a narrative synthesis, and studies were reviewed and compared on a variety of characteristics including: age (children and youth, adults); study design (cross-sectional, longitudinal), indicator of mental health, and statistical analysis technique employed.
Methodological quality and risk of bias assessment
All included studies used an observational design, therefore an adaptation of the National Institute of Health’s Quality Assessment Tool for Observational Cohort and Cross-sectional Studies (QATOCCS [50]) was used to assess the methodologic quality and validity of each study as well as their risk of bias. Study quality and risk of bias was assessed independently by two reviewers on the 14 criteria assessing clarity in reporting (e.g.., research question, population details), justification of methodological choices (e.g., reliability and validity of measurement tools, sample size), and use of best practices (e.g., repeated assessments, adjusting for confounders). Each study received a “yes”, “no”, or “other” response to each question to then be rated as “poor”, “fair”, or “good” based on these considerations as concerned with the exposure (i.e., 24-h movement behaviors) and outcomes of interest (i.e., indicators of mental health). The responses are intended to be used as a guide for assessing the quality and risk of bias rating, however, in line with previous work that has used ranges of scores to provide quantitative evaluations [51, 52], we considered studies with a score between ≤ 4 to be poor, 5 to 9 to be fair, and > 9 to be good.
Results
Included studies
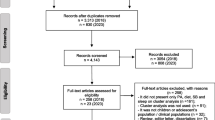
The initial search identified 11,339 records, which was reduced to 8,749 after duplicates were removed. Our updated searches in February and August identified an additional 1,366 and 890 records, which was reduced to 731 and 569 records after duplicates were removed. A total of 6 articles were identified in our manual search of the Journal of Activity, Sedentary and Sleep Behaviors. In total, 10,055 records were identified across the searches. A team of seven reviewers screened the titles and abstracts for inclusion (two independent reviewers per study), resulting in 266 records that were moved to the full text review stage. Two independent reviewers then read and assessed the full text articles for inclusion, ultimately resulting in a total of 73 studies that met all inclusion criteria. At both screening stages, any disagreements were resolved through discussion and consensus among the screening team. A PRISMA flow diagram is presented in Fig. 1.
Description of studies
Study details and outcomes are presented and briefly summarized in Table 1. Studies included were published between 2017 and 2023 with samples from 16 different countries: Canada (n = 22), United States (n = 15), China, including Hong Kong (n = 15), Australia: (n = 8), United Kingdom (n = 4), South Korea (n = 2), Spain (n = 2), Brazil (n = 2), Finland (n = 1), Japan (n = 2), New Zealand (n = 2), Singapore (n = 1), Sweden (n = 1), Switzerland (n = 1), and The Netherlands (n = 1), Belgium (n = 1). A total of 47 studies included samples of children and youth (414,542 total participants with a rangefrom 88 to 73,074 participants across studies, and ranging from 3 to 17 years of age), of which 37 used cross-sectional designs and 10 used longitudinal designs. For adults, a total of 26 studies were included in our review (183,163 participants with a range of 200 to 60,235 participants across studies, and ranging from 15 to 79 years of age), of which 21 used cross-sectional designs and five used longitudinal designs. The follow-up time ranged from 6-months to 22-years for prospective studies. A total of 65 studies included non-clinical samples (children and youth: n = 42; adults: n = 23) and 8 studies included clinical samples (children and youth: n = 5; adults: n = 3). The same datasets were used in multiple studies: two studies used the Application of integrateD Approaches to understanding Physical activity during the Transition to emerging adulthood (ADAPT) dataset [53, 54], two studies used a sample of children from two studies conducted in the United Kingdom [55, 56], two studies used the National Longitudinal Study of Adolescent to Adult Health (Add Health) [57, 58], three studies used the National Survey of Children’s Health (NSCH) [59,60,61], and the similarities of the study design and participant characteristics across three studies[62,63,64] suggested the same unnamed dataset was used. Associations between combinations of 24-h movement behaviors and indicators of mental health were assessed using seven different analytical approaches: total guideline adherence (i.e., adhering to none, one, two or all three of the guidelines), specific combinations of guideline adherence (i.e., adhering to none, physical activity, sleep, sedentary behavior/screen time, physical activity and sleep, sleep and sedentary behavior/screen time, physical activity and sedentary behavior/screen time, or all three guidelines concurrently), compositional data analysis, the Goldilocks approach (within a compositional data analysis framework, which aims to determine the optimal time-use composition for indicators of health), isotemporal substitution (traditional and compositional data analysis models), rest/activity rhythmicity, and latent profile or cluster-based analyses.
Measurement of movement behaviors
Physical activity was assessed via accelerometers in 31 studies (n = 16 for children and youth; n = 15 for adults) and using self- or proxy-reported questionnaires in 42 studies (n = 31 for children and youth; n = 11 for adults). Sedentary behavior, including recreational screen time, was assessed via accelerometers in 21 studies (n = 7 for children and youth; n = 14 for adults), self- or proxy-reported questionnaires in 50 studies (n = 38 for children and youth; n = 12 for adults), and a combination of accelerometers and self-reported questionnaires in two studies that were both conducted with samples of children and youth. Finally, sleep was assessed via accelerometers in 20 studies (n = 11 for children and youth; n = 9 for adults) and using self- or proxy-reported questionnaires in 53 studies (n = 36 for children and youth; n = 17 for adults).
Indicators of mental ill-being and well-being
Most studies (44 of 73; 60%) assessed multiple indicators of mental health. Indicators of mental well-being (i.e., positive mental health) included: flourishing (n = 5 for children and youth), quality of life (n = 3 for children and youth), self-esteem (n = 5 for children and youth), resilience (n = 6 for children and youth), life satisfaction (n = 3 for children and youth), general mental health (n = 2 for children and youth; n = 4 for adults), happiness (n = 1 for children and youth; n = 1 for adults), well-being (n = 1 for children and youth; n = 4 for adults), daily affect (n = 2 for adults) and mood states (n = 1 for adults). Indicators of mental ill-being (i.e., negative mental health) included: depression or depressive symptoms (n = 18 for children and youth; n = 13 for adults), anxiety or anxiety symptoms (n = 13 for children and youth; n = 10 for adults), psychological distress (n = 2 for children and youth; n = 4 for adults), loneliness (n = 1 for children and youth; n = 1 for adults), prolonged sadness (n = 1 for children and youth), suicidal ideation and planning (n = 2 for children and youth; n = 3 for adults), suicidal attempts (n = 2 for children and youth), total difficulty problems (n = 11 for children and youth), internalizing problems (n = 11 for children and youth), emotional dysregulation (n = 1 for children and youth), and post-traumatic stress disorder (n = 1 for adults). More associations were reported for indicators of mental ill-being (n = 127 for children and youth; n = 53 for adults) than well-being (n = 54 for children and youth; n = 26 for adults).
Some studies stratified their results by different factors including sex/gender (n = 5 studies), age groups including school grade (n = 6 studies), sleep guideline adherence (n = 2 studies), weight status (n = 1), workday vs. non workday (n = 1), weekday vs. weekend (n = 1), and chronic health conditions and disabilities (CCD; n = 1). As a result, total associations are out of the number of individual samples (i.e., a study that stratified their sample by sex/gender would be counted as two associations: one for boys and one for girls), rather than number of studies.
Associations between combinations of 24-h movement behaviors and mental health
A summary of all associations by age group (children and youth; adults), analytic approach, indicator of mental health (ill-being; well-being), and design (cross-sectional; longitudinal) is presented in Additional file 3.
Cross-sectional studies of children and youth
Total guideline adherence Among cross-sectional studies, 24/38 (63%) of the associations showed that meeting all three guidelines concurrently was correlated with favorable scores for indicators of mental health, whereas 22/38 (58%) and 23/38 (60%) associations demonstrated favorable effects for meeting one guidelines or two guidelines, respectively. When decomposed into indicators of well-being and ill-being, findings revealed 10/14 (71%), 11/14 (79%), and 11/14 (79%) associations were favorable effects when meeting one, two, or three guidelines, respectively, for indicators of mental well-being. For indicators of mental ill-being, 13/24 (54%) associations demonstrated favorable effects for meeting all three guidelines, 12/24 (50%) associations for meeting two guidelines, and 12/24 (50%) for meeting only one guideline.
