Abstract
Background
Candida albicans is an opportunistic human fungal pathogen responsible for superficial and systemic life-threatening infections. Treating these infections is challenging as many clinical isolates show increased drug resistance to antifungals. Chromosome (Chr) 4 monosomy was implicated in a fluconazole-resistant mutant. However, exposure to fluconazole adversely affects Candida cells and can generate numerous mutations. Hence, the present study aimed to truncate Chr4 and challenge the generated Candida strains to antifungals and evaluate their role in drug response.
Results
Herein, Chr4 was truncated in C. albicans using the telomere-mediated chromosomal truncation method. The resulting eight Candida strains carrying one truncated homolog of Chr4 were tested for response to multiple antifungals. The minimal inhibitory concentration (MIC) for these strains was determined against three classes of antifungals. The MIC values against fluconazole, amphotericin B, and caspofungin were closer to that of the wild type strain. Microdilution assay against fluconazole showed that the mutants and wild type strains had similar sensitivity to fluconazole. The disc diffusion assay against five azoles and two polyenes revealed that the zones of inhibition for all the eight strains were similar to those of the wild type. Thus, none of the generated strains showed any significant resistance to the tested antifungals. However, spot assay exhibited a reasonably high tolerance of a few generated strains with increasing concentrations of fluconazole.
Conclusion
This analysis suggested that Chr4 aneuploidy might not underlie drug resistance but rather drug tolerance in Candida albicans.
Similar content being viewed by others
Background
Candida albicans is a diploid polymorphic fungus that grows as yeast with pseudohyphae and true hyphae [1, 2]. It resides as a harmless commensal on the skin and in the mucosal lining of the gastrointestinal and genitourinary tracts in humans and is the most prevalent fungal pathogen that can cause both superficial (such as oral and vaginal candidiasis) and systemic infections [3, 4]. Systemic infections are life-threatening and common in immunologically weak individuals, such as HIV patients, neonates with low birth weight, transplant recipients, and chemotherapy patients [5]. Several other species of Candida, including C. glabrata, C. tropicalis, C. parapsilosis, C. haemulonii, and C. krusei were also isolated from clinical samples; however, C. albicans remains the most common fungal pathogen [6]. Several potential antifungals are extensively used in clinical settings for the treatment and management of Candida infections. Based on the chemical compositions, the antifungals are classified into several groups: polyenes, pyrimidine analogs, echinocandins, thiocarbamates, allylamines, azoles, and morpholines [7]. These drugs inhibit the biosynthesis of crucial molecules, such as ergosterol and β-1,3-glucan, which are essential components of the fungal cell. Some antifungals can perforate the cell wall leading to the death of the fungi [8, 9]. Intriguingly, the clinical isolates are becoming increasingly resistant to the available antifungals, which pose a threat to the treatment and management of Candida infections, especially bloodstream infections [10, 11].
The drug resistance in C. albicans has been studied extensively in the last two decades to comprehend the underlying mechanism. It seems to have developed drug resistance via overexpression of drug transporters, alterations of drug targets, utilization of compensatory and catabolic pathways, and biofilm formation [11,12,13]. However, the ABC (ATP-binding cassette) (Cdr1p, Cdr2p) and major facilitator superfamily (MFS) (Mdr1p) transporters are considered the major contributors to drug resistance in C. albicans [13, 14].
Moreover, the modifications or alterations of biosynthetic pathways significantly contribute to drug resistance in this fungal pathogen. For example, the azole drugs (including fluconazole) inhibit the enzyme 14-alpha lanosterol demethylase (encoded by the ERG11 gene) required for the biosynthesis of ergosterol. However, multiple mutations in the ERG11 gene (encoding lanosterol 14α-demethylase) make inactive these drugs against C. albicans [15]. In addition, mutations in ERG3 (encoding sterol Δ5,6 desaturase) render resistance to Candida cells as the mutated enzyme fails to convert 14α-methylated sterols into toxic 3,6-diol derivatives [16]. Moreover, the effect of the toxic compound, 5-fluorocytosine (5-FC), is nullified by incorporating the mutations in the FUR1 gene encoding uracil phosphoribosyltransferase [17]. The mutations in the FSK1 gene encoding a subunit of β-1,3-glucan synthase complex render the Candida cells resistant to echinocandins [18]. In addition, many azole-resistant clinical isolates of C. albicans acquired gain-of-function mutations in the transcription factors: Tac1p, Mrr1p, and Upc2p [19, 20], which can counteract environmental stress and survive in adverse conditions.
Furthermore, pathogenic yeast C. albicans chromosomal nondisjunction causes genetic changes in response to environmental cues [21, 22]. This phenomenon generates aneuploidies that can adapt to stressful conditions for survival. In the presence of fluconazole, nondisjunction is observed in C. albicans, giving rise to Chr4 monosomy and Chr3 trisomy. The strains bearing these alterations become resistant to fluconazole [23]. Interestingly, in the absence of a complete sexual cycle, C. albicans resorts to a parasexual cycle in which two diploid cells generate a tetraploid. Subsequently, the tetraploids undergo a concerted chromosome loss and generate multiple aneuploidies, i.e., it can generate numerous changes in the genome, including but not limited to genome organization and variations in chromosome copy number. The Candida cells grown under high concentrations of fluconazole can incorporate numerous changes in the whole genome [23]. Therefore, the presence of Chr4 monosomy in fluconazole-resistant mutants might not confer fluconazole resistance.
Hence, a systematic chromosomal truncation approach should be applied to validate Chr4 monosomy and its relation to fluconazole resistance. This method was successfully applied to understand the regulation of L-sorbose utilization in C. albicans [24, 25]. Therefore, in this study, we adopted the telomere-mediated chromosomal truncation method [24] to truncate Chr4 and assess the response of the isoform against antifungals. Herein, we have carried out eight systematic truncations in one of the homologs of Chr4, whereas the second homolog remains intact. Next, the strains carrying the truncated Chr4 were tested against three classes of commonly used antifungals: azoles, polyenes, and echinocandins. This systematic study suggested that Chr4 may not be involved in drug resistance. However, it could play an essential role in the drug tolerance of this pathogen.
