Abstract
Background
Gallstone disease with its consequences is a common clinical issue that may necessitate surgical removal. In comparison with traditional open procedures, laparoscopic cholecystectomy (LC) remains the mainstay treatment for symptomatic gallstone disease and can lead to a shorter recovery period, and a shorter hospital stay; yet, severe abdominal and shoulder pain may be experienced.
Main body
Novel drugs and technology for acute and chronic pain management following LC have been studied to improve patient care. The review discusses innovative pain management strategies with non-opioid approaches for laparoscopic surgery, with an emphasis on ensuring speedy and safe recovery.
Conclusion
The key findings state that IV paracetamol is a necessary part of multimodal postoperative pain management. There were several pharmacological interventions found to be effective in pain control: magnesium sulfate and dexamethasone showed anti-inflammatory benefits; ondansetron provided analgesic effects; gabapentinoids and alpha-2-agonists reduced central sensitization; local anesthetics offered targeted pain relief; antidepressants addressed neuropathic pain; NSAIDs proved effective for inflammatory pain. Similarly, non-pharmacological approaches, and emerging technologies, also contributed to the management of post-LC pain underscoring the need for a comprehensive approach to its management. More rigorous research is needed to guide pain management after LC. Future studies should compare multiple treatments simultaneously and involve larger patient groups. This approach will help identify optimal pain control strategies. It will also provide clearer insights into the safety and efficacy of various pain medications under comparable clinical conditions.
Similar content being viewed by others
Background
Gallstones are solid bile deposits that can occur in the gallbladder caused by various factors such as hormones, dietary changes, drugs, and rapid weight loss or obesity. These gallstones can cause gallbladder inflammation and infection by impeding normal bile flow. This is known as cholecystitis, and it can produce severe, continuous abdominal pain, fever, nausea, and vomiting [1]. Regretfully, opinions differ about the best management approach for this condition. The sole novel route to the bile duct for a long time was a direct open surgical technique. Advanced endoscopic technology has made minimally invasive procedures possible [2]. An open cholecystectomy involves a 10–15 cm incision in the upper right quadrant of the abdomen. The surgeon removes the gallbladder through an incision. In contrast, the laparoscopic cholecystectomy (LC) operation requires only 3–4 extremely tiny incisions. This procedure makes use of a long, thin tube known as a laparoscope by introducing it through the incisions. One incision is made to remove the gallbladder [3].
LC is the current gold standard and less invasive therapy causing less postoperative pain, but it might be mild, moderate, or severe in certain people [4, 5]. Moreover, it results in reduced analgesic intake, reduced recovery time, and shorter hospital stays than open cholecystectomy [6, 7]. Visceral and shoulder pain are the most common types of pain experienced during LC. These pains are caused by diaphragmatic and peritoneal stretching, peritoneal irritation by CO2, changes in intra-abdominal pH, and the release of inflammatory mediators [8]. Inadequate care of acute pain within the first 48 h following surgery increases the likelihood of chronic pain development; therefore, postoperative pain management is crucial [9, 10] with the use of both non-opioid and opioid treatments. During the immediate postoperative phase, opioid medication can cause a variety of adverse effects, including respiratory depression, pruritus, nausea, and vomiting. Due to the significant adverse effects of opioids, the non-opioid medication in conjunction with a multimodal regimen is strongly suggested due to the latter regimen's fewer adverse effects [11, 12]. It is therefore crucial to identify the different non-opioid modalities in the management of postoperative LC pain. This current review aims to comprehensively evaluate the current evidence on non-opioid strategies as well as assess the efficacy of various pharmacological and non-pharmacological non-opioid interventions for pain control after LC.
Methods
Randomized controlled trials that were published in English between 2005 and 2024 were obtained from multiple databases, such as PubMed, Web of Science, Science Direct, Scopus, EMBASE, Medline, and Cochrane Library. The trials evaluated non-opioid postoperative pain management after laparoscopic cholecystectomy and reported pain scores. The various components of the gathered data were categorized based on the medication classifications. The terms "Laparoscopic cholecystectomy," "postoperative pain," "non-opioid strategies," "pain management," "gallbladder," "minimally invasive surgery," and "analgesia" are used to get the relevant articles.
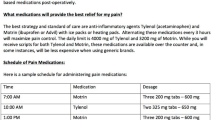
The retrieved studies were initially screened based on titles and abstracts to exclude irrelevant papers. Full texts of potentially eligible studies were then thoroughly reviewed to ensure they met the inclusion criteria. Studies were excluded if they focused solely on opioid interventions, did not report pain scores, or were not randomized controlled trials. The included studies were categorized based on the pharmacological class of the non-opioid interventions investigated. This categorization allowed for a systematic analysis of different types of non-opioid strategies. For each category, key information, including dosage, administration route, intervention timing, pain scores, and secondary outcomes, was extracted and summarized. The results of this analysis are presented in Table 1, which provides a comprehensive overview of the available evidence on non-opioid postoperative pain management strategies following LC.
Main text
Local anesthetics
Transversus abdominis plane block
The transversus abdominis plane (TAP) block enhances postoperative analgesia following abdominal surgery. A long-acting anesthetic is injected into the anterior abdominal wall's neurovascular plane to perform this procedure. This plane runs between the layers of the internal oblique and transversus abdominis muscles and passes the intercostal nerves from their spinal origins across the abdominal wall [88, 89]. This procedure can be done laparoscopically, under ultrasound (US) guidance, or utilizing a surface landmark-based method [3]. Overall, the data are positive, with the majority of studies showing clinically significant decreases in pain and postoperative opioid consumption. While it has been demonstrated that laparoscopic cholecystectomy (LC) patients can benefit from various TAP procedures, including US-guided TAP block and additional strategies, TAP blocking procedures are the most successful means of providing analgesia compared to general anesthesia and port infiltration. However, as US technology develops, TAP blockades are becoming more practicable and technically easier to execute. This has raised interest in TAP blocks as a therapeutic technique for analgesia following abdominal surgery [90]. Reducing opioid use with intraoperative laparoscopic transversus abdominis plane block (LC + TAP) is a safe and successful strategy, according to research that compared patients who underwent LC alone with patients who underwent a laparoscopic bilateral TAP block (LC + TAP) [17]. Accordingly, a randomized triple-blind study [52] compared the effectiveness of a laparoscopic TAP block versus port site local anesthetic infiltration in 100 patients having a LC. When comparing the TAP block group to the port site local anesthetic infiltration group, the median visual analogue scale (VAS) at 3, 6, 24 h, at discharge, and one week after surgery was significantly lower reflecting lower pain (p ≤ 0.001 for each), and the median Capuzzo score, which gauges patient satisfaction with analgesia, was significantly much greater (p < 0.001). Although it was not statistically significant (p = 0.48), the TAP block group's median duration for hospital stay was also shorter. In addition, the laparoscopic-guided TAP block is considered a cost-effective method based on the findings of a recent trial [91]. Further study demonstrated that the four-quadrant bilateral laparoscopic-guided transversus abdominis plane block was significantly lower than that of the unilateral transversus abdominis plane block (p = 0.0245) and the standard analgesic block (p = 0.002), concluding that the early postoperative pain following LC can be effectively avoided with bilateral TAP block. The TAP block should be delivered to all four quadrants [19].
Adjuvants can be added to the local anesthetic agent in US-guided TAP block applications to improve its analgesic efficacy and lessen the possibility of toxic side effects. Accordingly, a randomized trial was conducted to compare the intraoperative and postoperative impact of dexmedetomidine versus tramadol as adjuvants to bupivacaine in a TAP block in which 64 patients were equally distributed to either the TAP block group (bupivacaine + tramadol as an adjuvant) or dexmedetomidine group (bupivacaine + dexmedetomidine as an adjuvant). It is concluded there is no significant difference (p > 0.05) and superiority between the two groups over each other in the postoperative analgesia at (0, 3, 6 h), amount of analgesic required, mobilization times, and profile of side effects. However, the adjuvant dexmedetomidine in the TAP block preoperatively resulted in more stable intraoperative hemodynamic outcomes [18]. Nevertheless, another research [40] hypothesized the TAP block impact on postoperative pain and stress markers by comparing US-guided unilateral TAP block plus general anesthesia with general anesthesia alone revealing a significant reduction in pain at (6 and 12 h). Moreover, the TAP block group showed a significant reduction in the mean opioid use and stress response markers. Significant reduction of postoperative nausea and vomiting (PONV) and recovery period resulting in reduced hospital stay and intensive care unit (ICU) need in TAP block application have been demonstrated by a retrospective study conducted on 515 patients [53].
Based on the findings of trials reviewed in this study, the TAP block seems to have the potential to develop into a novel and significant intervention in the therapy of postoperative pain.
Bupivacaine
Bupivacaine is a safe and effective way to provide postoperative analgesia following laparoscopic cholecystectomy [92]. Bupivacaine is the most used local anesthetic following LC that decreases pain conduction by binding to voltage-gated sodium channels and preventing sodium entrance into cells [93]. A recent trial assessed the effectiveness of intraperitoneal (IP) diluted versus non-diluted bupivacaine group (NBG) for pain relief following LC. During the initial 24 h following surgery, the diluted bupivacaine group (DBG) had considerably lower postoperative VAS values than the NBG with a p value ≤ 0.003. In DBG, the time needed for the first analgesic demand was significantly higher than in the NBG (p value = 0.0001) over 24 h, suggesting that DBG had superior and longer-lasting postoperative analgesia. With (p value = 0.0001), the total opioid analgesics over 24 h were significantly less in DBG than in NBG. Regarding side effects following LC, there was no statistically significant difference (p value ˃ 0.05) in the incidence of PONV and shoulder pain between the two groups. Moreover, none of the research subjects in either group suffered from bradycardia, respiratory depression, or hypotension due to the local anesthetic injection [13]. Three groups, each with 60 patients, were compared in a randomized trial resulting in a significant reduction in VAS score in patients who received intravenous (I.V) parecoxib and subcutaneous (S.C) bupivacaine in contrast to placebo at 1, 2, and 4 h after the procedure. However, no significance was reported at 8, 12, and 24 h. In addition, the shoulder pain was lower in the bupivacaine group than in the other groups and the amount of rescue analgesics needed was reduced by the bupivacaine and parecoxib groups [75]. A study by Nikoubakht et al. [31] found no significant difference in the mean Ramsay score between the groups throughout the recovery, 2-, 8-, and 24-h postoperative timeframes. There was no significant difference between the groups when postoperative analgesic satisfaction scores were compared at 2 and 24 h after recovery. It indicated that using intraperitoneal (IP) bupivacaine and intra-abdominal bicarbonate reduced pain; with bupivacaine being more superior. A total of 90 patients were randomly assigned and compared (I.P bupivacaine to I.V ketorolac and the placebo group). Compared to the placebo group, the I.P bupivacaine and the I.V ketorolac significantly reduced the incidence of PONV, and postoperative stomach, and shoulder pain. While there was no statistically significant difference in analgesia between bupivacaine and ketorolac, both groups reported considerably higher levels of satisfaction. Furthermore, the need for opioid analgesics was significantly higher in the placebo group at 6 h and 12 h after the surgery [4]. Moreover, patients who received IP bupivacaine experienced a prolonged period of requesting rescue analgesia, which resulted in a substantial reduction in postoperative pain within the initial 6 h following surgery. In contrast to shoulder pain, which was significantly less in the bupivacaine group with p value = 0.04, side effects such as nausea and vomiting were equal in both groups [47]. Despite, many studies of high caliber proving the role of bupivacaine in post-LC pain management, a study was conducted to evaluate the efficacy of bupivacaine for shoulder and abdominal pain management after LC demonstrated no specific benefit for using bupivacaine as it did not affect pain compared to normal saline [32]. These variable results may be due to population variation and the fact that the majority of patients who undergo LC experience minor pain; hence, a large sample size must be studied as many patients must have a satisfactory outcome to show a discernible and substantial difference between the two groups. Additional studies are required to ascertain the effectiveness of IP bupivacaine in reducing pain during LC.
Lidocaine
The local anesthetic lidocaine is an amino amide that works by blocking sodium channels to lessen neural transmission. When given as a systemic infusion, it also lowers the chance of ileus. Local anesthetics have anti-inflammatory qualities, prevent the central nervous system from receiving nociceptive input, and are frequently highly beneficial in treating neuropathic pain.