Specific combinations of guideline adherence A total of 33/58 (57%) associations showed favorable effects for meeting all three guidelines concurrently. In contrast, 33/58 (57%), and 25/58 (43%), 25/58 (43%), associations demonstrated favorable effects for adherence to the screen time and sleep, physical activity and sleep, and physical activity and screen time guidelines, respectively. Specific to indicators of mental well-being, findings revealed 10/13 (77%) associations were favorable effects for adherence to all three guidelines, 8/13 (62%) for physical activity and sleep guideline adherence, 8/13 (62%) for physical activity and screen time guideline adherence, and 6/13 (46%) for screen time and sleep guideline adherence. For indicators of mental ill-being, findings revealed 23/45 (51%) associations were favorable effects for adherence to all three guidelines, 27/45 (60%) for meeting the screen time and sleep guidelines, 17/45 (38%) associations for meeting the physical activity and sleep guidelines and 17/45 (38%) associations for meeting the physical activity and screen time guidelines.
Compositional data analysis A significant relationship between the 24-h movement composition and indicators of mental health was observed in 11/20 (55%) associations. Among the studies that reported the effects of each behavior (relative to others), significant adverse associations were observed for light physical activity (2/16; 13%) and sedentary behavior (9/16; 56%), whereas significant beneficial associations were observed for sleep (6/16; 38%), MVPA (4/16; 25%) and light physical activity (1/16; 6%). Examining indicators of mental well-being and ill-being independently revealed a significant relationship for the 24-h movement composition with indicators of mental well-being in 4/7 (57%) associations and 7/13 (54%) associations for indicators of mental ill-being. Among the studies that reported the effects of each behavior (relative to others), significant favorable associations were observed for MVPA (1/3; 33%) for indicators of mental well-being and for sleep (6/13; 46%), MVPA (3/13; 23%), and light physical activity (1/13; 7%) for indicators of mental ill-being. Whereas significant adverse effects were observed for light physical activity (2/13; 15%) and sedentary behavior (9/16; 70%) for indicators of mental ill-being.
Goldilocks method The optimal 24-h movement composition for mental health was roughly 10 to 11 h of sleep; 6.5 to 8 h of sedentary time, 2 to 7 h of light physical activity, and 43 min to 2 h of MVPA in 5/5 (100%) associations. These results were consistent across the two associations for indicators of mental well-being and three associations for mental ill-being.
Rest-activity rhythmicity A significant negative relationship (more stability) was observed between inter-daily stability and indicators of mental ill-being in 1/2 (50%) associations, whereas no associations (0/2; 0%) were significant for intra-day variability. Rest-activity rhythmicity has not been examined in relation to mental well-being, to date.
Isotemporal substitution Replacing sedentary behavior with MVPA (14/17 associations; 82%) or sleep (13/17 associations; 76%) were most consistently found to be correlated with more favorable mental health scores. Reallocating sleep to MVPA was correlated with more favorable mental health scores in 4/17 (26%) associations, whereas in contrast, reallocating MVPA to sleep was correlated with more favorable mental health scores in 5/17 (29%) associations. When decomposed into indicators of well-being and ill-being, results revealed similar patterns. For mental well-being, replacing sedentary behavior with MVPA (7/8 associations; 88%) or sleep (6/8 associations; 75%) had favorable effects. For mental ill-being, replacing sedentary behavior with MVPA (8/9 associations; 89%) or sleep (7/9 associations; 78%) was correlated with favorable scores. Reallocating time from sleep to MVPA was beneficial in 3/8 associations (38%) for mental well-being compared to 1/9 associations (11%) for mental ill-being. Replacing MVPA with sleep was only beneficial for indicators of mental ill-being (5/9 associations; 56%).
Latent profile or cluster-based analyses The healthiest combination of movement behaviors (adequate sleep, high MVPA, low sedentary time) was correlated with the most favorable mental health scores across 5/5 associations (100%), followed by mixed behavioral profiles (e.g., healthy amounts of sleep and MVPA, but not screen time), and lastly, consistently unhealthy profiles (e.g., least healthy amounts of all three movement behaviors). These findings were consistent for 3/3 (100%) associations investigating indicators of mental well-being and 2/2 (100%) associations investigating mental ill-being.
Longitudinal studies of children and youth
Total guideline adherence For total guideline adherence, meeting one, two or three guidelines concurrently was correlated with favorable scores for indicators of mental health in 3/12 (25%) associations. None of the associations were significant for indicators of mental well-being (0/5; 0%), whereas 3/7 (43%) associations showed favorable effects for indicators of mental ill-being.
Specific combinations of guideline adherence Favorable mental health scores were found in 2/4 (50%) associations for meeting all three guidelines, 1/4 (25%) associations for meeting the screen time and physical activity guidelines and 3/4 (75%) associations for screen time and sleep guideline adherence. All associations investigated indicators of mental ill-being.
Compositional data analysis No associations (0/5; 0%) demonstrated a significant relationship for the 24-h movement composition with indicators of mental well-being (0/2 associations; 0%) or mental ill-being (0/3 associations; 0%).
Isotemporal substitution Akin to the cross-sectional studies among children and youth, replacing sedentary behavior with MVPA (8/8 associations; 100%) or sleep (7/8 associations; 89%) were most consistently found to be correlated with more favorable mental health scores. Comparatively, 5/8 (63%) associations found that replacing MVPA with sleep was correlated with better scores for mental health, whereas only 2/8 (26%) associations showed replacing sleep with MVPA was correlated with more favorable mental health scores. All associations investigated indicators of mental ill-being.
Latent profile or cluster-based analyses The healthiest combination of movement behaviors (adequate sleep, high MVPA, low sedentary time) was associated with the most favorable mental ill-being scores in 1/1 (100%) associations, whereas no differences were observed across the other behavioral combination profiles. Associations with indicators of mental well-being have not been examined.
Cross-sectional studies of adults
Total guideline adherence For total guideline adherence, 13/21 (62%) associations showed that meeting all three guidelines concurrently was associated with favorable effects for indicators of mental health, whereas 8/21 (38%) and 3/21 (14%) associations showed meeting two guidelines, or one guideline were associated with favorable effects, respectively. For indicators of well-being, findings revealed 1/7 (14%), 1/7 (14%), and 3/7 (43%) associations were favorable effects for adherence to one, two, and all three guidelines, respectively. For indicators of mental ill-being, a total of 2/14 (14%), 7/14 (50%), and 10/14 (71%) associations were favorable effects for adhering to one, two, and all three guidelines, respectively.
Specific combinations of guideline adherence A total of 5/8 (63%) associations demonstrated favorable effects for meeting all three guidelines concurrently, whereas 5/8 (63%), 5/8 (63%), and 4/8 (50%) associations were favorable effects for adherence to the physical activity and sleep guidelines, sedentary behavior and sleep, and physical activity and sedentary behavior guidelines, respectively. For indicators of mental well-being, results indicated a favorable effect for adhering to the physical activity and sleep guidelines in 1/1 (100%) associations. For mental ill-being, findings revealed 4/7 (57%), 4/7 (57%), 5/7 (71%), and 5/7 (71%) associations were favorable effects for adherence to the physical activity and sleep guidelines, physical activity and sedentary behavior guidelines, sleep and sedentary behavior guidelines, and all three guidelines, respectively.
Compositional data analysis A significant relationship between the 24-h movement composition and mental health was observed in 4/13 (31%) associations. Among the studies that reported the effects of each behavior (relative to others), significant favorable associations were observed for MVPA (4/10; 40%), sleep, (1/10; 10%) and light physical activity (1/10; 10%), whereas significant adverse associations were observed for sedentary behavior (2/10; 20%) and light physical activity (1/10; 10%). Among these results, findings revealed a significant relationship between the 24-h movement composition and indicators of mental well-being in 1/4 (25%) associations and 3/9 (33%) associations for indicators of mental ill-being. For studies that reported the effects of each behavior (relative to others), significant favorable effects were observed for MVPA (3/5; 60%) and light physical activity (1/5; 20%) for indicators of mental well-being and favorable effects were observed for MVPA (1/5; 20%) and sleep (1/5; 20%) for indicators of mental ill-being. Whereas adverse associations were observed for sedentary behavior (2/5; 40%) and light physical activity (1/5; 20%) for indicators of mental ill-being.