Methods
Strains, media, and growth conditions
C. albicans strain CAF4-2 (∆ura3::imm434/∆ura3::imm434) was used for chromosomal truncations [26]. The yeast Saccharomyces cerevisiae strain B-8728 (MATa ura3-52 trp1-Δ63 leu2-Δ1 GAL2) was used to prepare the chromosomal size marker (obtained from Fred Sherman, University of Rochester, USA). Escherichia coli strain XL-1 Blue was used for creating the plasmid constructs and routine amplification of plasmids [27].
Yeast extract/peptone/dextrose (YPD) and synthetic media were prepared as described previously [28]. Uridine was added at a concentration of 50 μg/mL to the media as required. All the strains were routinely grown at 30 °C. Fluconazole (Sigma, USA) solution (10 mg/mL) was prepared in dimethyl sulfoxide (DMSO). The bacterial strains were grown in YT media (0.5% sodium chloride, 0.5% yeast extract, and 1% tryptone) at 37 °C. The E. coli strains containing plasmids were grown in YT media containing 100 μg/mL ampicillin. The stock solution of zymolyase (Sigma) (1 mg/mL) was prepared in 15% glycerol and stored at − 20 °C. Mueller-Hinton agar plates (Himedia, Mumbai, India) were used for minimum inhibition concentration (MIC) and disc diffusion assays.
Molecular biology methods
Molecular biology methods, including restriction digestion of plasmids, gel elution of DNA fragments, ligation of DNA fragments into vectors, and polymerase chain reaction (PCR), were carried out as described previously [29]. Plasmids from E. coli were isolated using the alkaline lysis method [30]. E. coli transformation was carried out using the calcium chloride method [29], and C. albicans transformation was performed using the spheroplast method [31, 32].
Vectors and plasmid constructions
The pSFU1 plasmid containing a URA3 flipper was a kind gift from J. Morshhauser [33]. The plasmid “BSA” containing C. albicans telomere was obtained from McEachern and Hicks [34]. The plasmids pRC3915 (integrative plasmid) and pRC2312 (replicative plasmid) were obtained from Cannon et al. [35]. The plasmid pKA05 was constructed by subcloning a 0.75-kbp SalI-SacI fragment containing Candida telomere from the plasmid “BSA” into pSFU1 at the NotI-SacI site as described previously [25] and used as the basic plasmid for generating truncation constructs (Supplementary Fig. S1A). For truncating Chr4 at the intended sites, the DNA sequences were retrieved from the Candida Genome Database (CGD) [36], and the primers were designed (Table 1) to amplify the mapping sequence (MS). The PCR products were first cloned into pTZ57R/T vector using InsTA PCR Cloning kit (Thermo Fisher Scientific, Vilnius, Lithuania) and subsequently into pKA05 to generate the truncation constructs. The plasmid pKA484 was constructed by inserting a 2.2-kbp PstI-BamHI fragment (containing the open reading frame Orf19.3120) into the vector pRC2312. This construct was used for overexpression of Orf19.3120. The plasmids used in this study are listed in Table 2.
Chromosomal preparation, separation, and band analysis
In order to verify the karyotypes of the generated Candida strains, intact chromosomes were prepared as described previously [32]. Briefly, fresh C. albicans cells were grown in YPD liquid media to the cell density of 107 cells/mL and harvested by centrifugation. Cells were washed with 50 mM ethylenediaminetetraacetic acid (EDTA) pH 7.5 and resuspended at 1 × 109 cells/mL. For making the plugs, 200 μL cells, 20 μL zymolyase, and 250 μL of 1.2% low-melting agarose were mixed vigorously in a 1.5-mL tube and poured into the molds (Bio-Rad Laboratories, USA) as 100 μL aliquots/well and solidified at room temperature for 20 min. First incubation was at 37 °C for 18 h in solution containing 0.5 M EDTA (pH 9.0), 25 mM Tris-HCl (pH 8.0), and 4% β-mercaptoethanol, and the second incubation was at 55 °C in 0.5 M EDTA (pH 9.0), 25 mM Tris-HCl (pH 8.0), 1% N-lauroylsarcosine, and 0.01% proteinase K for 48 h.
The pulse-field gel electrophoresis system CHEF-DR II (Bio-Rad) was used in separating the chromosomes as described previously [32]. Agarose gels were stained using SYBR Green I nucleic acid gel stain (Sigma) for 30 min. The images of the gels were analyzed using Quantity One Software, and the intensity of the chromosome bands was analyzed by Image Lab Software Version 5.1 (Bio-Rad).
Minimum inhibitory concentration (MIC) assay
The MIC for the generated Candida strains was determined according to the protocol of the Clinical and Laboratory Standards Institute (CLSI) [37]. Briefly, fresh cells were collected from YPD plates and counted under a light microscope. Approximately 2 × 106 cells were mixed with 0.7% molten agar and poured onto Mueller-Hinton agar plates. The MIC strips were placed in the middle of the plate and incubated at 30 °C for 24 h. The images were captured using Quantity One Software. Ezy MICTM strips were used for three classes of antifungals: fluconazole (0.016–256 μg/mL), amphotericin B (0.002–32 μg/mL), and caspofungin (0.002–32 μg/mL) (Himedia, Mumbai, India).
Spot assay against fluconazole
For spot assay on fluconazole plate, young cells were collected from YPD plates streaked directly from − 80 °C. The cells were counted under a light microscope and spotted on synthetic dextrose (SD) plates containing fluconazole as 10-fold serial dilutions.
Microdilution assay against fluconazole
We carried out broth microdilution assay against fluconazole as described previously [37, 38]. The drug sensitivity test was carried out for the strains carrying truncations in one of the homologs of chromosome 4. Briefly, young cells were collected from the YPD plate, washed, and counted under a light microscope. Then, approximately 200 cells/well were inoculated into 96-well flat-bottomed microtiter plate. Subsequently, the antifungal drug fluconazole was added to the wells in increasing concentration from 0 to 128 μg/mL. The wells containing only media and media plus cells (without drug) were considered negative and positive controls. All the samples were plated in triplicate and incubated at 30 °C for 24 h, and optical densities (OD) were measured at 600 nm using a multi-detection microplate reader (Thermo Fisher Scientific, USA). Then, the graph of OD600 vs. fluconazole concentrations.