Additionally, with lesser doses of local anesthetic, selective sympathetic blocking may be extremely helpful for visceral pain [1]. Intravenous lidocaine has analgesic and anti-inflammatory effects. Intravenous lidocaine infusion during the perioperative period is safe and has several benefits, including reduced anesthesia, postoperative analgesia, quicker bowel function recovery, and shorter hospital stays [94, 95]. Additionally, lidocaine comes in patches for use as a topical painkiller. It functions by inhibiting peripheral nociceptors' ability to sense pain. It has minimal systemic absorption and minimal adverse effects [96]. In a recent randomized controlled trial (RCT), patch group compared to the control group, the total incidence of shoulder pain was significantly reduced (p = 0.005). At 24 h and 48 h following surgery, the patch group's shoulder pain severity was significantly lower than that of the control group (p = 0.01, p = 0.015 respectively). The only side effect associated with the lidocaine patch was nausea. It concluded that the incidence and intensity of LC postoperative shoulder pain were reduced with a 5% lidocaine patch with no complication [48]. Comparing the effectiveness of lidocaine spray with subcutaneous injection at the port site in terms of improved pain management and fewer long-lasting adverse effects is observed. The pain level was comparable across the groups at any of the six points in time measured, ranging from right after waking up from anesthesia to 24 h following the procedure (p value = 0.329). The instillation lidocaine spray group's consumption of narcotics and nonsteroidal anti-inflammatory drugs (NSAIDs) was statistically reduced (p values = 0.003 and 0.013, respectively). The duration of hospital stay, the time needed to resume regular bowel movements and oral food, and the amount of nausea or vomiting that occurred after surgery did not, however, differ significantly across the groups; this suggests that it may be a valuable choice for managing pain after LC, since it may suggest improved pain control [41]. To evaluate the impact of IV lidocaine infusion on postoperative recovery, a study conducted by Song et al. [66] demonstrated that lidocaine had a significant effect (p = 0.01) on pain intensity as measured by VAS at 2 and 6 h. Additionally, a significantly reduced (p = 0.005) total opioid intake (98.27 ± 16.33 mg vs. 187.49 ± 19.76 mg) was recorded. Fewer cytokines were released during IV lidocaine infusion compared to the control group, providing evidence that, after LC, perioperative IV lidocaine enhances surgical recovery and delays the onset of an exaggerated inflammation. A head-to-head comparison of IP versus IV lidocaine reported a noteworthy decline in the IP and IV lidocaine groups' scores for patient-controlled analgesia (PCA), satisfaction with pain, overall opioid use, and as compared to the control group. The IP group experienced significantly lower pain than the IV group at 2 h after surgery, and the IP group received PCA less frequently at 0–2 h. IV lidocaine infusion is a more practical approach that is easier to implement and has a better safety profile than IP, regardless of IP's effectiveness. It was concluded that IV lidocaine treatment is a feasible substitute for IP lidocaine administration while attempting to reduce postoperative pain in patients undergoing LC [77]. On the contrary, another study [79] concluded that IP lidocaine is ineffective in reducing post-LC pain. Nevertheless, when assessing the impact of IV lidocaine infusion at a rate of 1.25 mg/kgBW per hour on the severity of pain it was indicated that the lidocaine group showed lower numeric rating scale (NRS) scores at 2 and 6 h than the placebo group but no differences, at 12 and 24 h postoperatively. The lidocaine group had a reduced postoperative opioid requirement than the placebo group, with a p value of 0.000, concluding the hastened healing of the intestines and the analgesic effect of perioperative lidocaine infusion [61]. A randomized study compared the effects of two different IV lidocaine infusion doses: 1.5 mg/kg for bolus lidocaine administered intravenously, followed by a continuous infusion of 1.5 mg/kg/h; and 1.5 mg/kg for bolus lidocaine administered intravenously, followed by a continuous infusion of 2 mg/kg/h. It proved that patients in both groups often had mean VAS scores of less than three following surgery, suggesting that sufficient analgesia was found to be provided by both doses. However, compared to 1.5 mg/kg/h, the dose of 2 mg/kg/h was found to be superior in terms of analgesia, as evidenced by significantly lower VAS scores at all-time intervals; an increased mean time of 49.42 min for the first rescue analgesic request in comparison with 30.65 min; and a decline in the total amount of analgesics consumed in 24 h to patients receiving the maintenance dose of 2 mg/kg/h, with a mean of 178.85 mg against 126.92 mg. Furthermore, the investigation showed no appreciable detrimental effects and concluded that the dosages were safe [26]. For comparison purposes, we also analyzed contrast data obtained from a blind study that compared the effect of IV bolus lidocaine, followed by a continuous infusion of 2 mg/kg/h to an equivalent placebo; that did not successfully verify a reduction in opioid demand 24 h after surgery (p = 0.542). The incidence of shoulder pain or postoperative pain scores were unaffected by lidocaine administration at any time point. Additionally, no differences were found in the incidence of nausea and postoperative sedation perhaps due to the failure to reduce the opioid consumption [27].
Antidepressants
Duloxetine
Duloxetine is a non-opioid neuromodulator with peripheral and central analgesic effects [97]. It possesses its action through selective inhibition of serotonin and norepinephrine reuptake. It is generally used as an anti-depressant and for the treatment of anxiety disorder, chronic musculoskeletal pain, fibromyalgia, and neuropathic pain [98, 99]. As part of multimodal analgesic regimes, duloxetine has also been linked to decreased consumption of postoperative opioids, a longer time until the first rescue analgesic is needed, and decreased chronic postoperative pain incidence [97]. The efficacy of preoperative duloxetine in controlling pain has been assessed in a variety of surgical procedures and found it had a lower incidence of drug-related cognitive adverse effects and a comparable analgesic impact for pain treatment following spinal surgery, it can be administered in place of pregabalin [100]. It has also been shown from a prior trial that it can lessen the need for morphine during the first 48 h following knee replacement surgery [101]. Preoperative duloxetine was helpful in seven randomized controlled studies for various procedures. The aggregated data showed that duloxetine significantly reduced pain scores at 4 (p < 0.001) and 24 h (p = 0.005) when compared to the placebo [102]. According to new research from a RCT, the area under the curve (AUC) of the VAS scores derived for the duloxetine group was significantly lower than those of the control group. The mean postoperative VAS scores showed a statistically significant difference, with the duloxetine group's values being statistically considerably lower at 4 and 24 h. In comparing the two groups' initial requests for rescue medication, there was no statistically significant difference (p = 0.665). Patients in the duloxetine group had a smaller total PONV, although it was not statistically significant (p = 0.734 and p = 0.572) compared to patients in the control group at 8- and 24-h intervals [33].
Gabapentinoids
Pregabalin and gabapentin belong to the gabapentinoid group of drugs that reduce postoperative pain via binding to the α-2-δ subunit of voltage-gated calcium channels and so inhibiting the release of excitatory neurotransmitters substance P, serotonin, and glutamate [103, 104]. Gabapentinoids are safe and effective at low dosages for treating pain following a variety of surgical procedures, including LC, despite having minimal risk effects of somnolence, vertigo, and vomiting. Other benefits of gabapentinoids include opioid sparing, preoperative anxiolysis, and a reduction in movement-evoked pain [36, 105]. According to research comparing the effectiveness of gabapentin and memantine as premedication, a lower NRS score was observed in the gabapentin group at 15 min and 1 h after surgery. In contrast, the memantine group requested rescue analgesia 50.53 min later than the gabapentin and placebo groups. Analgesiometer data used for objective pain assessment revealed no statistically significant differences in threshold or tolerance values between the three groups. However, acute postoperative pain is likely best evaluated and treated by subjective means; using an analgesiometer to quantify the general pain threshold may not be helpful in this regard. In contrast to the other two groups, the gabapentin group had higher Ramsay sedation scores. In summary, gabapentin, when given as a single preoperative dosage, provides superior adjuvant analgesia than memantine for patients undergoing laparoscopic cholecystectomy [46]. Also, Jain et al. [45] studied the effect of 1200 mg oral gabapentin given 2 h before the LC on the hemodynamic parameters and postoperative pain level, and observed that the gabapentin group had a significantly decreased VAS score and experienced a significantly longer duration of analgesia, nausea, and vomiting-free period (p < 0.01)[45]. Additionally, in comparison with hydrocortisone, it was demonstrated that the gabapentin group's mean VAS score was significantly lower in the first 2, 4, and 24 h following surgery with no differences at 6 h, 12 h, and 18 h [59].
However, pregabalin was shown to have anti-epileptic, analgesic, and anxiolytic effects that were comparable to those of gabapentin in earlier research, but it also had a more favorable pharmacokinetic profile [106]. After an oral intake, it is quickly absorbed, reaching its maximum plasma concentration an hour after one or more doses with 90% oral bioavailability that is dose-independent. In comparison with gabapentin, these properties provide an advantage for perioperative use [107]. In a prior trial, pregabalin used preoperatively has been shown to significantly lower the pain score and total opioid consumption [36, 105, 108]. When comparing the effectiveness of pregabalin and tizanidine, patients in the placebo group requested more analgesia than those in the tizanidine and pregabalin groups (p = 0.03), but no statistical differences were found between both interventions (p = 0.84). The findings suggest that the single or combination use of these medications may be useful in lowering or managing LC postoperative pain in conjunction with common postoperative analgesics, such as opioids and NSAIDs; additionally, lowering the dosage of these medications is linked to fewer side effects and improved quality of life [29]. Preemptive pregabalin was found to exhibit a highly significant difference in pain scoring across all-time records in a prior trial, with a p value of less than 0.0001. Those in the placebo group experienced serious pain compared to mild pain experienced in the intervention group, with no adverse effects in either group [36]. Singh et al. [54] discovered that in comparison with 150 mg and 300 mg pregabalin, the control group's overall mean VAS score was significantly higher. The mean VAS values among the pregabalin-treated groups were higher for 150 mg pregabalin than for 300 mg pregabalin; however, this difference was not statistically significant. However, a pregabalin dose of 300 mg is linked to a higher frequency of side effects, including sedation, vertigo, and visual problems. For individuals having a LC, 150 mg of pregabalin is therefore a safe and ideal dosage for reducing postoperative pain with the least amount of adverse effects. On the other hand, a study by Von Plato et al. [60] discovered that 150 mg of pregabalin administered as additive analgesia before surgery failed to reduce post-surgery abdominal pain or opioid intake in the initial hour following surgery in patients who had high risk for postsurgical pain. A significant positive association (p = 0.045) was seen between preoperative stress, as evaluated on a 0–10 scale, and postsurgical pain.
Kaur et al. studied the preemptive pain-relieving effects of gabapentin and pregabalin, and demonstrated that when both were compared to a placebo, the VAS scores were significantly decreased. However, both drugs had similar scores. When gabapentin and pregabalin were used instead of a placebo, there was a statistically significant variance (p value < 0.001) in the meantime of rescue analgesia. As a result, gabapentin and pregabalin offer longer postoperative analgesia. Furthermore, the intervention groups consumed a significantly reduced mean dose of opioids over 24 h than in the placebo group. Nonetheless, there was no significant variation in the overall amount of opioids consumed by both drugs. However, they cause a greater degree of drowsiness than a placebo up to 6 h after surgery [28]. Other studies found that both gabapentin and pregabalin are important for postoperative analgesia when compared to placebo; nonetheless, pregabalin was considered more effective for postoperative analgesia because the pregabalin group used fewer opioids, had a lower VAS score, and delayed 1st rescue analgesic demand than the gabapentin group [68, 73].
Paracetamol
Paracetamol shares analgesic and antipyretic properties but the consensus is that it has little to no anti-inflammatory properties. Its outstanding safety record contributes to its status as one of the most widely used medications in the world. As a metabolite of phenacetin, paracetamol increases the threshold for pain by blocking cyclooxygenase in the central nervous system, but not in peripheral tissue. As a result, it has no anti-inflammatory effects. For the short-term treatment of mild pain, especially following surgery, and fever, IV paracetamol is utilized. Additionally, it lessens the requirement for opioids [109], and in a multimodal approach to postoperative pain management, it is typically combined with other drugs [110, 111]. When IV paracetamol is administered, the analgesic effect begins quickly (5–10 min), peaks in 1 h, and lasts for 4–6 h [112]. Erdi et al. compared the efficacy and side effects of ibuprofen and paracetamol to be used as a substitute for opioids for pain control post-surgery. While there were no significant differences (p = 0.719) between the mean score of pain in the abdomen in the ibuprofen and paracetamol groups, there was a significant decrease (p < 0.001) compared to the control group. In the ibuprofen and acetaminophen groups, the intensity of shoulder pain, PONV, sedation, and opioid use were not statistically significantly different, but they were significantly less than in the control group [42]. Furthermore, a study involving 316 patients was carried out to compare the analgesic effects of combined pethidine/acetaminophen and parecoxib/acetaminophen. The mean NRS between the two groups was found to be equally effective (p value = 1.000) at (45 min, 2 h, 6 h, 12 h, and 24 h). On the other hand, patients in the acetaminophen monotherapy group had higher NRS scores (p < 0.01) than other groups [43]. In a comparison of ketorolac to paracetamol, a greater number of patients in the ketorolac group reported a VAS > 4, and both groups' pain scores were generally similar. The majority of patients who required postoperative opioid rescue only needed one rescue and analgesic application during their hospital stay, which prevailed between 3 and 12 h, with no statistically significant differences [67]. Additionally, it has been proved by Johnson et al. [58] that a preoperative single dose of oral paracetamol is not inferior to intraoperative IV paracetamol for patients undergoing LC at ambulatory surgery centers and the median end-pain score in the post-anesthesia care unit was 2 for both groups. The confidence interval (CI) upper limit was found to be under the cutoff value of 1 pain score point. To summarize, substituting preoperative per oral (PO) paracetamol for single-dose IV paracetamol in patients undergoing LC is a cost-effective strategy that can be readily implemented in an ambulatory surgical center. There are minimal variations in the pain scores or rescue opioid consumption [58]. However, paracetamol's analgesic efficacy and its ability to regulate the hemodynamic condition of patients undergoing LC were documented by Kamali et al. [22], the mean pain scores at 2, 4, 8, 12, and 24 h did not significantly differ between the paracetamol and dexmedetomidine groups; however, the paracetamol group's pain score was significantly reduced (p = 0.04) than the dexmedetomidine group's. In comparison with the dexmedetomidine group, the paracetamol group's median opioid consumption in the 24 h following surgery was lower, and their mean duration of analgesia was longer. A study conducted to compare paracetamol and opioid analgesics showed that tramadol exhibited higher VAS scores than paracetamol during the 1.5-, 3-, 6-, 12-, and 24-h periods with one patient in the tramadol group having postoperative nausea. There were no negative consequences linked to paracetamol [74]. However, according to Gousheh et al. [82], a randomization process was used to assign candidates for laparoscopic cholecystectomy to either the paracetamol or placebo groups. The difference in the VAS up to 5 h after the procedure was significant, according to a comparison of both arms’ mean VAS (p = 0.01). Nonetheless, the morphine intake within the first 6 h following surgery was comparable across the groups (p = 0.24). It is not an adequate analgesic to use as a monotherapy treatment for controlling moderate postoperative pain. As mentioned in the previously discussed study by Mulita et al. [43], the combinations of pethidine/acetaminophen and parecoxib/acetaminophen were more successful than acetaminophen monotherapy. Based on the demonstrated evidence, the consistent efficacy, favorable safety profile, and versatility in combination therapies position IV paracetamol as a central component in non-opioid pain management strategies post-LC.
Nonsteroidal anti-inflammatory drugs
Diclofenac
Diclofenac is a phenylacetic acid class NSAID with analgesic, antipyretic, and anti-inflammatory properties. Diclofenac inhibits cyclooxygenase, an essential enzyme that converts arachidonic acid into several prostaglandins that are mediators of pain and inflammation [113, 114]. For the treatment of acute painful and inflammatory disorders, diclofenac is a well-tolerated and effective NSAID. Because of its short duration, it is the most often used NSAID for treating pain following surgery for many years [115]. Moreover, rectal suppository and transdermal patch can be used to administer diclofenac. These drug delivery methods avoid first-pass metabolism, have higher bioavailability, lower risk of gastrointestinal problems, fewer systemic side effects, and more patient adherence [116, 117]. The effectiveness of tramadol vs diclofenac in treating pain after LC procedures has been the subject of numerous randomized trials. Zaman et al. [64] conducted a study to compare IV tramadol and diclofenac analgesia following LC. Diclofenac showed varying effectiveness over time: seven patients felt relief within 8 h, 12 between 9 and 16 h, and 18 within 17–24 h post-surgery. Comparatively, tramadol eased pain for 16 patients in the first 8 h, 21 patients between 9 and 16 h, and 25 patients within 17–24 h after the operation. These patterns suggest differences in the onset and duration of pain relief between the two medications. Patients who received a tramadol infusion reported experiencing more nausea and vomiting than those who received diclofenac for pain relief but the incidence of gastritis was higher in the diclofenac group. Sinha et al. [81] also in their study showed at 12 h after surgery, the change in the VAS score was determined to be highly significant (p = 0.00071). The mean VAS scores at 12 h were greater in both arms, with two patients in the diclofenac group having values above 30. Furthermore, another study comparing the preemptive efficacy of diclofenac, ketorolac, and tramadol on postoperative pain found that pain can be adequately controlled for the first 24 h with little to no supplementation of low-dose IV opioid analgesics. In this study, 60 patients were randomly assigned to each drug group given IV half an hour before induction. Ketorolac and tramadol have similar analgesic efficacy and are greater than diclofenac. The use of the medications did not present any notable side effects [85]. Based on these investigations, we found that patients who received injectable tramadol experienced a smoother recovery than those who received diclofenac, with fewer adverse effects. A study compared oral, intramuscular (IM), and transdermal diclofenac for post-LC pain in 90 patients. Patches and IM injections provided better pain relief as indicated by lower VAS scores than oral diclofenac. IM had the lowest postoperative (Ramsey sedation score), while oral caused the most. Postoperative modified Aldrete's score system (MASS) was similar across groups. Patch and IM groups needed less tramadol medication. No side effects or PONV were reported for transdermal or IV administration. For outpatient LC, patches seem ideal, offering good pain control with fewer opioid-related issues. [78].