Isotemporal substitution Replacing sedentary behavior with MVPA was associated with more favorable mental health scores in 8/17 (47%) associations. Reallocating time from sedentary behavior (6/17 associations; 35%) or MVPA (1/17 associations; 6%) to sleep was found to have beneficial effects for mental health. Replacing sleep with MVPA was also found to be correlated with more favorable benefits for mental health in 5/17 (29%) associations. Finally, reallocating time from sleep (4/17; 24%) or sedentary behavior (5/14; 29%) to LPA was found to have beneficial effects for mental health. Examining indicators of mental well-being and ill-being independently revealed similar pattens. For mental well-being, replacing sedentary behavior with MVPA (2/5 associations; 40%) or sleep (2/5 associations; 40%) was associated with more favorable effects. Reallocating time from sleep (2/5 associations; 40%) or sedentary behavior (2/5 associations; 40%) to LPA was also found to be correlated with favorable benefits for mental well-being. For indicators of mental ill-being, replacing sedentary behavior with MVPA (6/12 associations; 50%) or sleep (4/12 associations; 33%) was associated with more favorable effects. Reallocating time from sleep (2/12 associations; 17%) or sedentary time (3/12 associations; 25%) to LPA was also correlated with more favorable scores for mental ill-being.
Latent profile or cluster-based analyses A total of 2/3 (67%; 2/2 for indicators of mental well-being) associations revealed the healthiest combinations of movement behaviors (adequate sleep, high MVPA, low sedentary time) was associated with the most favorable scores for mental health, followed by mixed behavioral profiles, and lastly, consistently unhealthy profiles. For indicators of mental ill-being, a total of 1/3 (33%) associations showed engaging in healthy amounts of all three behaviors, two out of three behaviors or no behaviors were associated with more favorable scores than engaging in healthy amounts of only one behavior.
Longitudinal studies of adults
Total guideline adherence For total guideline adherence, 2/2 (100%) associations (both measures of mental ill-being) showed that meeting all three guidelines concurrently was associated with favorable effects for mental health.
Compositional data analysis No associations (0/4; 0%) found a significant relationship between the 24-h movement composition and indicators of mental well-being (0/2 associations; 0%) or mental ill-being (0/2 associations; 0%).
Isotemporal substitution Replacing sedentary behavior with MVPA was correlated with more favorable mental health scores in 5/11 (45%) associations, whereas replacing sedentary behavior with sleep was only correlated with beneficial effects for mental health scores in 2/11 (18%) associations. Finally, 2/11 (18%) associations revealed that reallocating time from sleep to MVPA was associated with beneficial effects for mental health. For indicators of well-being, beneficial effects were observed in 3/5 (60%) associations when replacing sedentary time for MVPA. Reallocating time from sleep to MVPA was associated with beneficial effects for mental well-being in 2/5 (40%) associations. For mental ill-being, replacing sedentary time with MVPA (2/6 associations; 33%) or sleep (2/6 associations; 33%) was correlated with more favorable scores.
Methodological quality and risk of bias assessment
The study quality and risk of bias results are presented in Table 2. The majority of studies (n = 66; 90%) were considered to be of fair quality, with only 7 (10%) considered to be of good quality. No studies were considered of poor quality.
Discussion
This systematic review synthesized the evidence surrounding the relationships between combinations of 24-h movement behaviors—physical activity, sleep, and sedentary behaviors—and a range of different indicators of mental ill-being and well-being across the lifespan. A total of 597,705 participants from 16 different countries were represented in the 73 studies that met our inclusion criteria. The majority of studies included samples of children and youth (n = 47), though roughly one third of the studies focused on adults (n = 26). The volume of studies involving adult samples is promising given 24-h movement guidelines specific to these age groups were only released in 2020 [39]. Although more longitudinal work has been published in recent years (n = 15), the body of literature largely consists of cross-sectional studies (n = 58). Different research questions related to the associations between movement behaviors and indicators of mental health have been quantified using seven different analytical approaches, with the vast majority of studies investigating total or specific combinations of guideline adherence, followed by compositional data analysis, isotemporal substitution, latent profile or cluster-based analysis, the Goldilocks method, and rest-activity rhythmicity. The diversity of analytical methods employed in this literature highlights the complexity of quantifying these associations but converges on a critical consensus: engaging in a healthy balance of movement behaviors characterized by accruing adequate sleep, maximizing MVPA, and minimizing sedentary behaviors, regardless of age, appears to be beneficial for mental health. However, the need for more longitudinal studies and device-based measurement to improve the precision in our estimates remains to fully understand the implications of movement behaviors on mental health and to tailor recommendations that can effectively promote mental well-being and reduce ill-being across the lifespan.
At present, cross-sectional studies investigating guideline adherence, whether it be total guidelines met or specific combinations, with self- or proxy-reported measures remain dominant. From a behavioral surveillance standpoint this is not surprising given that several countries have independent recommendations for each movement behavior irrespective of whether they have adopted integrated 24-h guidelines or not, and their surveillance systems have allowed researchers to investigate the collective effects of physical activity, sedentary behavior, and sleep on outcomes such as mental health. While monitoring guideline adherence is important for the public health goal of promoting well-being in the population, the threshold-based nature of these guidelines can be limiting. Specifically, cut-point criterions neglect the dose–response nature of the relationships that have been observed between each movement behavior and indicators of mental health (e.g., [17, 65, 66]) and the co-dependent nature of 24-h movement behaviors. Nevertheless, our synthesis of the evidence generally found that adhering to an increasing number of the three guidelines was associated with more favorable scores for several indicators of mental ill-being and well-being across the lifespan, including some evidence supporting a dose–response gradient [62, 67,68,69,70,71,72,73]. While null effects were observed in several studies, over half (63% for children/youth; 62% for adults) of the cross-sectional associations, and both of the longitudinal associations for adults included in this review provided support for continuing to promote an integrated 24-h approach that targets all three behaviors. It should be noted that weakest among the evidence supporting a link between movement behaviors and mental health was the longitudinal work conducted among children and youth. One potential reason for these findings is that most of these associations were derived from studies of young children [74, 75]. Given that early childhood precedes life stages when mental health problems become more apparent (e.g., adolescence) [76], there may not be enough variance within the indicators of mental health to observe significant associations. Previous research investigating cross-sectional associations between wake-time movement compositions and mental health among preschool children supports this notion [77]. Moving forward, studies examining guideline adherence may provide a simple barometer of the importance of 24-h movement behaviors for mental health, although it should be recognized that the use of alternative approaches such as compositional data analysis may provide a more nuanced and precise understanding of these relationships.
With the prevailing shift to the 24-h movement paradigm, there has also been an emphasis on adopting device-based measures that can capture movement across the whole day. Although not without limitations, accelerometry provides an opportunity to use compositional data analysis, and therefore considers the co-dependent nature of 24-h movement behavior data. Our review found accelerometry was used most often to capture physical activity data (42% of studies), followed by sedentary behavior (32% of studies), and sleep (27% of studies). The range in usage across behaviors is interesting, but likely reflects the fact that accelerometry cannot capture recreational screen time (i.e., to assess the sedentary component of the 24-h guidelines). Additionally, protocols with hip-worn devices can be uncomfortable for participants to sleep with. Despite this disparity, a total of 19 studies (26% of those included) used compositional data analysis techniques, including 14 studies that used compositional isotemporal substitution, two studies that used the novel Goldilocks approach to identify a combination of movement behaviors that optimizes mental health, and one study that investigated rest-activity rhythmicity. This represents considerable growth since Sampasa-Kanyinga et al.'s [44] systematic review of children and youth, which identified only two studies that used compositional data analysis. The increased application of compositional data analysis techniques is indicative of its increase in popularity and uptake by researchers investigating the relationships between 24-h movement behaviors and indicators of mental health. Findings from these analyses, however, reveal disparities across the age groups and study designs to date. Specifically, 55% of the cross-sectional associations from studies of children and youth observed a significant association between the 24-h movement composition and mental health compared to only 31% for adults, with similar findings across the indicators of mental ill-being and well-being for both groups. Further, none of the nine longitudinal studies demonstrated significant associations between the 24-h movement composition at baseline and mental health at follow-up. It is worth noting that the strength of the composition-based literature is likely underestimated as several manuscripts have reported significant effects for individual behaviors within the 24-h composition (relative to others) or isotemporal substitutions (reallocating sedentary behavior to sleep or MVPA, in particular) but have overlooked reporting the full 24-h composition model. Authors of these studies suggest some of the null findings may be due to small sample sizes (i.e., limited power to detect significant effects) or limited changes in the mental health outcomes at follow up [78, 79]. Another possible explanation relates to a limitation of using devices in that they are unable to capture contextual information. The setting in which physical activity takes place (e.g., occupational versus leisure time), and the type of sedentary behavior (e.g., having coffee with a friend versus scrolling social media) could have vastly different impacts on mental health [20, 30]. Future studies that pair wearable devices with signal-contingent ecological momentary assessments are warranted as they stand to provide information related to other aspects of these behaviors beyond time-based estimates of behavioral engagement. Given the potential for improving our understanding of the relationships between 24-h movement behaviors and mental health, an emphasis should be placed on leveraging data from wearable devices as they continue to become more ubiquitous in commercial and medical use. Although strict data protection policies need to be in place, longitudinal data derived from these devices could be used in various compositional models for the purpose of improving our understanding of the causal nature of these relationships.