Disc diffusion assay
The disc diffusion test for Candida strains was carried out as described previously [39]. Discs containing fluconazole (25 μg), itraconazole (10 μg), ketoconazole (10 μg), clotrimazole (10 μg), miconazole (30 μg), amphotericin B (50 μg), and nystatin (50 μg) were used for disc diffusion assay (Himedia). Approximately 2 × 106 cells were mixed with 0.7% molten agar and poured onto Mueller-Hinton agar plates. The agar solidified for 15 min, and then the discs containing antifungals were placed in the middle of the plate. Next, we incubated the plates at 30 °C and measured the zone of inhibition at 24 h.
Results
Truncations of Chr4 in C. albicans
In order to elucidate the role of Chr 4 concerning drug resistance, we adopted a well-established telomere-mediated chromosomal truncation approach that analyzes L-sorbose utilization in this pathogen [24, 25]. To truncate Chr4, approximately 1 kbp PCR product (MS) was amplified from the intended truncation site using genomic DNA of parental strain CAF4-2, and then the truncation cassette was constructed. The exogenous construct consisted of three essential components: MS, selection marker (URA3), and Candida telomere (plasmid-borne telomere, PBT). After transformation into Candida strain, the truncation cassette replaces the entire portion of one homolog of Chr4 from the intended site to the telomere (Fig. 1). Furthermore, Chr4 is 1603 kbp long in which the centromere is located at 992–996.2 kbp position according to assembly 22 of the Candida Genome Database [36]. Since the left portion of Chr4 is longer (~ 992 kbp) than the right portion (~ 606 kbp), we performed the first truncation (truncation 1) at 969.925 kbp position (left side of the centromere) to remove approximately 970 kbp of the left portion as shown in Fig. 1a. The plasmid pKA52 was digested with KpnI-SacI to release the truncation cassette, which was transformed with the wild type strain CAF4-2. The ura+ transformants were screened by PCR using specific primers KC49/KC102 to identify the appropriate candidates for this truncation (Table 1, Supplementary Fig. 1B). Subsequently, we verified the truncated homolog of Chr4 by running a contour-clamped homogenous electric field (CHEF) program; nine positive candidates were obtained (Table 3). The chromosomal separation of one representative candidate of truncation 1 (969.925 kbp position) is shown in Fig. 2a. The size of the intact homolog of Chr4 is 1603 kbp, which is slightly above the 1532 kbp size marker of S. cerevisiae. However, the expected size of the truncated homolog of Chr4 was approximately 638 kbp (including URA3 flipper) and between 577 kbp and 784 kbp of S. cerevisiae markers (Fig. 2a). The PCR verification results for truncation 1 are shown in Fig. 2b. The primers KC49/KC102 could amplify the 1.5 kbp PCR product if truncation occurs at 969.925 kbp position (truncation1). The Candida strain carrying truncated Chr4 (truncation 1) showed a 1.5 kbp band on agarose gel electrophoreses, whereas wild type strain (no truncation) did not produce any PCR product (Fig. 2b).
Schematic diagram of chromosomal truncation. A Truncation on the left side of the centromere of chromosome 4. Two thick lines represent two homologs of Chr4 containing a centromere (C) in the middle and two telomeres at the ends (T). Truncation cassette has three essential components: PBT, plasmid-borne telomere sequence cloned in the same orientation as it is present in the cellular chromosome; MS, mapping sequence retrieved from the chromosomal sequence at which truncation is intended; and URA3, selection marker. B Truncation of Chr4 on the right-hand side of centromere. Truncation cassettes are made similarly to left portion truncation. However, the telomere sequence will face towards the right and will replace the cellular right portion telomere. Truncation on either side of the centromere generates a truncated homolog of Chr4 wherein the second homolog remains intact
Verification of truncation 1. A Karyotypic verification of truncation 1 (969.925 kb position) of chromosome 4 using contour-clamped homogenous electric field (CHEF). Sc, Saccharomyces cerevisiae chromosomes used as size marker, three relevant chromosome sizes are indicated by arrows at 1532 kb, 784 kb and 577 kb respectively; P, wild type strain CAF4-2; Trn.1, chromosomes of the strain carrying truncation 1. Arrows indicated for the intact homolog and truncated version of Chr4. Truncation at 969.925 kb position (~ 970 kb) generates a 633 kb long truncated version of Chr4. It runs between 784 kb and 577 kb marker chromosomes of S. cerevisiae. B PCR verification of truncation 1 with specific primers KC49/KC102. Lane M, 1 kb DNA ladder; lane P, PCR for wild type strain (no PCR product amplified); lane Trn.1, PCR for truncation junction producing 1.5 kb PCR product (expected size)
To determine whether the Candida strain carrying truncation 1 becomes resistant, we conducted the MIC test with three antifungal classes: fluconazole (azole), amphotericin B (polyene), and caspofungin (echinocandin). The MIC values for truncation 1 (at 969.925 kbp position) against fluconazole, amphotericin B, and caspofungin were 0.25, 1.0, and 0.125 μg/mL, respectively, whereas those for the wild type strain were 0.19, 0.75, and 0.064 μg/mL, respectively. These findings suggested that the strain carrying the truncated version of Chr4 (truncation 1) is sensitive to these antifungals, similar to that observed for the wild type strain (truncation 1 in Fig. 3, Supplementary Table S1).
Minimum inhibitory concentration (MIC) assay for strains carrying truncated Chr4. WT, wild type strain CAF4-2; Trn.1 to Trn.8, Candida strains carrying truncations 1–8. MIC strip test for the strains against A fluconazole in the range of 0.016–256 μg/ml; B amphotericin B in the range of 0.002–32 μg/ml; C caspofungin in the range of 0.002–32 μg/ml. Strains with truncated Chr4 showed MIC values similar to the wild type strain
As the removal of the left portion of Chr4 failed to produce any resistant phenotype, we carried out seven additional truncations (2–8) on the right portion of Chr4. These seven truncations were performed at 1002.852, 1102.087, 1201.989, 1301.783, 1369.883, 1529.969, and 1542.907 kbp positons on the right portion of Chr4 (Fig. 4). The karyotype of one representative candidate of truncation 5 (1301.783 kbp position) is shown in Fig. 5a. The truncated homolog of Chr4 (approximately 1305 kbp) runs just above Chr5 (size of Chr5 is 1191 kbp) and below the 1532 kbp size marker of S. cerevisiae; this truncation was further validated by PCR (Fig. 5b). Moreover, we attempted to truncate both left and right portions of Chr4 in the same strain to mimic Chr4 monosomy. However, we did not obtain any candidate after screening approximately 100 transformants. This failure could be attributed to two compelling reasons: First, the generation of monosomy of Chr4 may be a low-frequency event in C. albicans, and second, the deletion of both the left and right portions of Chr4 could be lethal due to the presence of recessive mutations or allelic differences.