Ketoprofen
Ketoprofen is a commonly used NSAID that is derived from phenylpropionic acid. It has analgesic, anti-inflammatory, and antipyretic effects. It works by blocking the cyclooxygenase pathway in both injured tissue and spinal neurons, which decreases nociceptive transmission, and it is frequently used to alleviate mild to moderate postoperative pain [86, 118]. Because of these qualities, ketoprofen is a good option for treating acute, and chronic pain and inflammation symptoms. When compared to diclofenac, ketoprofen has a much greater overall efficacy and may provide analgesia for a longer period in the postoperative setting [119]. A dose of 50–100 mg of ketoprofen is given after surgery involving moderate tissue injury, such as LC [120]. A study showed the systemic use of the preoperative infusion of ketoprofen led to a higher proportion of patients not needing the second analgesic and considerably better pain management (p = 0.001) than postoperative ketoprofen and preoperative and postoperative propacetamol, particularly in the first 3 h after surgery and compared to ketoprofen, there was no benefit to propacetamol preoperative use [86]. Another study [87] was conducted where 100 patients were randomly divided into five groups, each receiving different doses of ketoprofen and bupivacaine. Groups 1 to 4 were given different doses of ketoprofen and bupivacaine, and the control group received 40 mL of IP NS and 40 mL of IV NS, Table 1. Results showed that all groups had significantly reduced abdominal pain levels compared to the control group; however, group 3 which was administered 200 mg of intravenous ketoprofen, and 40 mL of 0.25% bupivacaine intraperitoneal spray had lower rates of postoperative vomiting and rescue analgesics. It is therefore advisable to use a combination of 200 mg of IV ketoprofen and 40 mL of 0.25% bupivacaine intraperitoneal spray for a multimodal approach to pain control after LC. Finally, it may be concluded that ketoprofen might be a useful therapeutic alternative for pain alleviation following surgery.
Centrally acting, non-opioid analgesic
Nefopam
Nefopam is a centrally acting, non-opioid, nonsteroidal painkiller that blocks dopamine, norepinephrine, and serotonin reuptake. It was discovered in the 1960s and is classified as part of the benzoxazine class that controls postoperative pain [121,122,123]. Nefopam has been widely available by rectal, oral, and parenteral injections [124]. Nefopam also inhibits sodium and calcium channels that are voltage-sensitive. Postsynaptic receptor activity is reduced due to these effects. It follows that nefopam may affect postsynaptic glutamatergic receptors, including n-methyl-d-aspartate (NMDA) receptors [125,126,127]. Given these characteristics, nefopam may be used to treat acute postoperative pain, delay the onset of chronic pain, and minimize sensory abnormalities that have been widely utilized in Europe [124, 128, 129]. Nefopam has been utilized as an analgesic and as a part of multimodal analgesia for enhanced recovery after surgery (ERAS) in several surgical operations [121, 130, 131]. Moreover, nefopam used perioperatively in orthopedic surgeries reduces immediate postoperative pain scores and significantly spares morphine without having a substantial adverse effect. It appears that patients with severe preoperative pain are particularly influenced by this analgesic effect [132]. Furthermore, research has demonstrated that perioperative nefopam lowers the amount of opioids used following hysterectomy, breast cancer surgery, upper abdomen surgery, and middle ear surgery. For this reason, nefopam is a useful analgesic adjuvant during and after surgery [133,134,135]. Many clinical trials designed to assess its effect on LC postoperative pain, accordingly Jung et al. [51] hypothesized that a PCA pump with nefopam alone is just as good at managing pain after LC as using a combination of nefopam and fentanyl, but with potentially fewer side effects. A total of 78 patients were allocated equally to each group in this perspective and consequently, NRS scores did not differ significantly across the groups during the recovery period following surgery nor at 30 min after admission, as well as 8 and 24 h after surgery. Other outcomes were not substantially different between the two groups and there was no significant difference in postoperative adverse effects. A comparative study evaluated the efficacy of intraoperative nefopam versus ketamine infusions for postsurgical pain management. The trial involved 60 patients randomly divided into three groups: nefopam (0.3 mg/kg IV bolus followed by 65 µg/kg/h infusion), ketamine (0.3 mg/kg IV bolus followed by 180 µg/kg/h infusion), and a control group receiving saline. Researchers assessed postoperative pain scores and analgesic requirements over the first 8 h. Results showed that both nefopam and ketamine groups experienced significantly lower pain scores and reduced fentanyl needs compared to the control group, particularly in the first hour post-surgery (p < 0.05). Notably, no significant differences were observed between the nefopam and ketamine groups, suggesting comparable efficacy in pain management [69]. Nevertheless, Choi et al. [71] proved that the total quantity of intraoperative remifentanil and postoperative supplementary morphine significantly decreased by co-administration of nefopam or ketamine. Regarding the postoperative VAS score and recovery index, the nefopam group performed was more effective than the control and ketamine groups. Compared to the ketamine group, the nefopam group had less morphine amount required, though not significantly.
Alpha-2-agonists
Dexmedetomidine
Desirable effects of alpha-2 agonists include analgesia and sedation. Although it complicates the interpretation of analgesic effects, alpha-2 agonist-induced sedation is a component of the overall analgesic impact that incorporates spinal and supraspinal pathways [136]. Highly selective α2 adrenergic agonist dexmedetomidine is a novel clonidine-like compound that can enhance postoperative analgesia by reducing hemodynamic disturbances and anesthetic demand by reducing endogenous catecholamine release [137, 138]. In mechanical ventilation and/or sedation-dependent surgeries, dexmedetomidine (DEX) has been used as a solo sedative or as an adjunct medication for operating anesthesia and postoperative care. According to several research, intraoperative dexmedetomidine administration promoted a quick and easy recovery after surgery, decreased postoperative pain, and increased patient satisfaction. The quality of recovery (QoR) score following major abdominal and spinal operations may be enhanced by the preoperative injection of dexmedetomidine [139, 140]. During intraoperative usage, dexmedetomidine acts as an adjuvant to reduce the stress response brought on by anesthesia and surgery while preserving hemodynamic stability [70]. Prior research has indicated that dexmedetomidine has the potential to alleviate postoperative pain during laparoscopic cholecystectomy surgery since the administration of dexmedetomidine infusion was linked to a significantly longer period before requiring rescue analgesia, a significantly reduced frequency of severe postoperative pain, and a significantly lower amount of opioids during surgery included a decreased incidence of chronic postsurgical pain, a lower incidence of PONV, and significantly lower consumption of fentanyl both intraoperatively and at the end of surgery to extubation (p = 0.001). There were no differences between groups in the lengths of hospitalization in the ICU or overall hospital stay nor the median pain intensity of 3 h, 6 h, 12 h, or 24 h following surgery [63]. A study conducted by Ye et al. [49] demonstrated that when administering intravenous dexmedetomidine at a dose of 0.6 μg/kg before induction, patients having LC can experience significantly less cough intraoperatively and less pain postoperatively. Additionally, it was reported that the postoperative first analgesic requirement time was longer and the pain scores in the ketamine and dexmedetomidine groups were lower than that of the control group (p < 0.001) at all periods over the 48-h monitoring time. Intravenous PCA opioid intake was greater in the dexmedetomidine group (p < 0.001) and in the control group (p < 0.001) when compared to the ketamine group [35]. In another investigation, it was shown that the postoperative VAS score of the dexmedetomidine group was reduced. The dexmedetomidine group displayed a reduced 24-h analgesic demand than the control group, although this difference was not significant. The control group experienced a significant hemodynamic stress response during tracheal intubation, laryngoscopy, formation of pneumoperitoneum, and extubation. A substantial attenuation of the hemodynamic response between the dexmedetomidine and control arms was also revealed. No noteworthy side effects were reported [14, 55]. Nevertheless, time for rescue analgesics was significantly (p = 0.00) lower in the IV group and IP group compared to the control group in a randomized trial using bupivacaine following LC. In the first 12 h, the mean VAS level of pain was similar in the IV and IP groups. Parecoxib and dexmedetomidine combined were also shown to have the lowest total patient-controlled intravenous analgesia (PCIA) press times during 48 h following LC, and their VAS values were significantly less than those of any other group, according to research done by Du et al. [57] to estimate the protective value of this combination on postoperative pain attenuation and early cognitive impairment in elderly patients undergoing LC. The control group had the lowest scores when compared to other groups, and the combination group had the highest Ramsay and mini-mental state examination (MMSE) scores. Finally, a study conducted by Kaarthika et al. [50] compared pain management strategies using different drug combinations. One group received bupivacaine alone, another received bupivacaine with clonidine, and the third received bupivacaine with dexmedetomidine. The clonidine group requested pain relief first, followed by the bupivacaine-only group and the dexmedetomidine group went the longest before requesting pain relief. These differences were significant, suggesting that combining dexmedetomidine with bupivacaine might ensure longer-lasting pain control than the other options. Patients given bupivacaine with dexmedetomidine needed more fentanyl than those receiving bupivacaine with clonidine. Both groups needed significantly less additional pain relief than patients given only bupivacaine, who required an average of 35.7 μg fentanyl. The results suggest that adding either dexmedetomidine or clonidine to bupivacaine can reduce the request for extra pain medication.
N-methyl-D-aspartate receptor antagonist
Ketamine
Ketamine is a noncompetitive antagonist of the N-methyl-D-aspartate (NMDA) receptor that may be used as an anesthetic at large dosages and as an analgesic at low levels [141]. Whether it is co-administered with other anesthetics or not [142], low-dose ketamine has shown a significant reduction in the quantity of opioids needed as well as nausea following abdominal surgery. Ketamine anesthesia has been licensed for use in postoperative pain treatment [143]. Also, it has been noted that a single bolus dosage of ketamine does not cause the side effects that are often observed with the infusion [142]. As mentioned previously, ketamine has an important role that is like that of dexmedetomidine in terms of how it affects total intravenous anesthesia on LC postoperative analgesia, complete intravenous anesthesia, and the reduction of opioid intake [35]. Comparing the opioid-based group to the opioid-free group, Vishnuraj et al. [15] demonstrated that the combination of dexmedetomidine and ketamine results in significantly less analgesia being needed within the first 2 h. The groups' intake of fentanyl at 6 h, however, was comparable (152 ± 28.2 vs. 164 ± 33.4, P = 0.061). It was concluded that giving dexmedetomidine and ketamine together in an opioid-free anesthesia technique with decreased PONV may be an alternative for certain patients undergoing elective LC [15]. Furthermore, ketamine and diclofenac combined patients rated much lower on the pain scale than either ketamine or a placebo, according to research done to evaluate the impact of prophylactic use of both medications. After surgery, analgesics were required for all research groups; however, patients receiving diclofenac and ketamine combined took longer to request analgesia than patients receiving diclofenac alone (p value = 0.03), ketamine (p value < 0.001), or a placebo (p value < 0.001) [83]. However, recent research showed that a single intraoperative ketamine bolus had a substantial pain-relieving effect that persisted for just half an hour following LC. The two group's numerical pain rating scale scores did not significantly vary at other times. Compared to the control arm, the ketamine arm experienced a more prolonged analgesia and a higher sedation score. There were no notable differences between the groups in the incidence of chronic pain or the cumulative tramadol demand at 24 h. However, the limited population sample size in this study prevented the investigation of the analgesic impact on dynamic pain. [34].
Memantine
Memantine is a low-affinity, noncompetitive receptor antagonist that prevents NMDA receptors from being pathologically activated without altering the physiological functioning of the receptors and is better tolerated in patients since it is an open-channel blocker [144, 145]. Memantine has been approved for the treatment of Alzheimer's disease for several years and has the benefit of having few side effects at doses that are within the therapeutic range [146]. The NMDA receptor is activated by prolonged, high-intensity pain inputs. Neuronal excitation and aberrant pain manifestations, such as spontaneous pain, allodynia, and hyperalgesia, are linked to NMDA receptor activation and abnormalities in the peripheral and central sensory system [147,148,149]. Therefore, pain may be reduced if antagonists block these receptors. This raised the researchers' focus on memantine which has shown promising results in clinical trials for improving memory, learning, pain, and neuroprotective properties [150] with several benefits over ketamine, including a decreased risk of adverse effects, a higher potency, and a slower elimination half-life (60–80 h) as opposed to ketamine's (2.5 h) [151]. Numerous studies have examined, with varying degrees of success, the use of memantine as an opioid-sparing adjuvant when given as a premedication before surgery. Morel et al. demonstrated the efficacy of memantine in the prevention of postsurgical pain in females undergoing mastectomy by administering 5–20 mg/day of memantine two weeks before surgery, and it was continued for an additional two weeks following surgery at a dose of 20 mg/day. Based on the data, patients who received memantine had significantly reduced levels of rescue analgesia, improved emotional states, and significantly less post-mastectomy pain at three months [152]. According to Rahimzadeh et al. [153], a double-blind RCT revealed that, as compared to a placebo, providing patients with 20 mg of oral memantine before dacryocystorhinostomy significantly decreased their postoperative pain. According to a preclinical investigation, memantine, when given to a neuropathic pain model four days before surgery, inhibits the development of cognitive impairment and neuropathic pain symptoms [154]. A randomized, double-blind study that began 20–30 mg/day of memantine immediately following upper limb amputation for four weeks showed that the incidence of phantom limb pain decreased by nearly four times six months after the procedure [155].