As previously mentioned, given that 24-h movement guidelines for children and youth guidelines were first released, there was a considerably smaller evidence base focusing on adult populations. Despite this disparity, differences and similarities in the patterns of results across the age groups deserve attention. First, adhering to all three guidelines was consistently found to most often be correlated with favorable benefits for mental health compared to meeting fewer guidelines for both children and youth (63%) as well as for adults (62%). Closer inspection of these results revealed that meeting all three guidelines was more consistently associated with indicators of mental well-being among children and youth (79% of associations versus 54% for ill-being), whereas the opposite was found for adults (71% of associations for mental ill-being versus 43% for well-being). However, considering the heterogeneity in indicators of mental health assessed, in addition to the difference in the size of the samples these inferences were drawn from, these findings should be interpreted with caution. Second, a considerable disparity was observed within the isotemporal substitution analyses wherein children and youth more consistently experience mental health benefits from replacing sedentary behavior or recreational screen time with either MVPA (82% for children and youth versus 47% for adults) or sleep (76% for children and youth versus 35% for adults), although it is important to note that the patterns of results were consistent across indicators of mental ill-being and well-being for both groups. One potential explanation for this finding could be that sedentary pursuits such as social media engagement may have a greater influence on mental health among children and youth. Specifically, harmful online feedback from peers may have a greater adverse impact on mental health during childhood and adolescence as the process of identity formation unfolds before a more fixed sense of self is recognized in adulthood [80]. Children and youth may also be more likely to struggle with regulating their emotional responses to such interactions given their prefrontal cortex has yet to mature [81]. Overall, evidence for both of these populations shows some coherence but it’s clear that more longitudinal research is needed to improve our understanding of the nature these relationships so that we can identify specific life stages when certain movement behaviors may confer the greatest benefits for mental health.
As emerging research continues to advance knowledge regarding the impacts of 24-h movement behaviors on mental health, it is clear that there are several different analytic approaches that each provides unique insight into this relationship. Studies examining guideline adherence will likely remain the foundation of this body of evidence as population-level behavioral surveillance systems continue to monitor the prevalence of 24-h guideline adherence using self- and proxy-reported surveys or a mix of self-reports and device-measured behavior. Beyond guideline adherence, the field is strongly encouraged to continue adopting compositional data analysis techniques given their appropriateness for analyzing time-use data within a fixed window (i.e., 24 h). The evidence base linking movement compositions to indicators of mental health will inevitably continue to develop in the coming years, yet findings from isotemporal studies make it clear that reallocating time from sedentary behaviors to sleep or physical activity should be prioritized in the meantime. New compositional techniques will continue to provide important insights into these relationships. For example, application of the Goldilocks method [82] has provided seminal knowledge regarding the optimal daily movement composition for indicators of mental health, whereas other emerging techniques such as the “Many roads lead to Rome” [83] approach have yet to be applied to mental health data yet but will yield important information regarding different iterations of movement compositions that can provide equivalently optimal benefits when eventually implemented. Similar to the Goldilocks method, rest-activity rhythmicity has received limited application to date but represents an excellent opportunity to understand how within- and between-day variability in sleep and movement may influence mental health. Finally, latent profile and cluster-based techniques should be considered for the purpose of identifying unique groups in the population that may stand to benefit most from targeted and tailored interventions [84]. Existing evidence has made it clear that a small fraction of the population engages in the least healthy combination of movement behaviors and membership in this group corresponds with the poorest scores on measures of mental health [53, 57, 85], which underscores the importance of allocating more public health resources to these individuals. In sum, this review has highlighted that there is currently a plethora of analytical tools at the disposal of researchers attempting to improve our current understanding of the relationship between 24-h movement behaviors and mental health, but novel techniques are emerging rapidly and should receive full consideration for the purpose of continuing to advance knowledge in this field.
With the 24-h movement paradigm receiving increasing interest as an integrative approach to promote mental well-being and prevent or manage mental ill-being, new evidence is needed to gain further insights into the interplay between the mechanisms underlying these relationships. The mechanisms that link physical activity, sedentary behaviors, and sleep with mental health are understandably complex and multifaceted, reflecting interactions across biological, psychosocial, and behavioral domains. Independent bodies of literature have provided a foundation of knowledge related to mechanisms by which each movement behavior influences indicators of mental health thus far. Sedentary behaviors, for example, have been associated with unfavorable effects on indicators of mental health via increased exposure to stressors such as negative social comparisons or cyberbullying [86,87,88], although it is important to recognize that these mechanistic pathways may be specific to recreational screen time and social media use as opposed to simply engaging in low energy expenditure behaviors. Excess sedentary behavior has also been linked to a higher likelihood of experiencing sleep disorders and disruptions [89], and the displacement of time that could be spent on physically or socially engaging activities that confer mental health benefits [90, 91]. Our isotemporal substitution findings align with this mechanistic understanding in that replacing sedentary behaviors with physical activity or sleep was found to have beneficial effects for several indicators of mental health. The mechanisms by which physical activity impacts mental health have received considerable attention to date. Specifically, biological (e.g., changes in the structural and functional composition of the brain, reduced inflammation and oxidative stress), psychosocial (e.g., social interactions, self-perceptions, interactions with the natural environment), and behavioral factors (e.g., improved sleep quantity and quality, development of self-regulatory and coping skills) have been identified as key intermediary mechanisms [92, 93]. Finally, adequate sleep has been to linked mental health—emotional regulation, depression, anxiety, and stress-related disorders in particular—via reducing cellular inflammation, stimulating or attenuating brain neurotransmitter activity (e.g., via the adenosinergic receptor system), and optimizing hypothalamic–pituitary–adrenal axis functioning, which plays a role in stress reactivity [94,95,96,97,98]. While these examples of mechanistic pathways are not exhaustive by any means, the overarching focus on how time-based estimates of movement behaviors relate to indicators of mental health obfuscates the impact of other relevant aspects of these behaviors such as quality-based (e.g., sleep quality, quality physical activity participation experiences [99, 100] and contextual factors (e.g., physical activity setting, sedentary behavior domains [20, 30]. Capturing data about these other important aspects of movement behaviors will help to elucidate the mechanisms underlying relationships with indicators of mental health. Doing so is critical for informing the development of tailored interventions that promote the optimal aspects of 24-h movement behaviors collectively to address the mental health issues facing society today.
Despite addressing an existing knowledge gap, this review is not without limitations. First, most studies have used cross-sectional designs which limits our ability to make causal inferences. While the recency of existing 24-h movement guidelines has certainly contributed to the lack of longitudinal work, researchers are encouraged to inspect older data sources as they may have included measures needed to investigate how combinations of movement behaviors influence mental health over time. Second, only studies published in English were included in the present review. We recognize that studies published in languages other than English may exist, but what was included in our search likely represents the greater majority of the literature published to date. Third, across the studies there was considerable variety in not only the tools employed to assess each movement behavior, but also in the measures of mental health outcomes. Although studies included measures that have shown strong psychometric properties, heterogeneity in the assessment tools used complicates any comprehensive synthesis of the literature.
In sum, this review was the first study to synthesize the evidence examining how physical activity, sleep and sedentary behaviors collectively relate to indicators of mental ill-being and well-being across the lifespan. Taken together, and with the emergence of several advanced analytical approaches, findings reinforce the notion that time spent engaging in physical activity and sleep need to be prioritized for promoting mental health and well-being, especially when replacing sedentary pursuits such as recreational screen time. This is an emerging literature—for adults in particular—and more longitudinal work is required to make stronger inferences. Nevertheless, moving forward public health messaging should continue to shift away from a siloed approach focused on individual behaviors to instead emphasize that the whole day counts when it comes to the importance of movement for mental health and well-being.
Data availability
Not applicable.
References
GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9(2):137–50.