The schematic diagram of eight truncations on chromosome 4 (1603 kb long). Truncation 1 at 969.925 kb position on the left side of the centromere. Truncations 2–8 at 1002.852 kb, 1102.087 kb, 1201.989 kb, 1301.783 kb, 1369.883 kb, 1529.969 kb, and 1542.907 kb positions on the right portion of Chr4. The centromere spanned at 992–996.2 kb position according to Candida Genome Database
Verification of truncation 5 on chromosome 4. A Karyotypic verification using CHEF. Sc, S. cerevisiae chromosomes size marker, three relevant chromosome sizes are indicated by arrows at 1532 kb, 1091 kb, and 924 kb respectively; P, wild type strain CAF4-2; Trn.5, chromosomes of the strain carrying truncation 5 at 1301.783 kb position on Chr4. The size of the truncated version of Chr4 (~ 1305 kb) is approximately 300 kb shorter than intact Chr4 and runs above Chr5 (Chr5 size---1191 kb). B PCR verification of truncation 5 with specific primers KC445/KC27. Lane M, 1 kb DNA ladder; lane P, PCR for wild type strain (no PCR product amplified); lane Trn.5, PCR for truncation junction producing 1.5 kb PCR product (expected size)
In summary, we performed eight systematic chromosomal truncations in one of the two homologs of Chr4 (Table 3). Truncations 1 and 2 removed the left and right portions of Chr4, respectively. Five truncations on the right portion of Chr4 (truncations 2–6) were performed at about 100 kbp from each other. On the other hand, the distance between truncations 7 and 8 was about 13 kbp from each other and was carried out to assess the role of the open reading frame (ORF) Orf19.3120 in drug resistance; it encodes a half-size PDR-subfamily ABC (ATP-binding cassette) transporter [36, 40].
Determination of MIC values for the generated strains
We determined the MIC values for all the eight Candida strains carrying a truncated version of one homolog of Chr4. These strains were tested using MIC strips for fluconazole, amphotericin B, and caspofungin (Fig. 3, Supplementary Table S1). The MIC values for fluconazole, amphotericin B, and caspofungin were as follows: 0.19–0.38 μg/mL (wild type 0.19 μg/mL), 0.75–1.0 μg/mL (wild type 0.75 μg/mL), and 0.064–0.25 μg/mL (wild type 0.064 μg/mL), respectively. These MIC values indicated that the strains bearing the truncated version of Chr4 are not drug-resistant.
Microdilution assay against fluconazole
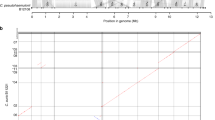
We carried out a microdilution assay against fluconazole for all the eight strains carrying truncations in one homolog of Chr4. The Candida strain CAF4-2 transformed with the integrative plasmid pRC3915 served as a control. Readings were recorded 24 h after inoculation, and graphs were plotted against fluconazole concentrations (Fig. 6). These results demonstrated that the generated strains remain sensitive to fluconazole.
Broth microdilution assay of the generated strains against fluconazole. WT, wild type strain CAF4-2; Trn.1 to Trn.8, Candida strains carrying truncations 1–8. Fluconazole concentrations from 0 to 128 μg/ml (0, 0.25, 0.5, 1, 2, 4, 8, 16, 32, 64, and 128 μg/ml) were used. All the strains are showing sensitivity to fluconazole, similar to the wild type strain
Spot assay against fluconazole
We spotted Candida strains carrying truncated homolog of Chr4 on SD plates containing various concentrations of fluconazole: 8, 16, 32, and 64 μg/mL (starting with 107 cells/mL). We considered high concentrations of fluconazole due to its fungistatic nature. The plates were incubated at 30 °C, and images were captured every 24 h for 3 days. The spotting assay of the generated strains on fluconazole showed distinct phenotypes when incubated for a prolonged period. The strain-sensitivity to fluconazole in 24 h was similar to that in the wild type strain; however, differential sensitivity towards fluconazole was detected in 48 h, which became prominent in 72 h (Fig. 7). The strain carrying truncation 5 was most sensitive among the strains. However, the strain carrying truncation 4 showed the least sensitivity to fluconazole, followed by truncation 8, while the other five stains did not differ markedly compared to the wild type strain. This analysis suggested that some truncated homologs of Chr4 were tolerant to fluconazole, although the MIC values were in the sensitive range.
Spot assay against fluconazole for the strains carrying truncated Chr4. WT, wild type strain CAF4-2; Trn.1 to Trn.8, Candida strains carrying truncations 1–8. Strains were 10-fold serially diluted (starting with 107/ml) and spotted on plate containing fluconazole A 8 μg/ml, B 16 μg/ml, C 32 μg/ml, and D 64 μg/ml where (i) control plate without fluconazole and photograph was taken after 24 h. For a plate containing fluconazole, we took photographs at 24 h (ii), 48 h (iii), and 72 h (iv) after spotting
Disc diffusion assay
We conducted a disc diffusion assay for eight strains against seven antifungals, including five azoles and two polyenes. All the strains showed sensitivity to these drugs, forming a clear zone of inhibition (Table 4, supplementary Fig. S2). However, the diameter of the zone of inhibition varied among the strains. The diameters of the zone of inhibition for the strains 32–39 mm against fluconazole (wild type, 37 mm), 23–32 mm against clotrimazole (wild type, 27 mm), 22–33 mm against itraconazole (wild type, 29 mm), 23–38 mm against ketoconazole (wild type, 34 mm), 25–41 mm against miconazole (wild type, 34 mm), 17–25 mm against amphotericin B (wild type, 24 mm), and 19–32 mm against nystatin (wild type, 30 mm). The variation in the drug sensitivity could be attributed to the strains’ genetic makeup as Chr4 was truncated at different sites removing large chromosomal segments of various sizes.