In conclusion, memantine is a helpful adjuvant when administered in the early stages of phantom limb pain or right after surgery in patients who are tolerant to opioids. Based on these data, Karri et al. conducted a study on 60 patients to compare the efficacy of memantine versus gabapentin on postoperative pain following LC. An hour before the surgery, patients were given oral gabapentin 600 mg, memantine 20 mg, or a placebo. Compared to the other two groups, the gabapentin group scored lower on the NRS at 15 min and 1 h after surgery. The mean time for the memantine group to request rescue analgesia was 50.53 min longer than that of the gabapentin and placebo groups. Analgesiometer-based objective pain evaluation revealed no statistically significant differences in threshold or tolerance values between the three groups. Compared to the other two groups, the gabapentin group had greater Ramsay sedation scores. This suggests that even when administered alone, gabapentin reduces postoperative pain more effectively than memantine [46].
Magnesium
It has long been known that magnesium is an important cation. Regarding the antinociceptive effect, magnesium works by blocking the NMDA receptors non-competitively, blocking calcium from entering the cell, thereby attenuating pain and central sensitization. This is the basic mechanism behind the use of magnesium in acute and chronic pain conditions such as postoperative pain [156, 157], acute migraine attacks [158], dysmenorrhea [159], neuropathic pain [160], and fibromyalgia [161]. Several investigators have demonstrated studies to report the magnesium sulfate (MgSO4) analgesia effect for postoperative pain in different procedures like thoracotomy, hysterectomy, and laparoscopic sleeve gastrectomy was assessed, finding that the administration of magnesium decreased the amount of opioids required for pain relief without any adverse effects [162,163,164]. Pain management is also impacted by oral magnesium (in the form of lozenges or tablets) not only injections [165]. Additionally, systematic reviews suggested that in addition to reducing opioid intake to a lesser amount, IV magnesium lowers the level of pain scores, clinical toxicities were not documented in any of the examined studies [166,167,168]. As a result of different randomized trials, Akhondi and Sarkoohi et al. [24] reported that analgesic intake during recovery and 6 h post-surgery was lower in the magnesium group than in the control group (p < 0.001). Compared to the control group, the intervention group's mean pain score during recovery and the first 2-, 6-, and 12-h following surgery (p < 0.001) was significantly lower. In conclusion, magnesium sulfate is a safe and effective supplement that can help minimize postoperative pain and the need for opioids by intraoperative IV magnesium. Furthermore in another trial, 60 patients were randomized into three groups comparing the analgesic effect of different doses of the preemptive IV magnesium sulfate along with the control group receiving IV normal saline found that the VAS score at 5.0 and 7.5 mg/kg; however, 7.5 mg/kg proved to be more successful and significantly lower than the control group in early postoperative pain and consumption of analgesics required following laparoscopic cholecystectomy was considerably decreased. However, there was no difference in pain relief at 6, 9, or 24 h [80]. Additionally, Mentes et al. [84] found that patients who had laparoscopic cholecystectomy in the 50 mg/kg magnesium sulfate group 0, 4, and 12 h after surgery had lower pain scores and narcotic doses compared with the normal saline group. The average VAS score was statistically significant between groups at rest and during coughing periods during the first 24 h after surgery, which was consistent with the results. Jijo et al. [39] found that patients treated with magnesium sulfate (MgSO4) had considerably lower mean pain levels in the first six postoperative hours, and the time to first analgesic demand was significantly prolonged. Between the two groups, the incidence of shoulder pain was found to be less than 10% and statistically insignificant. A result indicating that IP magnesium sulfate (MgSO4) during LC results in efficient postoperative analgesia with few adverse effects, as demonstrated by decreased pain scores during the initial 24 h and decreased analgesic use throughout 24 h. Moreover, it significantly decreases the frequency of nausea and vomiting. However, a trial conducted by ElHoshy et al. compared the MgSO4 and esmolol infusion impact on the recovery pain ratings and showed that the recall time for first rescue analgesia did not differ significantly between the two groups under study. This discrepancy between these research results could be attributed to variations in the patient population and different routes of administration [25].
Steroids
Since steroids tend to lessen the inflammatory response to surgery, there is a rising interest in integrating multimodal analgesia protocols and utilizing them to improve postoperative recovery and lessen pain and fatigue [169]. Dexamethasone is a high-potency, long-acting corticosteroid with fewer mineralocorticoid effects than other steroids. Dexamethasone has a well-known antiemetic action, and it is commonly used to PONV [170]. Data from two meta-analyses revealed that IV dexamethasone given once can lessen both postoperative pain and the need for opioids following surgery [171, 172]. Dexamethasone's potency, prolonged half-life, safety record, and cost-effectiveness have made it an ideal option for an outstanding corticosteroid [173]. It has been shown that dexamethasone inhibits peripheral phospholipase, hence reducing the production of pain-aggravating products from the pathways of cyclooxygenase and lipoxygenase [174]. Recent randomized controlled trials revealed that IP bupivacaine and IV dexamethasone together may be a highly effective combination for reducing PONV and postoperative pain [175]. Patients scheduled for LC participated in a double-blind clinical trial in which they were randomized into three groups: IP dexamethasone, IV dexamethasone, and control groups. The results showed that in the first 24 h following surgery, the IP group reported less nausea than the control group, but not the IV group. In contrast to the IV group, none of the IP group patients suffered PONV after 8 h. Metoclopramide was administered to patients who experienced PONV at a considerably greater rate in the IV group than in the group given IP dexamethasone (with p = 0.001); however, the level of nausea was less severe in the IP group. Furthermore, the IP group had a significantly lower (p = 0.02) VAS score than the other two groups [38]. A randomized experiment successfully demonstrated that a single-dose IV dexamethasone before surgery significantly lowered the VAS score compared to placebo at 6-, 12-, and 24- but not 2-h following surgery. It is suggested that dexamethasone be used as a safe and efficient medicine to reduce pain after surgery [37]. Additionally, a different randomized trial showed a significant decrease in the VAS score (p value < 0.001) and amount of rescue analgesics used (p value = 0.013) when bupivacaine and dexamethasone were administered intraperitoneally until 2 h after surgery, as opposed to bupivacaine alone. Additionally, compared to the bupivacaine group alone, the combination group took a significantly longer time for the first rescue analgesic to be required [30]. According to Surender et al., the quality of recovery was significantly greater with preoperative single IV bolus dexamethasone compared to the single IV bolus lignocaine. When compared to lignocaine, dexamethasone showed statistically superior pain alleviation, physical independence, and physical comfort. The VAS was lower in the dexamethasone group than in the lignocaine group. The dexamethasone group consumed fewer opioids (364.08 ± 127.31) throughout the postoperative period; however, there was no statistically significant difference seen in either group (p > 0.05) [62]. Nonetheless, when a single intraoperative IV dexamethasone dosage was compared with a placebo the dexamethasone group experienced significantly less pain (p < 0.01) at 2-, 6-, and 12-h intervals, and the group's meperidine intake was significantly lower than that of the control group (p < 0.05) [76]. Conversely, another investigation revealed no statistically significant variation between dexamethasone versus placebo in incisional pain during rest and motion, as well as visceral pain during rest over the 6, 12, and 24 h postoperatively. The study group required lower analgesics and antiemetic medications than the control group; however, the difference between the two groups was not significantly different (p > 0.05), anticipating that a multimodal analgesic and antiemetic combination would provide superior results when used rather than a single medication. Given that dexamethasone was administered 90 min before surgery, variations in this period of administration time and the small sample size might account for the observed discrepancies in the outcomes [176].
Serotonin (5-HT3) antagonist
Ondansetron
5-HT3-antagonists exhibit anti-inflammatory and analgesic qualities, according to many studies, which suggests a possible therapeutic function in pain management [177, 178]. Ondansetron is a selective serotonin (5-HT3) antagonist. It has been shown in earlier research to be able to block sodium channels [179] and opioid receptors [180]. To prevent postoperative nausea and vomiting (PONV), ondansetron is commonly administered as a premedication to patients following gastrointestinal surgery since it blocks serotonin's stimulatory effects on the chemoreceptor trigger zone (CTZ) and the afferent vagal nerve pathway [181]. Nevertheless, because of the multimodal effect of ondansetron, earlier trials demonstrated that it can reduce pain successively following a propofol infusion [182,183,184] and chronic benign neuropathic pain [185] while another recent study found that ondansetron had no discernible or significant effect on propofol pain or PONV over lidocaine [186]. In summary, a recent systematic review discovered that ondansetron significantly lowers moderate and severe pain compared to placebo and is better at reducing the occurrence of pain. In terms of the incidence of patients experiencing no pain, moderate pain, or severe pain, lidocaine outperformed ondansetron [187]. On the other hand, it was shown that ondansetron, when administered subcutaneously, had 15 times the potency of lidocaine, a well-known and successful alternative for managing pain following LC [179]. According to the results of randomized research, IP ondansetron may have a favorable impact on the analgesic effectiveness of acetaminophen in addition to its antiemetic and antinauseant effect, making it a special and innovative choice for managing postoperative pain in patients undergoing LC; shown by the significantly reduced need for rescue analgesia, (p = 0.005) in the ondansetron arm compared to the control arm. The participants who required rescue were found to have consumed a similar cumulative 24-h dose of rescue drugs between the two trial groups with no significant difference (p = 0.785). The ondansetron group's unassisted mobilization time was substantially less than that of the control group (p < 0.001). The AUC of VAS scores and the time required for unassisted mobilization demonstrated a statistically significant analgesic effect from ondansetron [44]. Thus, the analgesic effect of this class of drugs is linked to its local action and may be related to differences in the mode of administration of ondansetron, which was shown to have a significant analgesic effect when administered intraperitoneally because ondansetron did not affect the analgesic effect of paracetamol following surgery when given intravenously in a previous study involving women undergoing laparoscopic hysterectomy [44, 188].
Tropisetron
Tropisetron is a partial α7 nicotinic acetylcholine receptor (a7nAChRs) agonist and a 5HT-3 receptor antagonist that is often utilized for its postoperative antiemetic and anti-nauseous qualities [189]. The central and peripheral nervous systems employ nicotinic acetylcholine receptors, which are ligand-gated ion channels according to previous definitions. Non-ionic signaling pathways through nAChRs have recently been shown in immune cells. Therefore, by reducing the production of inflammatory cytokines, activating a7nAch receptors exerts analgesic benefits. Consequently, targeting these two receptors at the same time may thereby reduce postoperative rebound pain and anxiety. But according to a recent study, orthopedicic patients did not have a lower incidence of rebound pain following surgery when intraoperative tropisetron was used. The main results showed no significant differences (p = 0.487) in rebound pain incidence or NRS score (p = 0.539) between the tropisetron and saline groups 24 h post-surgery. The use of postoperative analgesia with NSAIDs and opioids and patient satisfaction were comparable in both groups. Regarding postoperative adverse events, such as PONV, there were also no appreciable variations. However, the low prevalence of PONV linked to the fact that more patients in the control group consumed alcohol and smoked might also be contributing factors. Furthermore, the trial employed 5 mg of tropisetron to treat postoperative rebound pain; a greater dose could be necessary to show a meaningful improvement in effectiveness. Also, during the first 24 h after surgery, the pain score was not recorded regularly. Inaccurate data may have resulted in incorrect pain score recalling [190]. Its underlying mechanism of action suggests it may be a promising candidate for future investigation in LC.
Non-pharmacological
Acupuncture
Acupuncture is widely regarded as the cornerstone of traditional Chinese medicine (TCM). Many studies conducted in the last few years have demonstrated that preoperative acupuncture has the potential to alleviate anxiety, enhance the preoperative state, and minimize the need for anesthetics. On the other hand, surgical acupuncture can support the recovery of intestinal function and postoperative pain management, minimize postoperative nausea and vomiting, and reduce hospital stay duration [191]. Acupuncture has been shown to suppress pain through the release of endogenous opioid compounds in the central nervous system and to stop harmful signal transmission in the spinal cord by activating Aβ fibers in the peripheral nervous system [192]. Comparing acupuncture to standard care, numerous studies have demonstrated that it is both safe and economical [193,194,195]. In clinical practice, electrical acupuncture and transcutaneous electrical acupoint stimulation (TEAS) have been used in addition to traditional manual acupuncture. The combination of general anesthetic and TEAS is known as acupuncture-drug compound anesthesia [196]. As a complementary and alternative therapy in addition to analgesic medicine, it was helpful in numerous clinical trials involving total knee replacement [197], low back surgery [198], and thoracoscopic surgery [196]. A single-blind RCT examined the effects of acupuncture combined with conventional treatment compared to the effect of conventional treatment alone after lumbar spine surgery, and the result showed that although most subjects were satisfied with their pain management although experienced moderate pain due to inadequate analgesia [199]. This led researchers to demonstrate RCT to investigate its effect on the management of laparoscopic cholecystectomy postoperative pain. Patients undergoing laparoscopic cholecystectomy admitted to the hospital were randomly assigned to one group from each group and received either acupuncture after 2 h from surgery or parecoxib sodium injections at request. The outcomes showed that acupuncture can clinically improve the short-term management of postoperative pain following LC and reduce the need for further analgesics. Therefore, acupuncture may have the potential as one of the multimodal analgesia treatments for postoperative pain [21].
Gas aspiration
Shoulder pain is mostly caused by referred pain from peritoneal irritation, which varies depending on the length of the surgery and the amount of residual CO2 in the tissue [200, 201]. A study has shown that shoulder pain following elective surgical operations, such as cholecystectomy, can be decreased by reducing remaining intra-abdominal gas using a variety of approaches [202]. Carbon dioxide gas aspiration following surgery falls into two categories: passive gas aspiration, in which the gas is released spontaneously, and active gas aspiration, in which the gas is actively extracted using a specific tool or suction [203]. Many studies have shown that active gas aspiration following laparoscopic cholecystectomy is an easy, practical, and safe operation. By lowering postoperative shoulder and abdominal pain and, consequently, the need for analgesics, this procedure can effectively result in a more restful hospitalization for patients following laparoscopic surgery. It also significantly reduces the residual intraperitoneal gas volume and postoperative pain [202, 204,205,206]. A RCT designed to evaluate the effects of usual gas release, active aspiration, and passive-valve release on recovery in patients who have undergone laparoscopic cholecystectomy has shown that the volume of residual CO2 in the intraperitoneal cavity at the end of laparoscopic surgery can be reduced using either the active aspiration or passive-valve release technique, which successfully lowers the degree of postoperative shoulder and abdominal pain. Furthermore, both methods improved the postoperative recovery of patients and decreased the rates of nausea, vomiting, and abdominal pain. Nonetheless, the active aspiration group's ambulation duration was noticeably less than that of the control and passive-valve release groups [65].