Piao J, Huang Y, Han C, Li Y, Xu Y, Liu Y, et al. Alarming changes in the global burden of mental disorders in children and adolescents from 1990 to 2019: a systematic analysis for the Global Burden of Disease study. Eur Child Adolesc Psychiatry. 2022;31(11):1827–45.
Santomauro DF, Herrera AMM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–12.
Chen Y, Cowden RG, Fulks J, Plake JF, VanderWeele TJ. National data on age gradients in well-being among US adults. JAMA Psychiat. 2022;79(10):1046–7.
Thygesen LC, Møller SP, Ersbøll AK, Santini ZI, Nielsen MBD, Grønbæk MK, et al. Decreasing mental well-being during the COVID-19 pandemic: a longitudinal study among Danes before and during the pandemic. J Psychiatr Res. 2021;144:151–7.
Doran CM, Kinchin I. A review of the economic impact of mental illness. Aust Health Rev Publ Aust Hosp Assoc. 2019;43(1):43–8.
Trautmann S, Rehm J, Wittchen HU. The economic costs of mental disorders. EMBO Rep. 2016;17(9):1245–9.
Health TLG. Mental health matters. Lancet Glob Health. 2020;8(11): e1352.
Keyes CLM. The mental health continuum: from languishing to flourishing in life. J Health Soc Behav. 2002;43(2):207–22.
Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3(2):171–8.
Firth J, Ward PB, Stubbs B. Editorial: lifestyle psychiatry. Front Psychiatry. 2019. https://doi.org/10.3389/fpsyt.2019.00597.
Firth J, Solmi M, Wootton RE, Vancampfort D, Schuch FB, Hoare E, et al. A meta-review of “lifestyle psychiatry”: the role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatry. 2020;19(3):360–80.
Falck RS, Davis JC, Li L, Stamatakis E, Liu-Ambrose T. Preventing the ‘24-hour Babel’: the need for a consensus on a consistent terminology scheme for physical activity, sedentary behaviour and sleep. Br J Sports Med. 2021. https://doi.org/10.1136/bjsports-2021-104487.
Chaput JP, Carson V, Gray CE, Tremblay MS. Importance of all movement behaviors in a 24 hour period for overall health. Int J Environ Res Public Health. 2014;11(12):12575–81.
Biddle SJH, Ciaccioni S, Thomas G, Vergeer I. Physical activity and mental health in children and adolescents: an updated review of reviews and an analysis of causality. Psychol Sport Exerc. 2019;1(42):146–55.
Guo Z, Li R, Lu S. Leisure-time physical activity and risk of depression: a dose-response meta-analysis of prospective cohort studies. Medicine (Baltimore). 2022;101(30): e29917.
Pearce M, Garcia L, Abbas A, Strain T, Schuch FB, Golubic R, et al. Association between physical activity and risk of depression: a systematic review and meta-analysis. JAMA Psychiat. 2022;79(6):550–9.
Rebar AL, Stanton R, Geard D, Short C, Duncan MJ, Vandelanotte C. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol Rev. 2015;9(3):366–78.
Rosenbaum S, Tiedemann A, Sherrington C, Curtis J, Ward PB. Physical activity interventions for people with mental illness: a systematic review and meta-analysis. J Clin Psychiatry. 2014;75(9):14465.
White RL, Babic MJ, Parker PD, Lubans DR, Astell-Burt T, Lonsdale C. Domain-specific physical activity and mental health: a meta-analysis. Am J Prev Med. 2017;52(5):653–66.
Wiese CW, Kuykendall L, Tay L. Get active? A meta-analysis of leisure-time physical activity and subjective well-being. J Posit Psychol. 2018;13(1):57–66.
Netz Y, Wu MJ, Becker BJ, Tenenbaum G. Physical activity and psychological well-being in advanced age: a meta-analysis of intervention studies. Psychol Aging. 2005;20(2):272–84.
Suchert V, Hanewinkel R, Isensee B. Sedentary behavior and indicators of mental health in school-aged children and adolescents: a systematic review. Prev Med. 2015;76:48–57.
Smith L, Hamer M, Gardner B. Sedentary behavior and mental health. In: Stubbs B, Rosenbaum S, editors. Exercise-based interventions for mental illness. Cambridge: Academic Press; 2018. p. 107–19.
Hoare E, Milton K, Foster C, Allender S. The associations between sedentary behaviour and mental health among adolescents: a systematic review. Int J Behav Nutr Phys Act. 2016;13(1):108.
Teychenne M, Ball K, Salmon J. Sedentary behavior and depression among adults: a review. Int J Behav Med. 2010;17(4):246–54.
Zhang J, Yang SX, Wang L, Han LH, Wu XY. The influence of sedentary behaviour on mental health among children and adolescents: a systematic review and meta-analysis of longitudinal studies. J Affect Disord. 2022;1(306):90–114.
Rhodes RE, Mark RS, Temmel CP. Adult sedentary behavior: a systematic review. Am J Prev Med. 2012;42(3):e3-28.
Huang Y, Li L, Gan Y, Wang C, Jiang H, Cao S, et al. Sedentary behaviors and risk of depression: a meta-analysis of prospective studies. Transl Psychiatry. 2020;10(1):1–10.
Hallgren M, Dunstan DW, Owen N. Passive versus mentally active sedentary behaviors and depression. Exerc Sport Sci Rev. 2020;48(1):20–7.
Faulkner S, Bee P. Perspectives on sleep, sleep problems, and their treatment, in people with serious mental illnesses: a systematic review. PLoS ONE. 2016;11(9): e0163486.
Grandner MA. The cost of sleep lost: Implications for health, performance, and the bottom line. Am J Health Promot. 2018;32(7):1629–34.
Bacaro V, Miletic K, Crocetti E. A meta-analysis of longitudinal studies on the interplay between sleep, mental health, and positive well-being in adolescents. Int J Clin Health Psychol. 2024;24(1): 100424.
Tremblay MS, Ross R. How should we move for health? The case for the 24-hour movement paradigm. CMAJ. 2020;192(49):E1728–9.
Tremblay MS, Carson V, Chaput JP, Connor Gorber S, Dinh T, Duggan M, et al. Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2016;41(Suppl 3):S311–27.
Draper CE, Tomaz SA, Biersteker L, Cook CJ, Couper J, de Milander M, et al. The South African 24-hour movement guidelines for birth to 5 years: an integration of physical activity, sitting behavior, screen time, and sleep. J Phys Act Health. 2020;17(1):109–19.
Okely AD, Ghersi D, Hesketh KD, Santos R, Loughran SP, Cliff DP, et al. A collaborative approach to adopting/adapting guidelines - The Australian 24-Hour Movement Guidelines for the early years (Birth to 5 years): an integration of physical activity, sedentary behavior, and sleep. BMC Public Health. 2017;17(Suppl 5):869.
Reilly JJ, Hughes AR, Janssen X, Hesketh KR, Livingstone S, Hill C, et al. GRADE-ADOLOPMENT process to develop 24-hour movement behavior recommendations and physical activity guidelines for the under 5s in the United Kingdom, 2019. J Phys Act Health. 2020;17(1):101–8.
Ross R, Chaput JP, Giangregorio LM, Janssen I, Saunders TJ, Kho ME, et al. Canadian 24-hour movement guidelines for adults aged 18–64 years and adults aged 65 years or older: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2020;45(Suppl. 2):S57-102.
Tremblay MS, Chaput JP, Adamo KB, Aubert S, Barnes JD, Choquette L, et al. Canadian 24-hour movement guidelines for the early years (0–4 years): an integration of physical activity, sedentary behaviour, and sleep. BMC Public Health. 2017;17(Suppl 5):874.
Rollo S, Antsygina O, Tremblay MS. The whole day matters: Understanding 24-hour movement guideline adherence and relationships with health indicators across the lifespan. J Sport Health Sci. 2020;9(6):493–510.
Saunders TJ, Gray CE, Poitras VJ, Chaput JP, Janssen I, Katzmarzyk PT, et al. Combinations of physical activity, sedentary behaviour and sleep: relationships with health indicators in school-aged children and youth. Appl Physiol Nutr Metab Physiol Appl Nutr Metab. 2016;41(6 Suppl 3):S283-293.
de Lannoy L, Barbeau K, Vanderloo LM, Goldfield G, Lang JJ, MacLeod O, et al. Evidence supporting a combined movement behavior approach for children and youth’s mental health – a scoping review and environmental scan. Ment Health Phys Act. 2023;1(24): 100511.