Overexpression of Orf19.3120
The overexpression of many genes renders the Candida strains resistant to multiple antifungals. Since ORF Orf19.3120 was predicted to encode a half-size PDR-subfamily ABC transporter [40], we overexpressed the molecule in the CAF4-2 Candida strain to test its response to fluconazole. Thus, we transformed CAF4-2 with the plasmid pKA484 (Orf19.3120 cloned in pRC2312). The transformants were detected on a fluconazole plate incubated at 30 °C for 2 days. Consequently, we found that the overexpression of Orf19.3120 does not render the strain resistant to fluconazole. However, it grew slightly more than the control strain, indicating a putative role in fluconazole resistance (Fig. 8).
Overexpression of Orf19.3120 and its response to fluconazole. Strains were 10-fold serially diluted and spotted on synthetic dextrose (SD), and synthetic dextrose plus fluconazole (8μg/ml) (SD+Flu) plates lacking uracil. The overexpressed strain grows a little better than the control strain in the presence of fluconazole
Discussion
In the history of C. albicans, the role of aneuploidy formation exhibited an efficient and effective means to generate critical genome modifications in response to environmental cues [41]. These changes are critical, such as altered chromosome copy number and translocation of a segment or truncation of a chromosome that exhibits multiple phenotypes, including drug resistance. In this study, we adopted a systematic chromosomal truncation approach to truncate Chr4 and assessed the strains for antifungals responses. The eight chromosomal truncations on one homolog of Chr4 generated Candida strains that were tested against antifungals. Either of the two homologs of Chr4 has the same probability of truncation as both are the same except for single nucleotide polymorphisms (SNPs) [42]. Truncation in one homolog generates monosomy of Chr4 with respect to the portion removed. For example, truncation at 969.925 kbp position on the left portion leaves only one left portion of the second homolog giving rise to the strain monosomy of Chr4 with respect to the left portion. The removal of the left portions of both homologs is not possible as there is one essential gene in approximately every 16 kbp of chromosomal stretch [36].
The generated Candida strains carrying the truncated homolog of Chr4 were assessed against multiple antifungals using different methods, such as determination of MIC, disc diffusion assay, microdilution assay, and spot assay. The MIC values obtained against fluconazole (azole), amphotericin B (polyene), and caspofungin (echinocandin) for these strains were similar to those for the wild type. These results suggested that strains carrying truncated Chr4 remain sensitive to these drugs. Furthermore, microdilution and disc diffusion assays were carried out for all eight strains to assess their responses to antifungals. The disc diffusion assay results showed slight variation in the responses to antifungals. Most of the generated strains showed slightly less sensitivity to the drugs compared to the wild type (Table 4). Interestingly, when strains were spotted on the plates containing increasingly higher concentrations of fluconazole, the Candida strain carrying truncation 4 (1201.989 kbp position on Chr4) showed better growth at fluconazole 8–64 μg/mL. However, the MIC value of this strain was the same as that of wild type (0.19 μg/mL for fluconazole). These findings indicated that the MIC values cannot predict the tolerance of a specific strain to antifungals. Previous observations revealed that antifungal tolerance operates at different pathways in this fungal pathogen. For example, the Rim pathway participates in antifungal tolerance through Hsp90p and Ipt1p [43]. However, tolerance to caspofungin can be mediated through the regulation of FSK gene expression and cell wall remodeling [44]. The antifungal tolerance could also be a subpopulation effect in which clinical isolates of C. albicans grow beyond the MIC. This extended growth is often associated with persistent candidemia [45]. Fluconazole is commonly used as the first-line drug for the treatment and management of Candida infections. Therefore, fluconazole tolerance can adversely affect the treatment of C. albicans bloodstream infections, and the patients could be at a high risk of morbidity and mortality [46].
Chr4 does not contain any drug resistance gene except the ORF Orf19.3120 (coordinates: 1538056–1539795 on Chr4), which encodes a half-size PDR-subfamily ABC transporter. To assess the role of Orf19.3120 in drug resistance, truncations 7 and 8 were performed on either side of this ORF at 1529.969 kbp and 1542.907 kb positions, respectively. The strain carrying truncation 8 grew slightly better than the strain carrying truncation 7 (Fig. 7). The overexpression of specific drug transporter genes, such as CDR1 and CDR2 produced a drug-resistant phenotype [47]. Hence, we overexpressed Orf19.3120 in Candida strain CAF4-2 and assessed its phenotype on the plate containing fluconazole.
Interestingly, the Candida strain with overexpressed Orf19.3120 showed an optimal growth in the presence of fluconazole (Fig. 8), thereby suggesting that Orf19.3120 may have a minor role in drug resistance. Conversely, the strain lacking this ORF was sensitive to fluconazole in the presence of silver nanoparticles [48].
Genomic plasticity is one of the major characteristics of C. albicans [49]. Rapid unusual genome changes in this pathogen might occur when mitotic cells are propagated in vitro as well as in vivo. Also, aneuploidy is detected in some pathogenic fungi. These phenomena suggested that variations in chromosome organization and copy number are common, rapid, and efficient means to generate diversity in response to stressful conditions, including the presence of drugs [49]. Moreover, Chr4 trisomy has been reported in a clinical isolate with a putative role in elevated fluconazole resistance. However, Chr4 trisomy failed to increase fluconazole resistance in the background of standard Candida strain SC5314 [50] used for sequencing the Candida genome. Furthermore, some clinical isolates harbor trisomy of Chr4 and Chr7 but their roles in drug resistance are not yet ascertained [51]. In addition, the presence of Chr4 monosomy in any clinical isolates of C. albicans and its association with drug resistance also has not been reported. Therefore, Chr4 monosomy or trisomy cannot be considered responsible for drug resistance. However, in specific genetic backgrounds with predisposing mutations or genomic changes, these conditions could be implicated in drug resistance.