Emerged technologies
Virtual reality (VR)
Virtual reality is a new technology that is becoming more and more used in critical care. However, it completely submerges the viewer in a three-dimensional virtual world. VR has a lot of promises to advance critical care medicine for patients, families, and medical professionals. In addition, it has the potential to reduce a patient's pain, anxiety, stress, and fear [207]. With VR, a patient can interact with a simulated environment using all five senses and react to sensory and motor signals [208]. So, it distracts the patients' attention, concentration, and emotions from the real world to the virtual one. As such, because they are not thinking about pain as much, the patients suffer from less intense pain [209, 210]. Additionally, it is important to note that virtual reality therapy has been effectively applied as an analgesic in several acute clinical situations, including burn pain [211], postcardiac surgery [212], and painful procedures [213,214,215]. A total of 150 patients who undergoing LC in the surgical wards participated in a randomized clinical trial in which they were split into three groups at random: control, distraction, and education. When comparing the preoperative anxiety mean scores of the two VR groups to those of the control group, the results showed a significant decrease. Additionally, patients in the two intervention groups showed a statistically significant decrease in their postoperative pain assessments when compared to the control group [20].
Limitations
Several limitations were encountered in the preparation of this narrative review regarding non-opioids for pain relief post-laparoscopic cholecystectomy. Direct comparisons across studies were difficult due to the differences in how findings were reported. Without full method details on each study, we cannot compare the rigor of such methods. Moreover, we have identified variability in the way pain scores were quantified and published which complicates our analysis. A limitation to drawing general conclusions is the variety of interventions, each with its distinct mechanisms. In addition, many studies had relatively brief follow-ups which prevented us from assessing the long-term outcomes and side effects associated with these non-opioid treatments.
Future perspectives
More thorough clinical studies with multiple arms and larger sample sizes are required to determine the best pain management plans for patients undergoing LC and assess the safety and effectiveness of analgesics under comparable clinical circumstances. Long-term effects, such as the likelihood of developing persistent pain following surgery, and the adverse effects of the drugs are crucial and should be assessed. Furthermore, a patient's age, anxiety before surgery, sex, or other preoperative patient-related characteristics may complicate the intensity of postsurgical pain and must be assessed. Though relief is provided by current pain management techniques, future developments in LC may involve personalized pain management. By knowing each patient's unique genetic and pain profile, physicians may be able to prescribe pain medications with fewer adverse effects and better pain control.
Conclusion
Complicated causes contribute to pain after laparoscopic cholecystectomy. To reduce the postoperative pain associated with LC, a variety of drugs are studied by administering either before, during, or after surgery. There was evidence that one essential part of multimodal postoperative pain management is IV paracetamol. Also, many pharmacological drugs including magnesium sulfate, dexamethasone, ondansetron, gabapentinoids, alpha-2-agonists, local anesthetics, antidepressants, and NSAIDs, were useful in controlling pain. Additionally, non-pharmacological and emerging technological approaches proved their effective role in controlling LC postoperative pain. Further in-depth medical research involving various treatment groups and more participants is needed to identify optimal approaches for managing pain in LC patients. This would help evaluate how well different pain medications work and how safe they are when used in similar medical situations. Clinicians should individualize this approach with factors such as patient comorbidities, allergies, and analgesic response records. Regular reviews of pain management results promote modification and improvement of the pain control protocol for maximum effectiveness. When these evidence-based non-opioid strategies are implemented in an orderly manner, post-LC pain control can be significantly improved by physicians while reducing risks associated with opioids.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- 5-HT3:
-
Serotonin receptor
- a7nAch:
-
Alpha-7 nicotinic acetylcholine receptor
- AUC:
-
Area under the curve
- CC:
-
Cubic centimeters
- CI:
-
Confidence interval
- CTZ:
-
Chemoreceptor trigger zone
- DBG:
-
Diluted bupivacaine group
- DEX:
-
Dexmedetomidine
- ERAS:
-
Enhanced recovery after surgery
- ICU:
-
Intensive care unit
- IM:
-
Intramuscular
- IP:
-
Intraperitoneal
- IV:
-
Intravenous
- LC:
-
Laparoscopic cholecystectomy
- MASS:
-
Modified Aldrete's score system
- MgSO4:
-
Magnesium sulfate
- MMSE:
-
Mini-mental state examination
- nAChR:
-
Nicotinic acetylcholine receptor
- NBG:
-
Non-diluted bupivacaine
- NMDA:
-
N-methyl-d-aspartate
- NRS:
-
Numeric rating scale
- NS:
-
Normal saline
- NSAIDs:
-
Nonsteroidal anti-inflammatory drugs
- PCA:
-
Patient-controlled analgesia
- PCIA:
-
Patient-controlled intravenous analgesia
- PO:
-
Per oral
- PONV:
-
Postoperative nausea and vomiting
- POP:
-
Postoperative pain
- QoR:
-
Quality of recovery
- RCT:
-
Randomized clinical trial
- S.C:
-
Subcutaneous
- TAP:
-
Transversus abdominis plane
- TCM:
-
Traditional Chinese medicine
- TEAS:
-
Transcutaneous electrical acupoint stimulation
- VAS:
-
Visual analogue scale
- VR:
-
Virtual reality
References
Kim SS, Donahue TR (2018) Laparoscopic cholecystectomy. JAMA. https://doi.org/10.1001/jama.2018.3438
Cianci P, Restini E (2021) Management of cholelithiasis with choledocholithiasis: endoscopic and surgical approaches. World J Gastroenterol 27:4536–4554
Jiang B, Ye S (2022) Pharmacotherapeutic pain management in patients undergoing laparoscopic cholecystectomy: a review. Adv Clin Exp Med 31:1275–1288
Arabzadeh A, Seyedsadeghi M, Sadeghi N, Nejati K, Erdi AM (2021) Comparison of intraperitoneal bupivacaine and intravenous ketorolac for postoperative pain management following laparoscopic cholecystectomy. Anesth Pain Med. https://doi.org/10.5812/AAPM.114623
Abaid RA, Cecconello I, Zilberstein B (2014) Simplified laparoscopic cholecystectomy with two incisions. ABCD 27:154–156
Luo Z, Wang H, Huang D (2019) The impact of parecoxib on pain management for laparoscopic cholecystectomy: a meta-analysis of randomized controlled trials. Surg Laparosc Endosc Percutan Tech 29(2):69–74. https://doi.org/10.1097/SLE.0000000000000626
Boddy AP, Mehta S, Rhodes M (2006) The effect of intraperitoneal local anesthesia in laparoscopic cholecystectomy: a systematic review and meta-analysis. Anesth Analg 103(3):682–688. https://doi.org/10.1213/01.ane.0000226268.06279.5a
Wei X, Yao X (2020) The impact of intraperitoneal levobupivacaine on pain relief after laparoscopic cholecystectomy: a meta-analysis of randomized controlled studies. Surg Laparosc Endosc Percutan Tech 30(1):1–6. https://doi.org/10.1097/SLE.0000000000000742
Bisgaard T, Rosenberg J, Kehlet H (2005) From acute to chronic pain after laparoscopic cholecystectomy: a prospective follow-up analysis. Scand J Gastroenterol 40(11):1358–1364. https://doi.org/10.1080/00365520510023675
Hilda Onuţu A (2015) Duloxetine, an antidepressant with analgesic properties – a preliminary analysis. Rom J Anaesth Intensive Care 22(2):123–128
Garimella V, Cellini C (2013) Postoperative pain control. Clin Colon Rectal Surg 26(3):191–196. https://doi.org/10.1055/s-0033-1351138
Bisgaard T, Warltier DC (2006) Analgesic treatment after laparoscopic cholecystectomy. Anesthesiology 104(4):835–846. https://doi.org/10.1097/00000542-200604000-00030
Abdelraheem Mohamed M, Elsayed HMA, Badawy FA (2024) A comparative study of the analgesic efficacy of intraperitoneal instillation of diluted bupivacaine versus non-diluted bupivacaine after laparoscopic cholecystectomy, a prospective single-blinded controlled randomized study. Egypt J Anaesth 40(1):1–9. https://doi.org/10.1080/11101849.2023.2295047
Zheng L, Fang T, Zhang W, Zhang X, Ren Z, Qin W, Liang W, Ma Q, Yin N (2024) Beneficial effects of low-dose intravenous dexmedetomidine premedication in patient undergoing laparoscopic cholecystectomy under general anesthesia: a prospective, double-blind, randomized controlled trial. Drug Des Dev Ther 18:443–452. https://doi.org/10.2147/DDDT.S452077
Vishnuraj KR, Singh K, Sahay N, Sinha C, Kumar A, Kumar N (2024) Opioid-free anesthesia using a combination of ketamine and dexmedetomidine in patients undergoing laparoscopic cholecystectomy: a randomized controlled trial. Anesth Pain Med 19(2):109–116. https://doi.org/10.17085/apm.23097
Uzunay NT, Mingir T, Erginoz E, Karakas DO, Kose E (2024) Comparison of laparoscopic-guided versus ultrasound-guided TAP block in laparoscopic cholecystectomy. Cirugia y Cirujanos (English Edition) 92(2):174–180. https://doi.org/10.24875/CIRU.23000394
Jeffrey KN, Thelen AE, Dreimiller AM, Tollinche LE, Alkhatib H, Dorsey A, El-Hayek KM (2023) Laparoscopic transversus abdominis plane block reduces postoperative opioid requirements after laparoscopic cholecystectomy. In: Surgery (United States). Elsevier Inc., pp 864–869
Korkutata Z, Tekeli AE, Kurt N (2023) Intraoperative and postoperative effects of dexmedetomidine and tramadol added as an adjuvant to bupivacaine in transversus abdominis plane block. J Clin Med. https://doi.org/10.3390/jcm12227001
Çevikkalp E, Narmanlı M, Özgüç H, Ocakoğlu G (2023) Bilateral 4-quadrant laparoscopic-assisted transversus abdominis plane block reduces early postoperative pain after laparoscopic cholecystectomy A prospective, single-blind, randomized study. Saudi Med J 44(2):145–154. https://doi.org/10.15537/smj.2023.44.2.20220407
Abbasnia F, Aghebati N, Miri HH, Etezadpour M (2023) Effects of patient education and distraction approaches using virtual reality on pre-operative anxiety and post-operative pain in patients undergoing laparoscopic cholecystectomy. Pain Manag Nurs 24(3):280–288. https://doi.org/10.1016/j.pmn.2022.12.006
Wang F, Peng P, Zheng Y, Cheng S, Chen Y (2023) Effect of acupuncture on postoperative pain in patients after laparoscopic cholecystectomy: a randomized clinical trial. Evid Based Complement Altern Med. https://doi.org/10.1155/2023/3697223
Kamali A, Ashrafi TH, Rakei S, Noori G, Norouzi A (2018) A comparative study on the prophylactic effects of paracetamol and dexmedetomidine for controlling hemodynamics during surgery and postoperative pain in patients with laparoscopic cholecystectomy. Medicine (United States). https://doi.org/10.1097/MD.0000000000013330
Sravanthi GC, Abuji K, Soni SL, Nagaraj SS, Sharma A, Jafra A, Tandup C, Kurdia KC, Dahiya D (2023) Effect of intraperitoneal magnesium sulfate in the prevention of postoperative pain in daycare laparoscopic cholecystectomy: a prospective randomized controlled trial. Indian J Pharmacol 55(3):174–178. https://doi.org/10.4103/ijp.ijp_827_22
Akhondi M, Sarkoohi A (2023) Effect of intravenous injection of magnesium sulphate on intraoperative end-tidal CO2 level and postoperative pain in laparoscopic cholecystectomy. Anesth Pain Med. https://doi.org/10.5812/aapm-135189
ElHoshy HS, El-Din Yacout AG (2023) Efficacy of esmolol versus magnesium sulphate on quality of recovery in patients undergoing laparoscopic cholecystectomy: randomized controlled study. Egypt J Anaesth 39(1):665–672. https://doi.org/10.1080/11101849.2023.2240659
Gupta S, Attal P, Mehta N, Saini H, Banerjee S (2023) Comparison of dose–response to two different doses of intravenous lidocaine for analgesia in patients undergoing elective laparoscopic cholecystectomy under general anesthesia. Ain-Shams J Anesthesiol. https://doi.org/10.1186/s42077-023-00390-y
Sarakatsianou C, Perivoliotis K, Baloyiannis I, Georgopoulou S, Tsiaka A, Tzovaras G (2023) Efficacy of intraoperative intravenous lidocaine infusion on postoperative opioid consumption after laparoscopic cholecystectomy: a randomized controlled trial. Langenbecks Arch Surg. https://doi.org/10.1007/s00423-023-02937-x
Kaur S, Turka S, Kaur Bindra T, Tuteja RD, Kumar M, Jit Singh Bajwa S, Kurdi MS, Sutagatti AJ (2023) Comparison of the efficacy of pregabalin and gabapentin for preemptive analgesia in laparoscopic cholecystectomy patients: a randomised double-blind study. Cureus. https://doi.org/10.7759/cureus.46719
Sane S, Sayyadi S, Abbasivash R, Rezaei S, Azadfar A, Salimi S (2023) Comparison of the effect of preoperative oral tizanidine and pregabalin on shoulder pain in laparoscopic cholecystectomy under general anesthesia. Adv Biomed Res 12(1):58. https://doi.org/10.4103/abr.abr_222_22