Sampasa-Kanyinga H, Colman I, Goldfield GS, Janssen I, Wang J, Podinic I, et al. Combinations of physical activity, sedentary time, and sleep duration and their associations with depressive symptoms and other mental health problems in children and adolescents: a systematic review. Int J Behav Nutr Phys Act. 2020;17(1):72.
Wilhite K, Booker B, Huang BH, Antczak D, Corbett L, Parker P, et al. Combinations of physical activity, sedentary behavior, and sleep and their associations with physical, psychological, and educational outcomes in children and adolescents: a systematic review. Am J Epidemiol. 2022;14: kwac212.
Dumuid D, Stanford TE, Martin-Fernández JA, Pedišić Ž, Maher CA, Lewis LK, et al. Compositional data analysis for physical activity, sedentary time and sleep research. Stat Methods Med Res. 2018;27(12):3726–38.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;21(339): b2535.
Westerhof GJ, Keyes CLM. Mental illness and mental health: the two continua model across the lifespan. J Adult Dev. 2010;17(2):110–9.
Pedišić Ž. Measurement issues and poor adjustments for physical activity and sleep undermine sedentary behaviour research—the focus should shift to the balance between sleep, sedentary behaviour, standing and activity. Kinesiology. 2014;46(1):135–46.
National Institutes of Health. National Institutes of Health quality assessment tool for observational cohort and cross-sectional studies. Bethesda: NIH; 2016.
Madigan S, Prime H, Graham SA, Rodrigues M, Anderson N, Khoury J, et al. Parenting behavior and child language: a meta-analysis. Pediatrics. 2019;144(4): e20183556.
Vizheh M, Qorbani M, Arzaghi SM, Muhidin S, Javanmard Z, Esmaeili M. The mental health of healthcare workers in the COVID-19 pandemic: a systematic review. J Diabetes Metab Disord. 2020;19(2):1967–78.
Brown DMY, Cairney J, Kwan MY. Adolescent movement behaviour profiles are associated with indicators of mental wellbeing. Ment Health Phys Act. 2021;1(20): 100387.
Brown DMY, Kwan MYW. Movement behaviors and mental wellbeing: a cross-sectional isotemporal substitution analysis of Canadian adolescents. Front Behav Neurosci. 2021;15: 736587.
Fairclough SJ, Tyler R, Dainty JR, Dumuid D, Richardson C, Shepstone L, et al. Cross-sectional associations between 24-hour activity behaviours and mental health indicators in children and adolescents: a compositional data analysis. J Sports Sci. 2021;39(14):1602–14.
Fairclough SJ, Clifford L, Brown D, Tyler R. Characteristics of 24-hour movement behaviours and their associations with mental health in children and adolescents. J Act Sedentary Sleep Behav. 2023;2(1):11.
Brown DMY, Kwan MY, Arbour-Nicitopoulos KP, Cairney J. Identifying patterns of movement behaviours in relation to depressive symptoms during adolescence: a latent profile analysis approach. Prev Med. 2021;1(143): 106352.
García-Hermoso A, Ezzatvar Y, Ramírez-Vélez R, López-Gil JF, Izquierdo M. Trajectories of 24-h movement guidelines from middle adolescence to adulthood on depression and suicidal ideation: a 22-year follow-up study. Int J Behav Nutr Phys Act. 2022;19(1):135.
Brown DMY, McPhee PG, Kwan MY, Timmons BW. Implications of disability severity on 24-hour movement guideline adherence among children with neurodevelopmental disorders in the United States. J Phys Act Health. 2021;18(11):1325–31.
Brown DMY, Ronen GM. Associations between 24-hour movement guideline adherence and mental health disorders among young people with active and inactive epilepsy. Epilepsy Behav. 2021;1(125): 108386.
Zhu X, Haegele JA, Healy S. Movement and mental health: behavioral correlates of anxiety and depression among children of 6–17 years old in the U.S. Ment Health Phys Act. 2019;16:60–5.
Bu H, He A, Gong N, Huang L, Liang K, Kastelic K, et al. Optimal movement behaviors: correlates and associations with anxiety symptoms among Chinese university students. BMC Public Health. 2021;21(1):2052.
Chao L, Ma R, Jiang W. Movement behaviours and anxiety symptoms in Chinese college students: a compositional data analysis. Front Psychol. 2022. https://doi.org/10.3389/fpsyg.2022.952728.
Liang K, de Lucena Martins CM, Chen ST, Clark CCT, Duncan MJ, Bu H, et al. Sleep as a priority: 24-hour movement guidelines and mental health of Chinese college students during the COVID-19 pandemic. Healthcare. 2021;9(9):1166.
Chiu HY, Lee HC, Chen PY, Lai YF, Tu YK. Associations between sleep duration and suicidality in adolescents: a systematic review and dose-response meta-analysis. Sleep Med Rev. 2018;42:119–26.
Liu M, Wu L, Yao S. Dose–response association of screen time-based sedentary behaviour in children and adolescents and depression: a meta-analysis of observational studies. Br J Sports Med. 2016;50(20):1252–8.
Carson V, Ezeugwu VE, Tamana SK, Chikuma J, Lefebvre DL, Azad MB, et al. Associations between meeting the Canadian 24-hour movement guidelines for the early years and behavioral and emotional problems among 3-year-olds. J Sci Med Sport. 2019;22(7):797–802.
Feng J, Huang WY, Lau PWC, Wong SHS, Sit CHP. Movement behaviors and mental health of caregivers of preschoolers in China during the COVID-19 pandemic. Prev Med. 2022;155: 106913.
Janssen I, Roberts KC, Thompson W. Is adherence to the Canadian 24-hour movement behaviour guidelines for children and youth associated with improved indicators of physical, mental, and social health? Appl Physiol Nutr Metab. 2017;42(7):725–31.
Li C, Haegele JA, Sun F, Alves MLT, Ang SHC, Lee J, et al. Meeting the 24-h movement guidelines and health-related outcomes among youth with autism spectrum disorder: a seven-country observational study. Child Adolesc Psychiatry Ment Health. 2022;16(1):50.
Peralta GP, Camerini AL, Haile SR, Kahlert CR, Lorthe E, Marciano L, et al. Lifestyle behaviours of children and adolescents during the first two waves of the COVID-19 pandemic in Switzerland and their relation to well-being: an observational study. Int J Public Health. 2022;67:1604978.
Sampasa-Kanyinga H, Lien A, Hamilton HA, Chaput JP. Canadian 24-h movement guidelines, life stress, and self-esteem among adolescents. Front Public Health. 2022;10: 702162.
Wang W, Haegele JA, Wu Y, Li C. Meeting the 24-hour movement guidelines and outcomes in adolescents with ADHD: a cross-sectional observational study. Int J Environ Res Public Health. 2022;19(4):2132.
McNeill J, Howard SJ, Vella SA, Cliff DP. Compliance with the 24-Hour movement guidelines for the early years: cross-sectional and longitudinal associations with executive function and psychosocial health in preschool children. J Sci Med Sport. 2020;23(9):846–53.
Taylor RW, Haszard JJ, Healey D, Meredith-Jones KA, Taylor BJ, Galland BC. Adherence to 24-h movement behavior guidelines and psychosocial functioning in young children: a longitudinal analysis. Int J Behav Nutr Phys Act. 2021;18(1):110.
Solmi M, Radua J, Olivola M, Croce E, Soardo L, de Pablo GS, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. 2022;27(1):281–95.
Brown DMY, Kwan MYW, King-Dowling S, Cairney J. Cross-sectional associations between wake-time movement compositions and mental health in preschool children with and without motor coordination problems. Front Pediatr. 2021. https://doi.org/10.3389/fped.2021.752333.
Chong KH, Parrish AM, Cliff DP, Dumuid D, Okely AD. Cross-sectional and longitudinal associations between 24-hour movement behaviours, recreational screen use and psychosocial health outcomes in children: a compositional data analysis approach. Int J Environ Res Public Health. 2021;18(11):5995.
Cabanas-Sánchez V, Esteban-Cornejo I, García-Esquinas E, Ortolá R, Ara I, Rodríguez-Gómez I, et al. Cross-sectional and prospective associations of sleep, sedentary and active behaviors with mental health in older people: a compositional data analysis from the Seniors-ENRICA-2 study. Int J Behav Nutr Phys Act. 2021;18(1):124.
Demo DH. The self-concept over time: research issues and directions. Annu Rev Sociol. 1992;18(1):303–26.
Arain M, Haque M, Johal L, Mathur P, Nel W, Rais A, et al. Maturation of the adolescent brain. Neuropsychiatr Dis Treat. 2013;9:449–61.