Conclusion
In summary, we performed systematic chromosomal truncations of Chr4 of Candida albicans and assessed their responses to antifungals. The partial or segmental aneuploidies generated were challenged against three classes of antifungals, such as azoles, polyenes, and echinocandin. All the strains carrying truncated Chr4 were sensitive to these antifungals, similar to that for the wild type strain. However, some truncations exhibited a highly tolerant phenotype against fluconazole, a front-line antifungal drug. Drug tolerance was also observed when the strains were incubated in fluconazole for > 2 days. Therefore, C. albicans uses Chr4 as a drug-tolerant arsenal, which would benefit its propagation and colonization at different niches, posing a threat to candidiosis treatment and management. Finally, we concluded that it is unlikely that Chr4 is involved in drug resistance in this fungal pathogen. However, it may participate in developing resistance to antifungals in specific genetic backgrounds.
Nevertheless, truncations 4 and 8 would be explored in future studies to unveil the genes responsible for fluconazole tolerance. The strains will also be tested against other commonly used antifungals to deduce their efficacy with respect to these two truncations. In addition, we aim for truncations in the left portion of Chr4 to identify the chromosomal segments involved in drug resistance/tolerance. Further studies would be required to compare the genes’ expression in the strains carrying truncated Chr4, which would be valuable in understanding the Candida biology.
Availability of data and materials
The authors declare that all data are included in the article.
Abbreviations
- ABC:
-
ATP-binding cassette
- CGD:
-
Candida Genome Database
- CHEF:
-
Contour-clamped homogenous electric field
- Chr4:
-
Chromosome 4
- CLSI:
-
Clinical and Laboratory Standards Institute
- DMSO:
-
Dimethyl sulfoxide
- EDTA:
-
Ethylenediaminetetraacetic acid
- MFS:
-
Major facilitator superfamily
- MIC:
-
Minimum inhibitory concentration
- PCR:
-
Polymerase chain reaction
- PDR:
-
Pleiotropic drug resistance
- SD:
-
Synthetic dextrose
- WT:
-
Wild type
- YPD:
-
Yeast extract/peptone/dextrose
References
Sudbery PE (2011) Growth of Candida albicans hyphae. Nat Rev Microbiol 9(10):737–748. https://doi.org/10.1038/nrmicro2636
Su C, Yu J, Lu Y (2018) Hyphal development in Candida albicans from different cell states. Curr Genet 64(6):1239–1243. https://doi.org/10.1007/s00294-018-0845-5
Kabir MA, Hussain MA, Ahmad Z (2012) Candida albicans: A model organism for studying fungal pathogens. ISRN Microbiol 2012:538694–538615. https://doi.org/10.5402/2012/538694
Mayer FL, Wilson D, Hube B (2013) Candida albicans pathogenicity mechanisms. Virulence 4(2):119–128. https://doi.org/10.4161/viru.22913
Castanheira M, Deshpande LM, Davis AP, Rhomberg PR, Pfaller MA (2017) Monitoring antifungal resistance of CLSI epidemiological values and whole-genome sequencing analysis for detection of azole resistance. Antimicrob Agents Chemother 61(10):e00906–e00917. https://doi.org/10.1128/AAC.00906-17
Pappas PG, Lionakis MS, Arendrup MC, Ostrosky-Zeichner L, Kulberg BJ (2018) Invasive candidiasis. Nat Rev Dis Primers 4:18026. https://doi.org/10.1038/nrdp.2018.26
Cowen LE, Sanglard D, Howard SJ, Rogers PD, Perlin DS (2014) Mechanisms of antifungal drug resistance. Cold Spring Harb Perspect Med 5(7):a019752. https://doi.org/10.1101/cshperspect.a019752
Morschhäuser J (2016) The development of fluconazole resistance in Candida albicans - an example of microevolution of a fungal pathogen. J Microbiol 54(3):192–201. https://doi.org/10.1007/s12275-016-5628-4
Grela E, Zdybicka-Barabas A, Pawlikowska-Pawlega B, Cytrynska M, Wlodarczyk M, Grudzinski W, Luchowski R, Gruszecki WI (2019) Modes of the antibiotic activity of amphotericin B against Candida albicans. Sci Rep 9:17029. https://doi.org/10.1038/s41598-019-53517-3
Whaley SG, Berkow EL, Rybak JM, Nishimoto AT, Barker KS, Rogers PD (2017) Azole antifungal resistance in Candida albicans and emerging non-albicans Candida species. Front Microbiol 7:2173. https://doi.org/10.3389/fmicb.2016.02173
Pristov KE, Ghannoum MA (2019) Resistance of Candida to azoles and echinocandins worldwide. Clin Microbiol Infect 25(7):792–798. https://doi.org/10.1016/j.cmi.2019.03.028
Zarnowski R, Sanchez H, Covelli AS, Dominguez E, Jaromin A, Bernhardt J, Mitchell KF, Heiss C, Azadi P, Mitchell A, Andes DR (2018) Candida albicans biofilm-induced vesicles confer drug resistance through matrix biogenesis. PLoS Biol 16(10):e2006872. https://doi.org/10.1371/journal.pbio.2006872
Prasad R, Nair R, Banerjee A (2019) Emerging mechanism of drug resistance in Candida albicans. Prog Mol Subcell Biol 58:135–153. https://doi.org/10.1007/978-3-030-13035-0_6
Redhu AK, Shah AH, Prasad R (2016) MFS transporters of Candida species and their role in clinical drug resistance. FEMS Yeast Res 16:fow043. https://doi.org/10.1093/femsyr/fow043
Flowers SA, Colón B, Whaley SG, Schuler MA, Rogers PD (2015) Contribution of clinically derived mutations in ERG11 to azole resistance in Candida albicans. Antimicrob Agents Chemother 59(1):450–460. https://doi.org/10.1128/AAC.03470-14
Morio F, Pagniez F, Lacroix C, Miegeville M, Pape PL (2012) Amino acid substitutions in the Candida albicans sterol Δ5,6-desaturase (Erg3p) confer azole resistance: characterization of two novel mutants with impaired virulence. J Antimicrob Chemother 67(9):2131–2138. https://doi.org/10.1093/jac/dks186