Vandana P, Ananya N, Muralikrishna D, Ponduru S, Renganathan V, Gopinath R (2023) Analgesic efficacy of intra-peritoneal instillation of dexamethasone and bupivacaine versus bupivacaine following laparoscopic cholecystectomy: a randomised, double-blind controlled study. Indian J Anaesth 67(11):999–1003. https://doi.org/10.4103/ija.ija_275_23
Nikoubakht N, Faiz SHR, Mousavie SH, Shafeinia A, Borhani Zonoz L (2022) Effect of bupivacaine intraperitoneal and intra-abdominal bicarbonate in reducing postoperative pain in laparoscopic cholecystectomy: a double-blind randomized clinical trial study. BMC Res Notes. https://doi.org/10.1186/s13104-022-06083-3
Iqbal A, Khodavirdipour A, Ravishankar H (2022) Irrigation with bupivacaine at the surgical bed for postoperative shoulder tip and abdominal pain relief after laparoscopic cholecystectomy. Surg J 08(04):e312–e315. https://doi.org/10.1055/s-0042-1758141
Mansour NO, Boraii S, Elnaem MH, Elrggal ME, Omar T, Abdelraouf A, Abdelaziz DH (2022) Evaluation of preoperative duloxetine use for postoperative analgesia following laparoscopic cholecystectomy: a randomized controlled trial. Front Pharmacol. https://doi.org/10.3389/fphar.2022.944392
Jain S, Nazir N, Mustafi SM (2022) Preemptive low-dose intravenous ketamine in the management of acute and chronic postoperative pain following laparoscopic cholecystectomy: a prospective randomized control study. Med Gas Res 12(4):141–145. https://doi.org/10.4103/2045-9912.337995
Efe Mercanoglu E, Girgin Kelebek N, Turker G, Aksu H, Ozgur M, Karakuzu Z, Turkcan S, Ozcan B (2022) Comparison of the effect of ketamine and dexmedetomidine combined with total intravenous anesthesia in laparoscopic cholecystectomy procedures: a prospective randomized controlled study. Int J Clin Pract. https://doi.org/10.1155/2022/1878705
Najam F, Jafri N, Khan MN, Daraz U (2022) Reduction of acute postoperative pain with pre-emptive pregabalin following laparoscopic cholecystectomy. Cureus. https://doi.org/10.7759/cureus.27783
Jamil K, Qaisar R (2022) The effect of dexamethasone on postoperative pain in patients after laparoscopic cholecystectomy. Cureus. https://doi.org/10.7759/cureus.32067
Nazemroaya B, Keleidari B, Arabzadeh A, Honarmand A (2022) Comparison of intraperitoneal versus intravenous dexamethasone on postoperative pain, nausea, and vomiting after laparoscopic cholecystectomy. Anesth Pain Med. https://doi.org/10.5812/aapm-122203
Jijo J, Rashmi R, Fijul K (2022) Postoperative analgesia in laparoscopic cholecystectomy following intraperitoneal magnesium sulphate: a prospective cohort study. J Clin Diagn Res. https://doi.org/10.7860/jcdr/2022/59201.16860
Saliminia A, Yekta Y, Azimaraghi O, Shamabadi A, Naderi S, Movafegh A (2022) Evaluation of the effect of Transversus Abdominis Plane (TAP) block on post-laparoscopic cholecystectomy stress responses: a randomized controlled trial. Archives of Anesthesiology and Critical Care 8 (Supp.1):399–406
Kiany F, Meshkati Yazd SM, Shahriarirad R, Kamran H, Karoobi M, Shabani Mofrad N, Kamali M (2022) Evaluation of post laparoscopic cholecystectomy pain after subcutaneous injection of lidocaine at port site versus lidocaine spray on gallbladder bed after cholecystectomy: a randomized controlled trial. Langenbecks Arch Surg 407(7):2853–2859. https://doi.org/10.1007/s00423-022-02645-y
Erdi AM, Arabzadeh A, Issazadeh Far K, Masoumzadeh M, Bahadoram M (2022) Comparing the efficacy and side effects of intravenous ibuprofen and acetaminophen in pain control following laparoscopic cholecystectomy. World J Plast Surg 11(1):117–124. https://doi.org/10.52547/wjps.11.1.117
Mulita F, Karpetas G, Liolis E, Vailas M, Tchabashvili L, Maroulis I (2021) Comparison of analgesic efficacy of acetaminophen monotherapy versus acetaminophen combinations with either pethidine or parecoxib in patients undergoing laparoscopic cholecystectomy: a randomized prospective study. Med Glas 18(1):80–85. https://doi.org/10.17392/1245-21
Abdelaziz DH, Boraii S, Cheema E, Elnaem MH, Omar T, Abdelraouf A, Mansour NO (2021) The intraperitoneal ondansetron for postoperative pain management following laparoscopic cholecystectomy: a proof-of-concept, double-blind, placebo-controlled trial. Biomed Pharmacother. https://doi.org/10.1016/j.biopha.2021.111725
Jain R, Kumar M, Singh T, Rautela RS, Kumar S (2021) Effect of oral gabapentin premedication on hemodynamic parameters and postoperative pain in patients of laparoscopic cholecystectomy: a randomized double-blind controlled study. J Anaesthesiol Clin Pharmacol 37(1):67–72. https://doi.org/10.4103/joacp.JOACP_439_19
Karri S, Jayaram K, Kumar A, Durga P (2021) Comparison of efficacy of gabapentin and memantine premedication in laparoscopic cholecystectomies for postoperative pain relief: a randomised placebo controlled trial. Indian J Anaesth 65(7):539. https://doi.org/10.4103/ija.ija_140_21
Vijayaraghavalu S, Bharthi Sekar E (2021) A comparative study on the postoperative analgesic effects of the intraperitoneal instillation of bupivacaine versus normal saline following laparoscopic cholecystectomy. Cureus. https://doi.org/10.7759/cureus.14151
Kim HY, Choi JB, Min SK, Chang MY, Lim GM, Kim JE (2021) A randomized clinical trial on the effect of a lidocaine patch on shoulder pain relief in laparoscopic cholecystectomy. Sci Rep. https://doi.org/10.1038/s41598-020-80289-y
Ye Q, Wang F, Xu H, Wu L, Gao X (2021) Effects of dexmedetomidine on intraoperative hemodynamics, recovery profile and postoperative pain in patients undergoing laparoscopic cholecystectomy: a randomized controlled trial. BMC Anesthesiol. https://doi.org/10.1186/s12871-021-01283-z
Kaarthika T, Radhapuram S, Samantaray A, Pasupuleti H, Hanumantha Rao M, Bharatram R (2021) Comparison of effect of intraperitoneal instillation of additional dexmedetomidine or clonidine along with bupivacaine for post-operative analgesia following laparoscopic cholecystectomy. Indian J Anaesth 65(7):533. https://doi.org/10.4103/ija.ija_231_21
Jung KT, So KY, Kim SC, Kim SH (2021) Effect of nefopam-based patient-controlled analgesia with and without fentanyl on postoperative pain intensity in patients following laparoscopic cholecystectomy: a prospective, randomized, controlled, double-blind non-inferiority trial. Medicina (Lithuania) 57:4. https://doi.org/10.3390/medicina57040316
Vindal A, Sarda H, Lal P (2021) Laparoscopically guided transversus abdominis plane block offers better pain relief after laparoscopic cholecystectomy: results of a triple blind randomized controlled trial. Surg Endosc 35(4):1713–1721. https://doi.org/10.1007/s00464-020-07558-9
Tekeli AE, Eker E, Bartin MK, Öner MÖ (2020) The efficacy of transversus abdominis plane block for postoperative analgesia in laparoscopic cholecystectomy cases: a retrospective evaluation of 515 patients. J Int Med Res. https://doi.org/10.1177/0300060520944058
Singh T, Kathuria S, Jain R, Sood D, Gupta S (2020) Premedication with pregabalin 150mg versus 300mg for postoperative pain relief after laparoscopic cholecystectomy. J Anaesthesiol Clin Pharmacol 36(4):518–523. https://doi.org/10.4103/joacp.JOACP_440_19
Chilkoti GT, Karthik G, Rautela R (2020) Evaluation of postoperative analgesic efficacy and perioperative hemodynamic changes with low dose intravenous dexmedetomidine infusion in patients undergoing laparoscopic cholecystectomy: a randomised, double-blinded, placebo-controlled trial. J Anaesthesiol Clin Pharmacol 36(1):72–77. https://doi.org/10.4103/joacp.JOACP_184_17
Chilkoti GT, Kumar M, Mohta M, Saxena AK, Sharma N, Singh J (2019) Comparison of postoperative analgesic efficacy of low-dose bolus intravenous dexmedetomidine and intraperitoneal dexmedetomidine with bupivacaine in patients undergoing laparoscopic cholecystectomy: a randomised, controlled trial. Indian J Anaesth 63(2):106–113. https://doi.org/10.4103/ija.IJA_440_18
Du X, Song F, Zhang X, Ma S (2019) Protective efficacy of combined use of parecoxib and dexmedetomidine on postoperative hyperalgesia and early cognitive dysfunction after laparoscopic cholecystectomy for elderly patients. Acta Cir Bras. https://doi.org/10.1590/s0102-865020190090000005
Johnson RJ, Nguyen DK, Acosta JM, O’Brien AL, Doyle PD, Medina-Rivera G (2019) Intravenous versus oral acetaminophen in ambulatory surgical center laparoscopic cholecystectomies: a retrospective analysis. P T 44(6):359–363
Ghadami N, Barzanji A, Nasseri K, Sarshivi F, Nouri B (2019) Effect of gabapentin in comparison with hydrocortisone on postlaparoscopic cholecystectomy pain control. J Fam Med Prim Care 8(2):652. https://doi.org/10.4103/jfmpc.jfmpc_407_18
Von Plato H, Mattila K, Poikola S, Löyttyniemi E, Hamunen K, Kontinen V (2019) Risk-based targeting of adjuvant pregabalin treatment in laparoscopic cholecystectomy: a randomized, controlled trial. Scand J Pain 19(2):309–317. https://doi.org/10.1515/sjpain-2018-0330
Arif SK, Rawung Y, Musba AMT, Tanra AH (2019) Effect of the perioperative intravenous lidocaine infusion of 1.25 mg/kgBW/H on the bowel sound recovery and pain intensity after laparoscopic cholecystectomy. Eur J Med Health Sci. https://doi.org/10.24018/ejmed.2019.1.1.15
Surender AP, Khurana G, Sachan P (2018) Comparison of postoperative quality of recovery and pain relief with preoperative single-dose dexamethasone and lignocaine after laparoscopic cholecystectomy. Anesth Essays Res 12(3):630. https://doi.org/10.4103/aer.aer_82_18
Bielka K, Kuchyn I, Babych V, Martycshenko K, Inozemtsev O (2018) Dexmedetomidine infusion as an analgesic adjuvant during laparoscopic cholecystectomy: a randomized controlled study. BMC Anesthesiol. https://doi.org/10.1186/s12871-018-0508-6
Zaman M, Chowdhary K, Shah A, Yadav R, Grewal P, Choudhary AK, Bawa A (2018) Injectable tramadol vs diclofenac for postoperative pain management in laparoscopic cholecystectomy surgery: a comparative prospective study. World J Laparosc Surg DVD 11(1):5–7. https://doi.org/10.5005/jp-journals-10033-1325
Tuvayanon W, Silchai P, Sirivatanauksorn Y, Visavajarn P, Pungdok J, Tonklai S, Akaraviputh T (2018) Randomized controlled trial comparing the effects of usual gas release, active aspiration, and passive-valve release on abdominal distension in patients who have undergone laparoscopic cholecystectomy. Asian J Endosc Surg 11(3):212–219. https://doi.org/10.1111/ases.12451
Song X, Sun Y, Zhang X, Li T, Yang B (2017) Effect of perioperative intravenous lidocaine infusion on postoperative recovery following laparoscopic cholecystectomy: a randomized controlled trial. Int J Surg 45:8–13. https://doi.org/10.1016/j.ijsu.2017.07.042
Medina-Vera AJ, Novoa LM (2017) Disminución de los requerimientos anestésicos y analgésicos postoperatorios, en pacientes sometidos a colecistectomía laparoscópica: premedicación con paracetamol versus ketorolaco intravenoso, un estudio aleatorizado y doble ciego. Rev Esp Anestesiol Reanim 64(2):64–70. https://doi.org/10.1016/j.redar.2016.05.007
Eidy M, Fazel MR, Abdolrahimzadeh H, Moravveji AR, Kochaki E, Mohammadzadeh M (2017) Effects of pregabalin and gabapentin on postoperative pain and opioid consumption after laparoscopic cholecystectomy. Korean J Anesthesiol 70(4):434–438. https://doi.org/10.4097/kjae.2017.70.4.434
Kim EM, Jeon JH, Chung MH, Choi EM, Baek SH, Jeon PH, Lee MH (2017) The effect of nefopam infusion during laparascopic cholecystectomy on postoperative pain. Int J Med Sci 14(6):570–577. https://doi.org/10.7150/ijms.19021
Vaswani JP, Debata D, Vyas V, Pattil S (2017) Comparative study of the effect of dexmedetomidine vs. fentanyl on haemodynamic response in patients undergoing elective laparoscopic surgery. J Clin Diagn Res 11(9):UC04–UC08. https://doi.org/10.7860/JCDR/2017/27020.10578
Choi SK, Yoon MH, Il CJ, Kim WM, Heo BH, Park KS, Song JA (2016) Comparison of effects of intraoperative nefopam and ketamine infusion on managing postoperative pain after laparoscopic cholecystectomy administered remifentanil. Korean J Anesthesiol 69(5):480–486. https://doi.org/10.4097/kjae.2016.69.5.480
Anil A, Kaya FN, Yavaşcaoǧlu B, Mercanoǧlu Efe E, Türker G, Demirci A (2016) Comparison of postoperative analgesic efficacy of intraoperative single-dose intravenous administration of dexketoprofen trometamol and diclofenac sodium in laparoscopic cholecystectomy. J Clin Anesth 32:127–133. https://doi.org/10.1016/j.jclinane.2016.02.020
Mishra R, Tripathi M, Chandola H (2016) Comparative clinical study of gabapentin and pregabalin for postoperative analgesia in laparoscopic cholecystectomy. Anesth Essays Res 10(2):201. https://doi.org/10.4103/0259-1162.176409
Bandey S, Singh V (2016) Comparison between IV paracetamol and tramadol for postoperative analgesia in patients undergoing laparoscopic cholecystectomy. J Clin Diagn Res 10(8):5–9. https://doi.org/10.7860/JCDR/2016/21021.8274