Dumuid D, Olds T, Lange K, Edwards B, Lycett K, Burgner DP, et al. Goldilocks days: optimising children’s time use for health and well-being. J Epidemiol Community Health. 2022;76(3):301–8.
Dumuid D, Mellow ML, Stanford TE, Chong KH, Sawyer SM, Smith AE, et al. Many different roads lead to Rome: equivalence of time-use for activity, sedentary and sleep behaviours and dietary intake profiles among adolescents. J Act Sedentary Sleep Behav. 2022;1(1):6.
Morgan PJ, Young MD, Smith JJ, Lubans DR. Targeted health behavior interventions promoting physical activity: a conceptual model. Exerc Sport Sci Rev. 2016;44(2):71–80.
Brown DMY, Hill RM, Wolf JK. Cross-sectional associations between 24-h movement guideline adherence and suicidal thoughts among Canadian post-secondary students. Ment Health Phys Act. 2022;1(23): 100484.
Kwan I, Dickson K, Richardson M, MacDowall W, Burchett H, Stansfield C, et al. Cyberbullying and children and young people’s mental health: a systematic map of systematic reviews. Cyberpsychology Behav Soc Netw. 2020;23(2):72–82.
Ademiluyi A, Li C, Park A. Implications and preventions of cyberbullying and social exclusion in social media: systematic review. JMIR Form Res. 2022;6(1): e30286.
Geng J, Wang Y, Wang H, Wang P, Lei L. Social comparison orientation and cyberbullying perpetration and victimization: roles of envy on social networking sites and body satisfaction. J Interpers Violence. 2022;37(17–18):NP16060–83.
Yang Y, Shin JC, Li D, An R. Sedentary behavior and sleep problems: a systematic review and meta-analysis. Int J Behav Med. 2017;24(4):481–92.
Park JH, Moon JH, Kim HJ, Kong MH, Oh YH. Sedentary lifestyle: overview of updated evidence of potential health risks. Korean J Fam Med. 2020;41(6):365–73.
Mutz DC, Roberts DF, Van Vuuren DP. Reconsidering the displacement hypothesis: television’s influence on children’s time use. Commun Res. 1993;20(1):51–75.
Lubans D, Richards J, Hillman C, Faulkner G, Beauchamp M, Nilsson M, et al. Physical activity for cognitive and mental health in youth: a systematic review of mechanisms. Pediatrics. 2016;138(3): e20161642.
Kandola A, Ashdown-Franks G, Hendrikse J, Sabiston CM, Stubbs B. Physical activity and depression: towards understanding the antidepressant mechanisms of physical activity. Neurosci Biobehav Rev. 2019;1(107):525–39.
Chellappa SL, Aeschbach D. Sleep and anxiety: from mechanisms to interventions. Sleep Med Rev. 2022;1(61): 101583.
Germain A, Buysse DJ, Nofzinger E. Sleep-specific mechanisms underlying posttraumatic stress disorder: integrative review and neurobiological hypotheses. Sleep Med Rev. 2008;12(3):185–95.
Richards A, Kanady JC, Neylan TC. Sleep disturbance in PTSD and other anxiety-related disorders: an updated review of clinical features, physiological characteristics, and psychological and neurobiological mechanisms. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol. 2020;45(1):55–73.
Fang H, Tu S, Sheng J, Shao A. Depression in sleep disturbance: a review on a bidirectional relationship, mechanisms and treatment. J Cell Mol Med. 2019;23(4):2324–32.
van Dalfsen JH, Markus CR. The influence of sleep on human hypothalamic–pituitary–adrenal (HPA) axis reactivity: a systematic review. Sleep Med Rev. 2018;1(39):187–94.
Martin Ginis KA, Gee CM, Sinden AR, Tomasone JR, Latimer-Cheung AE. Relationships between sport and exercise participation and subjective well-being among adults with physical disabilities: is participation quality more important than participation quantity? Psychol Sport Exerc. 2024;1(70): 102535.
Scott AJ, Webb TL, Martyn-St James M, Rowse G, Weich S. Improving sleep quality leads to better mental health: a meta-analysis of randomised controlled trials. Sleep Med Rev. 2021;1(60): 101556.
Baillot A. Health associations with meeting the new Canadian 24-hour movement guidelines recommendations according to body mass index classes in Canadian adults. Health Rep. 2022;33(82):3–15.
Bang F, Roberts KC, Chaput JP, Goldfield GS, Prince SA. Physical activity, screen time and sleep duration: combined associations with psychosocial health among Canadian children and youth. Health Rep. 2020;31(5):9–16.
Blodgett JM, Mitchell JJ, Stamatakis E, Chastin S, Hamer M. Associations between the composition of daily time spent in physical activity, sedentary behaviour and sleep and risk of depression: compositional data analyses of the 1970 British cohort Study. J Affect Disord. 2023;320:616–20.
Brown DMY, Faulkner GEJ, Kwan MYW. Healthier movement behavior profiles are associated with higher psychological wellbeing among emerging adults attending post-secondary education. J Affect Disord. 2022;15(319):511–7.
Burns RD, Bai Y, Pfledderer CD, Brusseau TA, Byun W. Movement behaviors and perceived loneliness and sadness within alaskan adolescents. Int J Environ Res Public Health. 2020;17(18):6866.
Cao R, Gao T, Hu Y, Qin Z, Ren H, Liang L, et al. Clustering of lifestyle factors and the relationship with depressive symptoms among adolescents in Northeastern China. J Affect Disord. 2020;274:704–10.
Christian H, Murray K, Trost SG, Schipperijn J, Trapp G, Maitland C, et al. Meeting the Australian 24-hour movement guidelines for the early years is associated with better social-emotional development in preschool boys. Prev Med Rep. 2022;27: 101770.
Colley RC. Reallocating time between sleep, sedentary and active behaviours: associations with obesity and health in Canadian adults. Health Rep. 2018;29(82):3–13.
Curtis RG, Dumuid D, Olds T, Plotnikoff R, Vandelanotte C, Ryan J, et al. The association between time-use behaviors and physical and mental well-being in adults: a compositional isotemporal substitution analysis. J Phys Act Health. 2020;17(2):197–203.
Curtis RG, Dumuid D, McCabe H, Singh B, Ferguson T, Maher C. The association between 24-hour activity, sedentary and sleep compositions and mental health in Australian adults: a cross-sectional study. J Act Sedentary Sleep Behav. 2023;2(1):15.
de Faria FR, Barbosa D, Howe CA, Canabrava KLR, Sasaki JE, Dos Santos Amorim PR. Time-use movement behaviors are associated with scores of depression/anxiety among adolescents: a compositional data analysis. PLoS ONE. 2022;17(12): e0279401.
Del Pozo CB, Alfonso-Rosa RM, McGregor D, Chastin SF, Palarea-Albaladejo J, Del Pozo CJ. Sedentary behaviour is associated with depression symptoms: compositional data analysis from a representative sample of 3233 US adults and older adults assessed with accelerometers. J Affect Disord. 2020;265:59–62.
Duncan MJ, Riazi NA, Faulkner G, Gilchrist JD, Leatherdale ST, Patte KA. The association of physical activity, sleep, and screen time with mental health in Canadian adolescents during the COVID-19 pandemic: a longitudinal isotemporal substitution analysis. Ment Health Phys Act. 2022;23: 100473.
Fung H, Yeo BTT, Chen C, Lo JC, Chee MWL, Ong JL. Adherence to 24-hour movement recommendations and health indicators in early adolescence: cross-sectional and longitudinal associations in the adolescent brain cognitive development study. J Adolesc Health. 2023;72(3):460–70.
Gilchrist JD, Battista K, Patte KA, Faulkner G, Carson V, Leatherdale ST. Effects of reallocating physical activity, sedentary behaviors, and sleep on mental health in adolescents. Ment Health Phys Act. 2021;20: 100380.
Hajo S, Reed JL, Hans H, Tulloch HE, Reid RD, Prince SA. Physical activity, sedentary time and sleep and associations with mood states, shift work disorder and absenteeism among nurses: an analysis of the cross-sectional Champlain Nurses’ Study. PeerJ. 2020;2(8): e8464.
Hinkley T, Timperio A, Watson A, Duckham RL, Okely AD, Cliff D, et al. Prospective associations with physiological, psychosocial and educational outcomes of meeting Australian 24-hour movement guidelines for the early years. Int J Behav Nutr Phys Act. 2020;17(1):36.