Hope WW, Tabernero L, Denning DW, Anderson MJ (2004) Molecular mechanisms of primary resistance to flucytosine in Candida albicans. Antimicrob Agents Chemother 48(11):4377–4386. https://doi.org/10.1128/AAC.48.11.4377-4386.2004
Spettel K, Barousch W, Makristathis A (2019) Analysis of antifungal resistance genes in Candida albicans and Candida glabrata using next generation sequencing. PLoS One 14(1):e0210397. https://doi.org/10.1371/journal.pone.0210397
Ramírez-Zavala B, Manz H, Englert F, Rogers PD, Morschhäuser J (2018) A hyperactive form of the zinc cluster transcription factor Stb5 causes YOR1 overexpression and beauvericin resistance in Candida albicans. Antimicrob Agents Chemother 62(12):e01655–e01618. https://doi.org/10.1128/AAC.01655-18
Nishimoto AT, Zhang Q, Hazlett B, Morschhäuser J, Rogers PD (2019) Contribution of clinically derived mutations in the gene encoding the zinc cluster transcription factor Mrr2 to fluconazole antifungal resistance and CDR1 expression in Candida albicans. Antimicrob Agents Chemother 63(5):e00078–e00019. https://doi.org/10.1128/AAC.00078-19
Rustchenko EP, Howard DH, Sherman F (1994) Chromosomal alterations of Candida albicans are associated with the gain and loss of assimilating functions. J Bacteriol 176(11):3231–3241. https://doi.org/10.1128/jb.176.11.3231-3241.1994
Janbon G, Sherman F, Rustchenko E (1998) Monosomy of a specific chromosome determines L-sorbose utilization: a novel regulatory mechanism in Candida albicans. Proc Natl Acad Sci USA 95(9):5150–5155. https://doi.org/10.1073/pnas.95.9.5150
Perepnikhatka V, Fischer FJ, Niimi M, Baker RA, Cannon RD, Wang YK, Sherman F, Rustchenko E (1999) Specific chromosome alterations in fluconazole-resistant mutants of Candida albicans. J Bacteriol 181(13):4041–4049. https://doi.org/10.1128/JB.181.13.4041-4049.1999
Kabir MA, Ahmad A, Greenberg J, Wang YK, Rustchenko E (2005) Loss and gain of chromosome 5 controls growth of Candida albicans on sorbose due to dispersed redundant negative regulators. Proc Natl Acad Sci USA 102(34):12147–12152. https://doi.org/10.1073/pnas.0505625102
Reddy PK, Pullepu D, Dhabalia D, Udaya Prakash SM, Kabir MA (2020) CSU57 encodes a novel repressor of sorbose utilization in opportunistic human fungal pathogen Candida albican. Yeast 38:222–238
Fonzi WA, Irwin MY (1993) Isogenic strain construction and gene mapping in Candida albicans. Genetics 134(3):717–728. https://doi.org/10.1093/genetics/134.3.717
Gough JA, Murray NE (1983) Sequence diversity among related genes for recognition of specific targets in DNA molecules. J Mol Biol 166(1):1–19. https://doi.org/10.1016/S0022-2836(83)80047-3
Sherman F (2002) Getting started with the yeast. In: Guthrie C, Fink GR (eds) Methods in enzymology. Guide to yeast genetics and molecular biology, vol 350. Academic Press, New York, pp 3–41
Sambrook J, Russell DW (2001) Molecular cloning: A laboratory manual. Cold Spring Harbor Laboratory Press. Cold Spring Harbor, New York
Birnboim HC, Doly J (1979) A rapid alkaline extraction procedure for screening reombinant plasmid DNA. Nucleic Acids Res 7(6):1513–1523. https://doi.org/10.1093/nar/7.6.1513
Hinnen A, Hicks JB, Fink GR (1978) Transformation of yeast. Proc Natl Acad Sci USA 75(4):1929–1933. https://doi.org/10.1073/pnas.75.4.1929
Kabir MA, Rustchenko E (2005) Determination of gaps by contig alignment with telomere-mediated chromosomal fragmentation in Candida albicans. Gene 345(2):279–287. https://doi.org/10.1016/j.gene.2004.11.029
Morschhäuser J, Michel S, Staib P (1999) Sequential gene disruption in Candida albicans by FLP-mediated site-specific recombination. Mol Microbiol 32(3):547–556. https://doi.org/10.1046/j.1365-2958.1999.01393.x
McEachern MJ, Hicks JB (1993) Unusually large telomeric repeats in the yeast Candida albicans. Mol Cell Biol 13(1):551–560. https://doi.org/10.1128/mcb.13.1.551-560.1993
Cannon RD, Jenkinson HF, Shepherd MG (1992) Cloning and expression of Candida albicans ADE2 and proteinase genes on a replicative plasmid in C. albicans and Saccharomyces cerevisiae. Mol Gen Genet 235(2-3):453–457. https://doi.org/10.1007/BF00279393
Skrzypek MS, Binkley J, Binkley G, Miyasato SR, Simison M, Sherlock G (2017) The Candida Genome Database (CGD): incorporation of Assembly 22, systematic identifiers and visualization of high throughput sequencing data. Nucleic Acids Res 45(D1):D592–D596. https://doi.org/10.1093/nar/gkw924
Clinical and Laboratory Standards Institute (2018) Performance standards for antifungal susceptibility testing of yeasts, 3rd edn. CSLI supplement M60, Wayne
Ostrosky-Zeichner L, Rex JH, Pfaller MA, Diekema DJ, Alexander BD, Andes D, Brown SD, Chaturvedi V, Ghannoum MA, Knapp CC, Sheehan DJ, Walsh TJ (2008) Rationale for reading fluconazole MICs at 24 hours rather than 48 hours when testing Candida spp. by the CLSI M27-A2 standard method. Antimicrob Agents Chemother 52(11):4175–4177. https://doi.org/10.1128/AAC.00420-08
Clinical and Laboratory Standards Institute (2018) Method for antifungal disk diffusion susceptibility testing of yeasts, 3rd edn. CSLI guideline M44, Wayne
Gaur M, Choudhury D, Prasad R (2005) Complete inventory of ABC proteins in human pathogenic yeast, Candida albicans. J Mol Microbiol Biotechnol 9(1):3–15. https://doi.org/10.1159/000088141
Berman J (2016) Ploidy plasticity: A rapid and reversible strategy for adaptation to stress. FEMS Yeast Res 16(3):fow020. https://doi.org/10.1093/femsyr/fow020