Lin S, Hua J, Xu B, Yang T, He Z, Xu C, Meng H, Zhou B, Song Z (2015) Comparison of bupivacaine and parecoxib for postoperative pain relief after laparoscopic cholecystectomy: a randomized controlled trial. Int J Clin Exp Med 8(8):13824–13829
Mohtadi A, Nesioonpour S, Salari A, Akhondzadeh R, Rad BM, Aslani SMM (2014) The effect of single-dose administration of dexamethasone on postoperative pain in patients undergoing laparoscopic cholecystectomy. Anesth Pain Med. https://doi.org/10.5812/aapm.17872
Yang SY, Kang H, Choi GJ, Shin HY, Baek CW, Jung YH, Choi YS (2014) Efficacy of intraperitoneal and intravenous lidocaine on pain relief after laparoscopic cholecystectomy. J Int Med Res 42(2):307–319. https://doi.org/10.1177/0300060513505493
Ural SG, Yener O, Sahin H, Simsek T, Aydinli B, Ozgok A (2014) The comparison of analgesic effects of various administration methods of diclofenac sodium, transdermal, oral and intramuscular, in early postoperative period in laparoscopic cholecystectomy operations. Pak J Med Sci 30(1):96–100. https://doi.org/10.12669/pjms.301.4140
Hosseini H, Samaei A, Zare M, Abdollahi M, Rahimianfar A, Dehghan-Tezerjani M (2013) Study of the effect of intra-abdominal lidocaine on postoperative abdominal and scapular pain in elective laparoscopic cholecystectomy candidates. J Biol Today’s World. https://doi.org/10.15412/j.jbtw.01020503
Kocman IB, Krobot R, Premuzić J, Kocman I, Stare R, Katalinić L, Basić-Jukić N (2013) The effect of preemptive intravenous low-dose magnesium sulfate on early postoperative pain after laparoscopic cholecystectomy. Acta Clin Croat 52(3):289–294
Sinha SP, Sinha S, Sharma SC, Jain S, Hai A (2013) Efficacy of Tramadol V/s Diclofenac in Management of Post Laparoscopic Cholecystectomy Pain. Int J Sci Study 1(3):89–94
Gousheh SM, Nesioonpour S, Foroosh FJ, Akhondzadeh R, Sahafi SA, Alizadeh Z (2013) Intravenous paracetamol for postoperative analgesia in laparoscopic cholecystectomy. Anesth Pain Med 3(1):214–218. https://doi.org/10.5812/aapm.9880
Nesek-Adam V, Grizelj-Stojčić E, Mršić V, Rašić Ž, Schwarz D (2012) Preemptive Use of Diclofenac in Combination With Ketamine in Patients Undergoing Laparoscopic Cholecystectomy. Surg Laparosc Endosc Percutan Tech 22(3):232–238. https://doi.org/10.1097/SLE.0b013e31824f8ae4
Mentes O, Harlak A, Yigit T, Balkan A, Balkan M, Cosar A, Savaser A, Kozak O, Tufan T (2008) Effect of intraoperative magnesium sulphate infusion on pain relief after laparoscopic cholecystectomy. Acta Anaesthesiol Scand 52(10):1353–1359. https://doi.org/10.1111/j.1399-6576.2008.01816.x
Rafiqul Hasan Khan M, Zohirul Islam M, Sazzad Hossain M, Aziz L, Samad Choudhury S (2007) Comparison of pre-emptive use of diclofenac, ketorolac and tramadol for post-operative pain in laparoscopic cholecystectomy
Boccara G, Chaumeron A, Pouzeratte Y, Mann C (2005) The preoperative administration of ketoprofen improves analgesia after laparoscopic cholecystectomy in comparison with propacetamol or postoperative ketoprofen. Br J Anaesth 94(3):347–351. https://doi.org/10.1093/bja/aei056
Jabbour-Khoury SI, Dabbous AS, Gerges FJ, Azar MS, Ayoub CM, Khoury GS (2005) Intraperitoneal and intravenous routes for pain relief in laparoscopic cholecystectomy. JSLS 9(3):316–321
Bharti N, Kumar P, Bala I, Gupta V (2011) The efficacy of a novel approach to transversus abdominis plane block for postoperative analgesia after colorectal surgery. Anesth Analg 112(6):1504–1508. https://doi.org/10.1213/ANE.0b013e3182159bf8
Conaghan P, Maxwell-Armstrong C, Bedforth N, Gornall C, Baxendale B, Hong LL, Carty HM, Acheson AG (2010) Efficacy of transversus abdominis plane blocks in laparoscopic colorectal resections. Surg Endosc 24(10):2480–2484. https://doi.org/10.1007/s00464-010-0989-y
Alsharari AF, Abuadas FH, Alnassrallah YS, Salihu D (2022) Transversus abdominis plane block as a strategy for effective pain management in patients with pain during laparoscopic cholecystectomy: a systematic review. J Clin Med 11:6896
Nair P, Behera CR, Patra RK, Shekar N, Rao LS, Pujari P, Panda B, Mishra A (2022) Efficacy and cost-effectiveness of laparoscopic transversus abdominis plane (TAP) block in laparoscopic cholecystectomy: a comparison with the non-TAP group. Cureus. https://doi.org/10.7759/cureus.32038
Suma S, Suresh MV, Nikhil M, Sreeramulu PN (2019) Intra-peritoneal bupivacaine instillation for post-operative pain relief after laparoscopic cholecystectomy: a prospective study. Int J Contemp Surg 7(2):108. https://doi.org/10.5958/2321-1024.2019.00033.3
Paganelli MA, Popescu GK (2015) Actions of bupivacaine, a widely used local anesthetic, on NMDA receptor responses. J Neurosci 35(2):831–842. https://doi.org/10.1523/JNEUROSCI.3578-14.2015
Groudine SB, Fisher HAG, Kaufman RP, Patel MK, Wilkins LJ, Mehta SA, Lumb PD (1998) Intravenous lidocaine speeds the return of bowel function, decreases postoperative pain, and shortens hospital stay in patients undergoing radical retropubic prostatectomy. Anesth Analg 86(2):235–239. https://doi.org/10.1097/00000539-199802000-00003
Vigneault L, Turgeon AF, Côté D, Lauzier F, Zarychanski R, Moore L, McIntyre LA, Nicole PC, Fergusson DA (2011) Perioperative intravenous lidocaine infusion for postoperative pain control: a meta-analysis of randomized controlled trials. Can J Anesth 58(1):22–37. https://doi.org/10.1007/s12630-010-9407-0
Gammaitoni AR, Alvarez NA, Galer BS (2003) Safety and tolerability of the lidocaine patch 5%, a targeted peripheral analgesic: a review of the literature. J Clin Pharmacol 43:111–117
Onuţu AH (2015) Duloxetine, an antidepressant with analgesic properties - a preliminary analysis. Rom J Anaesth Intensive Care 22(2):123–128
Yuan M, Tang T, Ding Z, Li H, Zhou Z (2022) Analgesic effect of perioperative duloxetine in patients after total knee arthroplasty: a prospective, randomized, double-blind, placebo-controlled trial. BMC Musculoskelet Disord. https://doi.org/10.1186/s12891-022-05194-z
Lunn MP, Hughes RA, Wiffen PJ (2014) Duloxetine for treating painful neuropathy, chronic pain or fibromyalgia. Cochrane Database Syst Rev 2015(10). https://doi.org/10.1002/14651858.CD007115.pub3
Altiparmak B, Güzel Ç, Demirbilek SG (2018) Comparison of preoperative administration of pregabalin and duloxetine on cognitive functions and pain management after spinal surgery. Clin J Pain 34(12):1114–1120. https://doi.org/10.1097/AJP.0000000000000640
Ho KY, Tay W, Yeo MC, Liu H, Yeo SJ, Chia SL, Lo NN (2010) Duloxetine reduces morphine requirements after knee replacement surgery. Br J Anaesth 105(3):371–376. https://doi.org/10.1093/bja/aeq158
Zorrilla-Vaca A, Stone A, Caballero-Lozada AF, Paredes S, Grant MC (2019) Perioperative duloxetine for acute postoperative analgesia: a meta-analysis of randomized trials. Reg Anesth Pain Med 44(10):959–965. https://doi.org/10.1136/rapm-2019-100687
Stahl SM, Porreca F, Taylor CP, Cheung R, Thorpe AJ, Clair A (2013) The diverse therapeutic actions of pregabalin: is a single mechanism responsible for several pharmacological activities? Trends Pharmacol Sci 34:332–339
Zhang D, You G, Yao X (2020) Influence of pregabalin on post-operative pain after laparoscopic cholecystectomy: a meta-analysis of randomised controlled trials. J Minim Access Surg 16:99–105
Zhang Y, Wang Y, Zhang X (2017) Effect of pre-emptive pregabalin on pain management in patients undergoing laparoscopic cholecystectomy: a systematic review and meta-analysis. Int J Surg 44:122–127
Gonano C, Latzke D, Sabeti-Aschraf M, Kettner SC, Chiari A, Gustorff B (2011) The anxiolytic effect of pregabalin in outpatients undergoing minor orthopaedic surgery. J Psychopharmacol 25(2):249–253. https://doi.org/10.1177/0269881109106928
Mitra S, Khandelwal P, Roberts K, Kumar S, Vadivelu N (2012) Pain relief in laparoscopic cholecystectomy: a review of the current options. Pain Pract 12:485–496
Agarwal A, Gautam S, Gupta D, Agarwal S, Singh PK, Singh U (2008) Evaluation of a single preoperative dose of pregabalin for attenuation of postoperative pain after laparoscopic cholecystectomy. Br J Anaesth 101(5):700–704. https://doi.org/10.1093/bja/aen244
Abdelmageed WM, Al Taher WM (2014) Preoperative paracetamol infusion reduces sevoflurane consumption during thyroidectomy under general anesthesia with spectral entropy monitoring. Egypt J Anaesth 30(2):115–122. https://doi.org/10.1016/j.egja.2013.12.003
Oscier CD, Milner QJW (2009) Peri-operative use of paracetamol. Anaesthesia 64:65–72
Ohnesorge H, Bein B, Hanss R, Francksen H, Mayer L, Scholz J, Tonner PH (2009) Paracetamol versus metamizol in the treatment of postoperative pain after breast surgery: a randomized, controlled trial. Eur J Anaesthesiol 26(8):648–653. https://doi.org/10.1097/EJA.0b013e328329b0fd
Moller PL, Sindet-Pedersen S, Petersen CT, Juhl GI, Dillenschneider A, Skoglund LA (2005) Onset of acetaminophen analgesia: comparison of oral and intravenous routes after third molar surgery. Br J Anaesth 94(5):642–648. https://doi.org/10.1093/bja/aei109
Pandit MK, Godhi S, Lall AB (2011) Preoperative intravenous tramadol versus diclofenac for preventing postoperative pain after third molar surgery: a comparative study. J Maxillofac Oral Surg 10(4):306–309. https://doi.org/10.1007/s12663-011-0250-9
Altman R, Bosch B, Brune K, Patrignani P, Young C (2015) Advances in NSAID development: evolution of diclofenac products using pharmaceutical technology. Drugs 75:859–877
Patel RV (2020) Comparative effects of intravenous diclofenac versus intramuscular diclofenac on postoperative surgical pain management. MedPulse Int J Anesthesiol 15(1):15–19. https://doi.org/10.26611/10151514
Predel HG, Koll R, Pabst H, Dieter R, Gallacchi G, Giannetti B, Bulitta M, Heidecker JL, Mueller EA (2004) Diclofenac patch for topical treatment of acute impact injuries: a randomised, double blind, placebo controlled, multicentre study. Br J Sports Med 38(3):318–323. https://doi.org/10.1136/bjsm.2003.005017
Adarsh ES, Mane R, Sanikop CS, Sagar SM (2012) Effect of pre-operative rectal diclofenac suppository on post-operative analgesic requirement in cleft palate repair: a randomised clinical trial. Indian J Anaesth 56(3):265–269. https://doi.org/10.4103/0019-5049.98774
Porażka J, Szałek E, Żółtaszek W, Grabowski T, Wolc A, Grześkowiak E (2020) Influence of obesity on pharmacokinetics and analgesic effect of ketoprofen administered intravenously to patients after laparoscopic cholecystectomy. Pharmacol Rep 72(3):763–768. https://doi.org/10.1007/s43440-019-00042-9
Sarzi- Puttini P, Atzeni F, Lanata L, Bagnasco M, Colombo M, Fischer F, D’Imporzano M (2011) Pain and ketoprofen: what is its role in clinical practice? Reumatismo 62(3). https://doi.org/10.4081/reumatismo.2010.172
Krawczyk M, Wordliczek J, Czupryna A, Dobrogowski J, Dobosz M, Gaszyński W, Andziak P, Misiołek H, Dziki A (2012) The recommendations for perioperative pain relief in general surgery. Pol Przegl Chir 84(9):476–484. https://doi.org/10.2478/v10035-012-0081-5
Moon JY, Choi SS, Lee SY, Lee MK, Kim JE, Lee JE, Lee SH (2016) The effect of nefopam on postoperative fentanyl consumption: a randomized, double-blind study. Korean J Pain 29(2):110–118. https://doi.org/10.3344/kjp.2016.29.2.110
Kim KH, Abdi S (2014) Rediscovery of nefopam for the treatment of neuropathic pain. Korean J Pain 27:103–111
Alfonsi P, Adam F, Passard A, Guignard B, Sessler DI, Chauvin M (2004) Nefopam, a nonsedative benzoxazocine analgesic, selectively reduces the shivering threshold in unanesthetized subjects. Anesthesiology 100(1):37–43. https://doi.org/10.1097/00000542-200401000-00010
Kakkar M, Derry S, Moore RA, McQuay HJ (2009) Single dose oral nefopam for acute postoperative pain in adults. Cochrane Database Syst Rev 2019(5). https://doi.org/10.1002/14651858.CD007442.pub2
Fernández-Sánchez MT, Díaz-Trelles R, Groppetti A, Manfredi B, Brini AT, Biella G, Sotgiu ML, Novelli A (2002) Nefopam, an analogue of orphenadrine, protects against both NMDA receptor-dependent and independent veratridine-induced neurotoxicity. Amino Acids 23(1–3):31–36. https://doi.org/10.1007/s00726-001-0106-6
Verleye M, André N, Heulard I, Gillardin JM (2004) Nefopam blocks voltage-sensitive sodium channels and modulates glutamatergic transmission in rodents. Brain Res 1013(2):249–255. https://doi.org/10.1016/j.brainres.2004.04.035
Novelli A, Díaz-Trelles R, Groppetti A, Fernández-Sánchez MT (2005) Nefopam inhibits calcium influx, cGMP formation, and NMDA receptor-dependent neurotoxicity following activation of voltage sensitive calcium channels. In: Amino acids, pp 183–191
Evans MS, Lysakowski C, Tramèr MR (2008) Nefopam for the prevention of postoperative pain: quantitative systematic review. Br J Anaesth 101:610–617
Yoon JU, Byeon GJ, Cheon JH, Choi YM, Ri HS, Baik SW (2016) Post-operative intravenous patientcontrolled analgesic efficacy of morphine with ketorolac versus nefopam after laparoscopic gynecologic surgery: a randomized non-inferiority trial. Korean J Anesthesiol 69(2):161–166. https://doi.org/10.4097/kjae.2016.69.2.161