Hofman A, Voortman T, Ikram MA, Luik AI. Substitutions of physical activity, sedentary behaviour and sleep: associations with mental health in middle-aged and elderly persons. J Epidemiol Community Health. 2022;76(2):175–81.
Hou M, Herold F, Healy S, Haegele JA, Block ME, Ludyga S, et al. 24-Hour movement behaviors among visually impaired US children and adolescents. Ment Health Phys Act. 2023;1(25): 100545.
Kandola AA, del Pozo CB, Osborn DPJ, Stubbs B, Choi KW, Hayes JF. Impact of replacing sedentary behaviour with other movement behaviours on depression and anxiety symptoms: a prospective cohort study in the UK Biobank. BMC Med. 2021;19(1):133.
Kitano N, Kai Y, Jindo T, Tsunoda K, Arao T. Compositional data analysis of 24-hour movement behaviors and mental health in workers. Prev Med Rep. 2020;20: 101213.
Kuzik N, Naylor PJ, Spence JC, Carson V. Movement behaviours and physical, cognitive, and social-emotional development in preschool-aged children: cross-sectional associations using compositional analyses. PLoS ONE. 2020;15(8): e0237945.
Kuzik N, Spence JC, Arkko K, Blye CJ, Davie J, Duddridge R, et al. Associations between meeting the Canadian 24-hour movement guidelines and physical, cognitive, social-emotional, and overall development in early childhood. J Act Sedentary Sleep Behav. 2022;1(1):2.
Larisch LM, Kallings LV, Hagströmer M, Desai M, von Rosen P, Blom V. Associations between 24 h movement behavior and mental health in office workers. Int J Environ Res Public Health. 2020;17(17):6214.
Le F, Yap Y, Tung NYC, Bei B, Wiley JF. The associations between daily activities and affect: a compositional isotemporal substitution analysis. Int J Behav Med. 2022;29(4):456–68.
Lee EY, Spence JC, Tremblay MS, Carson V. Meeting 24-hour movement guidelines for children and youth and associations with psychological well-being among South Korean adolescents. Ment Health Phys Act. 2018;14:66–73.
Liang K, Chen S, Chi X. Differential associations between meeting 24-hour movement guidelines with mental wellbeing and mental illness among Chinese adolescents. J Adolesc Health. 2023;72(5):658–66.
Liu BP, Jia CX, Li SX. The association of soft drink consumption and the 24-hour movement guidelines with suicidality among adolescents of the United States. Nutrients. 2022;14(9):1870.
López-Gil JF, Roman-Viñas B, Aznar S, Tremblay MS. Meeting 24-h movement guidelines: prevalence, correlates, and associations with socioemotional behavior in Spanish minors. Scand J Med Sci Sports. 2022;32(5):881–91.
Lu S, Cheval B, Yu Q, Hossain MM, Chen ST, Taylor A, et al. Associations of 24-hour movement behavior with depressive symptoms and anxiety in children: cross-sectional findings from a Chinese sample. Healthc Basel Switz. 2021;9(11):1532.
Luo L, Cao Y, Hu Y, Wen S, Tang K, Ding L, et al. The Associations between meeting 24-hour movement guidelines (24-HMG) and self-rated physical and mental health in older adults-cross sectional evidence from China. Int J Environ Res Public Health. 2022;19(20):13407.
Luo L, Zeng X, Cao Y, Hu Y, Wen S, Tang K, et al. The associations between meeting 24-hour movement guidelines (24-HMG) and mental health in adolescents—cross sectional evidence from China. Int J Environ Res Public Health. 2023;20(4):3167.
Meyer JD, Ellingson LD, Buman MP, Shook RP, Hand GA, Blair SN. Current and 1-year psychological and physical effects of replacing sedentary time with time in other behaviors. Am J Prev Med. 2020;59(1):12–20.
Ohta T, Ogawa M, Kikuchi N, Sasai H, Okamoto T. Adherence to 24-h movement guidelines and depressive status during the coronavirus disease outbreak: a cross-sectional Japanese survey. Int J Public Health. 2023;68:1604647.
Perez LG, Dong L, Beckman R, Meadows SO. Movement behaviors associated with mental health among US military service members. Mil Psychol. 2022;34(2):211–23.
Porter CD, McPhee PG, Kwan MY, Timmons BW, Brown DMY. 24-hour movement guideline adherence and mental health: a cross-sectional study of emerging adults with chronic health conditions and disabilities. Disabil Health J. 2023;16(3): 101476.
Sampasa-Kanyinga H, Chaput JP, Goldfield GS, Janssen I, Wang J, Hamilton HA, et al. 24-hour movement guidelines and suicidality among adolescents. J Affect Disord. 2020;1(274):372–80.
Sampasa-Kanyinga H, Colman I, Dumuid D, Janssen I, Goldfield GS, Wang JL, et al. Longitudinal association between movement behaviours and depressive symptoms among adolescents using compositional data analysis. PLoS ONE. 2021;16(9): e0256867.
Sampasa-Kanyinga H, Chaput JP, Goldfield GS, Janssen I, Wang J, Hamilton HA, et al. The Canadian 24-hour movement guidelines and psychological distress among adolescents: les directives canadiennes en matière de mouvement sur 24 heures et la détresse psychologique chez les adolescents. Can J Psychiatry Rev Can Psychiatr. 2021;66(7):624–33.
Sampasa-Kanyinga H, Colman I, Goldfield GS, Janssen I, Wang J, Tremblay MS, et al. 24-hour movement behaviors and internalizing and externalizing behaviors among youth. J Adolesc Health. 2021;68(5):969–77.
Sampasa-Kanyinga H, Lien A, Hamilton HA, Chaput JP. The Canadian 24-hour movement guidelines and self-rated physical and mental health among adolescents. Can J Public Health Rev Can Sante Publique. 2022;113(2):312–21.
St. Laurent CW, Rasmussen CL, Holmes JF, Cremone-Caira A, Kurdziel LBF, Desrochers PC, et al. Associations of activity, sedentary, and sleep behaviors with cognitive and social-emotional health in early childhood. J Act Sedentary Sleep Behav. 2023;2(1):7.
Sun J, Jiang X, Wei S. Combinations of physical activity, screen time and sleep, and their association with subjective wellbeing in children. Complement Ther Clin Pract. 2023;51: 101720.
Taylor RW, Haszard JJ, Meredith-Jones KA, Azeem AA, Galland BC, Heath ALM, et al. Associations between activity, sedentary and sleep behaviours and psychosocial health in young children: a longitudinal compositional time-use study. J Act Sedentary Sleep Behav. 2023;2(1):3.
Vanderlinden J, Biddle GJH, Boen F, van Uffelen JGZ. To be well or not to be well: compositional associations of physical activity, sedentary behaviour and sleep with mental well-being in Flemish adults aged 55+ years. J Act Sedentary Sleep Behav. 2023;2(1):9.
Zhang X, Mao F, Wu L, Zhang G, Huang Y, Chen Q, et al. Associations of physical activity, sedentary behavior and sleep duration with anxiety symptoms during pregnancy: an isotemporal substitution model. J Affect Disord. 2022;1(300):137–44.
Zhang Y, Pan Y, Ma Z, Wang D, Zou R, Fan F. Cross-sectional and longitudinal associations of adherence to the 24-hour movement guidelines with mental health problems among Chinese adolescents. J Psychosom Res. 2023;170: 111352.
Zhu N, Guo H, Ma D, Wang Q, Ma J, Kim H. The association between 24 h movement guidelines and internalising and externalising behaviour problems among Chinese preschool children. Children. 2023;10(7):1146.
Author information
Authors and Affiliations
Contributions
CG: Methodology, Writing—Original Draft; Data Curation; CH: Data Curation, Writing—Review & Editing; CP: Data Curation; BS: Data Curation; IS: Data Curation; BW: Data Curation; MH: Methodology, Data Curation; MK: Methodology, Writing—Review & Editing; DB: Conceptualization, Methodology, Writing—Original Draft, Data Curation, Supervision. All authors have read and approved the final version of the manuscript and agree with the order of presentation of the authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. PRISMA Checklist and Abstract Checklist.
Additional file 2.
Search terms.
Additional file 3.
Table by associations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Groves, C.I., Huong, C., Porter, C.D. et al. Associations between 24-h movement behaviors and indicators of mental health and well-being across the lifespan: a systematic review. JASSB 3, 9 (2024). https://doi.org/10.1186/s44167-024-00048-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44167-024-00048-6