Abbey D, Hickman M, Gresham D, Berman J (2011) High-resolution SNP/CGH microarrays reveal the accumulation of loss of heterozygosity in commonly used Candida albicans strains. G3 1:523–530
Garnaud C, García-Oliver E, Wang Y, Maubon D, Bailly S, Despinasse Q, Champleboux M, Govin J, Cornet M (2018) The Rim pathway mediates antifungal tolerance in Candida albicans through newly identified Rim101 transcriptional targets, including Hsp90 and Ipt1. Antimicrob Agents Chemother 62(3):e01785–e01717. https://doi.org/10.1128/AAC.01785-17
Yang F, Zhang L, Wakabayashi H, Myers J, Jiang Y, Cao Y, Jimenez-Ortigosa C, Perlin DS, Rustchenko E (2017) Tolerance to caspofungin in Candida albicans is associated with at least three distinctive mechanisms that govern expression of FKS genes and cell wall remodeling. Antimicrob Agents Chemother 61(5):e00071–e00017. https://doi.org/10.1128/AAC.00071-17
Rosenberg A, Ene IV, Bibi M, Zakin S, Segal ES, Ziv N, Dahan AM, Colombo AL, Bennett RJ, Berman J (2018) Antifungal tolerance is a subpopulation effect distinct from resistance and is associated with persistent candidemia. Nat Commun 9(1):2470. https://doi.org/10.1038/s41467-018-04926-x
Levinson T, Dahan A, Novikov A, Paran Y, Berman J, Ben-Ami R (2021) Impact of tolerance to fluconazole on treatment response in Candida albicans bloodstream infection. Mycoses 64(1):78–85. https://doi.org/10.1111/myc.13191
Prasad R, Balzi E, Banerjee A, Khandelwal NK (2019) All about CDR transporters: Past, present, and future. Yeast 36(4):223–233. https://doi.org/10.1002/yea.3356
Dhabalia D, Ukkund SJ, Syed ST, Uddin W, Kabir MA (2020) Antifungal activity of biosynthesized silver nanoparticles from Candida albicans on the strain lacking the CNP41 gene. Mater Res Express 7(12):125401. https://doi.org/10.1088/2053-1591/abcc83
Selmecki A, Forche A, Berman J (2010) Genomic plasticity of the human fungal pathogen Candida albicans. Eukaryot Cell 9(7):991–1008. https://doi.org/10.1128/EC.00060-10
Anderson MZ, Saha A, Haseeb A, Bennett RJ (2017) A chromosome 4 trisomy contributes to increased fluconazole resistance in a clinical isolate of Candida albicans. Microbiology (Reading) 163(6):856–865. https://doi.org/10.1099/mic.0.000478
Hirakawa MP, Martinez DA, Sakthikumar S, Anderson MZ, Berlin A, Gujja S, Zeng Q, Zisson E, Wang JM, Greenberg JM, Berman J, Bennett RJ, Cuomo CA (2015) Genetic and phenotypic intra-species variation in Candida albicans. Genome Res 25(3):413–425. https://doi.org/10.1101/gr.174623.114
Acknowledgements
We are thankful to Joachim Morschhäuser, Würzburg, Germany, for the plasmid pSFU1. We thank Richard Cannon, University of Otago, New Zealand, for plasmid pRC2312 and pRC3915. We thank Michael McEachern for the plasmid “BSA” containing C. albicans telomere. Seed money provided by National Institute of Technology Calicut was used to carry out this work.
Funding
Seed money for research provided by National Institute of Technology Calicut was used to carry out this work.
Author information
Authors and Affiliations
Contributions
All the four authors participated in this study. MAK conceived the idea. WU, DD, and SMUP did the experiments. WU, DD, SMUP, and MAK analyzed the data. WU wrote the manuscript. DD and SMUP made substantial corrections. MAK revised and corrected the manuscript. The authors have read and approved the final manuscript.
Authors’ information
All the authors are from the same laboratory. The address is as follows: Molecular Genetics Laboratory, School of Biotechnology, National Institute of Technology Calicut, Calicut-673601, Kerala, India.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Authors give the consent for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table S1.
Minimum inhibitory concentration (MIC) for the strains carrying truncated chromosome 4. Supplementary Fig. S1. (A) Schematic diagram of plasmid pKA05 [25]. This plasmid was used as a backbone plasmid for generating truncation constructs. Mapping sequences (MS) from truncation sites of chromosome 4 were inserted at K-Xh (KpnI-XhoI) and the resulting plasmids were digested with KpnI-SacI and transformed into Candida. (B) Schematic diagram of PCR verification for chromosomal truncation. Primers P1 and P2 were designed from upstream of MS of chromosome 4 and URA3 flipper, respectively. The primers amplify PCR product of expected size only when truncation occurs at the intended site on Chr4. PBT, plasmid-borne Candida telomere. Supplementary Fig. S2. Disc diffusion assay for strains carrying truncated homologue of Chromosome 4. WT, wild type strain CAF4-2; Trn1 to Trn8, strains carrying truncations at 969.905 kb, 1002.852 kb; 1102.087 kb; 1201.989 kb; 1301.783 kb; 1369.883 kb; 1529.969 kb; 1542.907 kb positions on Chr4. Cells were poured along with molten 0.7% agar and disc containing (A) fluconazole (25 μg); (B) clotrimazole (10 μg); (C) itraconazole (10 μg); (D) ketokonazole (10 μg); (E) miconazole (30 μg); (F) amphotericin B (50 μg); (G) nystatin (50 μg) were placed on the plate (Himedia, Mumbai, India). Photographs were taken after 24 hr.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Uddin, W., Dhabalia, D., Prakash, S.M.U. et al. Systematic truncations of chromosome 4 and their responses to antifungals in Candida albicans. J Genet Eng Biotechnol 19, 92 (2021). https://doi.org/10.1186/s43141-021-00197-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43141-021-00197-0