Na HS, Oh AY, Ryu JH, Koo BW, Nam SW, Jo J, Park JH (2018) Intraoperative nefopam reduces acute postoperative pain after laparoscopic gastrectomy: a prospective, randomized study. J Gastrointest Surg 22(5):771–777. https://doi.org/10.1007/s11605-018-3681-5
Lim H, Kang S, Kim B, Ko S (2019) Comparison between preoperative and intraoperative administration of nefopam for acute and chronic postoperative pain in colon cancer patients: a prospective, randomized, double-blind study. World J Surg 43(12):3191–3197. https://doi.org/10.1007/s00268-019-05119-3
Du Manoir B, Aubrun F, Langlois M, Le Guern ME, Alquier C, Chauvin M, Fletcher D (2003) Randomized prospective study of the analgesic effect of nefopam after orthopaedic surgery. Br J Anaesth 91(6):836–841. https://doi.org/10.1093/bja/aeg264
McLintock TT, Kenny GN, Howie JC, McArdle CS, Lawrie S, Aitken H (1988) Assessment of the analgesic efficacy of nefopam hydrochloride after upper abdominal surgery: a study using patient controlled analgesia. Br J Surg 75(8):779–781. https://doi.org/10.1002/bjs.1800750818
Na HS, Oh AY, Koo BW, Lim DJ, Ryu JH, Han JW (2016) Preventive analgesic efficacy of nefopam in acute and chronic pain after breast cancer surgery. Medicine. https://doi.org/10.1097/MD.0000000000003705
Yoo JY, Lim BG, Kim H, Kong MH, Lee IO, Kim NS (2015) The analgesic effect of nefopam combined with low dose remifentanil in patients undergoing middle ear surgery under desflurane anesthesia: a randomized controlled trial. Korean J Anesthesiol 68(1):43–49. https://doi.org/10.4097/kjae.2015.68.1.43
Valverde A, Skelding AM (2019) Alternatives to opioid analgesia in small animal anesthesia: alpha-2 agonists. Vet Clin N Am Small Anim Practice 49:1013–1027
Kalaskar V, Ruparel D, Wakode R (2021) Effects of dexmedetomidine infusion in low dose on dose reduction of propofol, intraoperative hemodynamics, and postoperative analgesia in patients undergoing laparoscopic cholecystectomy. Anesth Essays Res 15(4):391. https://doi.org/10.4103/aer.aer_123_21
Weerink MAS, Struys MMRF, Hannivoort LN, Barends CRM, Absalom AR, Colin P (2017) Clinical pharmacokinetics and pharmacodynamics of dexmedetomidine. Clin Pharmacokinet 56:893–913
Ge DJ, Qi B, Tang G, Li JY (2015) Intraoperative dexmedetomidine promotes postoperative analgesia and recovery in patients after abdominal colectomy: a CONSORT-prospective, randomized, controlled clinical trial. Medicine. https://doi.org/10.1097/MD.0000000000001727
Bekker A, Haile M, Kline R, Didehvar S, Babu R, Martiniuk F, Urban M (2013) The effect of intraoperative infusion of dexmedetomidine on the quality of recovery after major spinal surgery. J Neurosurg Anesthesiol 25(1):16–24. https://doi.org/10.1097/ANA.0b013e31826318af
Laskowski K, Stirling A, McKay WP, Lim HJ (2011) A systematic review of intravenous ketamine for postoperative analgesia. Can J Anesth 58:911–923
Singh H, Kundra S, Singh RM, Grewal A, Kaul TK, Sood D (2013) Preemptive analgesia with ketamine for laparoscopic cholecystectomy. J Anaesthesiol Clin Pharmacol 29(4):478–484. https://doi.org/10.4103/0970-9185.119141
Naghibi K, Kashefi P, Abtahi AM (2013) The comparison of preemptive effects of propofol, remifentanil and ketamine on post-operative pain scores and analgesic requirements in elective lower abdominal surgery under general anesthesia: A randomized, double-blinded study. J Res Med Sci 18(7):567–572
Buvanendran A, Kroin JS (2008) Early use of memantine for neuropathic pain. Anesth Analg 107:1093–1094
Parsons CG, Danysz W, Quack G (1999) Memantine is a clinically well tolerated N-methyl-D-aspartate (NMDA) receptor antagonist-a review of preclinical data
Pickering G, Morel V (2018) Memantine for the treatment of general neuropathic pain: a narrative review. Fundam Clin Pharmacol 32:4–13
Carlton SM, Hargett GL, Coggeshall RE (1995) Localization and activation of glutamate receptors in unmyelinated axons of rat glabrous skin. Neurosci Lett 197(1):25–28. https://doi.org/10.1016/0304-3940(95)11889-5
Petrenko AB, Yamakura T, Baba H, Shimoji K (2003) The role of N-methyl-D-aspartate (NMDA) receptors in pain: a review. Anesth Analg 97:1108–1116
Bennett GJ (2000) Update on the Neurophysiology of Pain Transmission and Modulation. J Pain Symptom Manage 19(1):2–6. https://doi.org/10.1016/S0885-3924(99)00120-7
Berrino L, Oliva P, Massimo F, Aurilio C, Maione S, Grella A, Rossi F (2003) Antinociceptive effect in mice of intraperitoneal N-methyl-D-aspartate receptor antagonists in the formalin test. Europ J Pain 7(2):131–137. https://doi.org/10.1016/S1090-3801(02)00086-1
Suzuki M (2009) Role of N-methyl-D-aspartate receptor antagonists in postoperative pain management. Curr Opin Anaesthesiol 22:618–622
Morel V, Joly D, Villatte C, Dubray C, Durando X, Daulhac L, Coudert C, Roux D, Pereira B, Pickering G (2016) Memantine before mastectomy prevents post-surgery pain: a randomized, blinded clinical trial in surgical patients. PLoS ONE. https://doi.org/10.1371/journal.pone.0152741
Rahimzadeh P, Imani F, Nikoubakht N, Koleini Z, Faiz SHR, Sayarifard A (2017) A comparative study on the efficacy of oral memantine and placebo for acute postoperative pain in patients undergoing dacryocystorhinostomy (DCR). Anesth Pain Med. https://doi.org/10.5812/aapm.45297
Morel V, Etienne M, Wattiez AS, Dupuis A, Privat AM, Chalus M, Eschalier A, Daulhac L, Pickering G (2013) Memantine, a promising drug for the prevention of neuropathic pain in rat. Eur J Pharmacol 721(1–3):382–390. https://doi.org/10.1016/j.ejphar.2013.06.020
Schley M, Topfner S, Wiech K, Schaller HE, Konrad CJ, Schmelz M, Birbaumer N (2007) Continuous brachial plexus blockade in combination with the NMDA receptor antagonist memantine prevents phantom pain in acute traumatic upper limb amputees. Eur J Pain 11(3):299–308. https://doi.org/10.1016/j.ejpain.2006.03.003
Paoletti P, Neyton J (2007) NMDA receptor subunits: function and pharmacology. Curr Opin Pharmacol 7:39–47
Woolf CJ, Thompson SWN (1991) Basic section the induction and maintenance of central sensitization is dependent on N-methyl-D-aspartic acid receptor activation; implications for the treatment of post-injury pain hypersensitivity states. Elscvier, Hoboken
Dolati S, Rikhtegar R, Mehdizadeh A, Yousefi M (2020) The role of magnesium in pathophysiology and migraine treatment. Biol Trace Elem Res 196:375–383
Yaralizadeh M, Nezamivand-Chegini S, Najar S, Namjoyan F, Abedi P (2021) Effectiveness of magnesium on menstrual symptoms among dysmenorrheal college students: a randomized controlled trial. Int J Women’s Health Reprod Sci X. https://doi.org/10.1529/ijwhr.2023.25
Farsi L, Afshari K, Keshavarz M, NaghibZadeh M, Memari F, Norouzi-Javidan A (2015) Postinjury treatment with magnesium sulfate attenuates neuropathic pains following spinal cord injury in male rats. Behav Pharmacol 26(3):315–320. https://doi.org/10.1097/FBP.0000000000000103
Engen DJ, McAllister SJ, Whipple MO, Cha SS, Dion LJ, Vincent A, Bauer BA, Wahner-Roedler DL (2015) Effects of transdermal magnesium chloride on quality of life for patients with fibromyalgia: a feasibility study. J Integr Med 13(5):306–313. https://doi.org/10.1016/S2095-4964(15)60195-9
Ozcan PE, Tugrul S, Senturk NM, Uludag E, Cakar N, Telci L, Esen F (2007) Role of magnesium sulfate in postoperative pain management for patients undergoing thoracotomy. J Cardiothorac Vasc Anesth 21(6):827–831. https://doi.org/10.1053/j.jvca.2006.11.013
Taheri A, Haryalchi K, Mansour Ghanaie M, Habibi Arejan N (2015) Effect of low-dose (single-dose) magnesium sulfate on postoperative analgesia in hysterectomy patients receiving balanced general anesthesia. Anesthesiol Res Pract. https://doi.org/10.1155/2015/306145
El Mourad M, Arafa S (2019) Effect of intravenous versus intraperitoneal magnesium sulfate on hemodynamic parameters and postoperative analgesia during laparoscopic sleeve gastrectomy: a prospective randomized study. J Anaesthesiol Clin Pharmacol 35(2):242–247. https://doi.org/10.4103/joacp.JOACP_208_18
Jerkovic D, Tadin A, Gavic L, Vladislavic NZ, Grgic N, Macan D (2020) Effect of orally administered magnesium on postoperative pain level and trismus after surgical removal of the lower third molars: a randomized, double-blind, placebo-controlled trial. Clin Oral Investig 24(12):4649–4659. https://doi.org/10.1007/s00784-020-03335-z
Albrecht E, Kirkham KR, Liu SS, Brull R (2013) Peri-operative intravenous administration of magnesium sulphate and postoperative pain: a meta-analysis. Anaesthesia 68:79–90
Yan Q, Guo B-L, Lin Y, Hu W, Zhen C-X, Bao-Cheng Z, Wu H-H, Kaye AD, Duan J-H, Qu Y (2015) Systematic review effects of systemic magnesium on post-operative analgesia: is the current evidence strong enough? Pain Phys 18:405–417
Peng YN, Sung FC, Huang ML, Lin CL, Kao CH (2018) The use of intravenous magnesium sulfate on postoperative analgesia in orthopedic surgery. A systematic review of randomized controlled trials. Medicine (United States) 97:e13583
Kehlet H, Lindberg-Larsen V (2018) High-dose glucocorticoid before hip and knee arthroplasty: to use or not to use—that’s the question. Acta Orthop 89(5):477–479. https://doi.org/10.1080/17453674.2018.1475177
Gan TJ, Belani KG, Bergese S, Chung F, Diemunsch P, Habib AS, Jin Z, Kovac AL, Meyer TA, Urman RD, Apfel CC, Ayad S, Beagley L, Candiotti K, Englesakis M, Hedrick TL, Kranke P, Lee S, Lipman D, Minkowitz HS, Morton J, Philip BK (2020) Fourth consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg 131(2):411–448. https://doi.org/10.1213/ANE.0000000000004833
De Oliveira GS, Almeida MD, Benzon HT, McCarthy RJ (2011) Perioperative single dose systemic dexamethasone for postoperative pain: a meta-analysis of randomized controlled trials. Anesthesiology 115(3):575–588. https://doi.org/10.1097/ALN.0b013e31822a24c2
Waldron NH, Jones CA, Gan TJ, Allen TK, Habib AS (2013) Impact of perioperative dexamethasone on postoperative analgesia and side-effects: systematic review and meta-analysis. Br J Anaesth 110:191–200
O’Hare PE, Wilson BJ, Loga MG, Ariyawardana A (2019) Effect of submucosal dexamethasone injections in the prevention of postoperative pain, trismus, and oedema associated with mandibular third molar surgery: a systematic review and meta-analysis. Int J Oral Maxillofac Surg 48:1456–1469
Mathiesen O, Jacobsen LS, Holm HE, Randall S, Adamiec-Malmstroem L, Graungaard BK, Holst PE, Hilsted KL, Dahl JB (2008) Pregabalin and dexamethasone for postoperative pain control: a randomized controlled study in hip arthroplasty. Br J Anaesth 101(4):535–541. https://doi.org/10.1093/bja/aen215
Gayam S, Naduvinakeri K, Rajagopal M, Neelima C (2020) Preoperative dexamethasone and intraperitoneal bupivacaine for postoperative pain relief. Obsgyne Rev J Obstet Gynecol 6(4):96–101. https://doi.org/10.17511/joog.2020.i04.05
Gul G, Bilgic T, Aydin MA (2020) Evaluation of the effects of preoperative dexamethasone administration on postoperative patient comfort in laparoscopic cholecystectomy. Cureus. https://doi.org/10.7759/cureus.7968
Christidis N, Kang I, Cairns BE, Kumar U, Dong X, Rosén A, Kopp S, Ernberg M (2014) Expression of 5-HT3 receptors and TTX resistant sodium channels (NaV1.8) on muscle nerve fibers in pain-free humans and patients with chronic myofascial temporomandibular disorders. J Headache Pain. https://doi.org/10.1186/1129-2377-15-63
Costall B, Naylor R (2004) 5-HT3 Receptors. Current Drug Target -CNS & Neurological Disorders 3(1):27–37. https://doi.org/10.2174/1568007043482624
Ye JH, Mui WC, Ren J, Hunt TE, Wu W-H, Zbuzek VK (1997) Ondansetron exhibits the properties of a local anesthetic. Anesth Analg 85(5):1116–1121. https://doi.org/10.1097/00000539-199711000-00029
Roczniak W, Wróbel J, Dolczak L, Nowak P (2013) Influence of central noradrenergic system lesion on the serotoninergic 5-HT3 receptor mediated analgesia in rats. Adv Clin Exp Med 22(5):629–638
Kovac AL (2018) Updates in the management of postoperative nausea and vomiting. Adv Anesth 36:81–97
Ambesh SP, Dubey PK, Sinha PK (1999) Ondansetron pretreatment to alleviate pain on propofol injection. Anesth Analg 89(1):197–199. https://doi.org/10.1097/00000539-199907000-00035
Reddy MS, Chen FG, Ng HP (2001) Effect of ondansetron pretreatment on pain after rocuronium and propofol injection: a randomised, double-blind controlled comparison with lidocaine. Anaesthesia 56(9):902–905. https://doi.org/10.1046/j.1365-2044.2001.02059-6.x
Rahimzadeh P, Faiz SR, Nikoobakht N, Ghodrati M (2015) Which one is more efficient on propofol 2% injection pain? Magnesium sulfate or ondansetron: a randomized clinical trial. Adv Biomed Res 4(1):56. https://doi.org/10.4103/2277-9175.151593
McCleane GJ, Suzuki R, Dickenson AH (2003) Does a single intravenous injection of the 5HT3 receptor antagonist ondansetron have an analgesic effect in neuropathic pain? A double-blinded, placebo-controlled cross-over study. Anesth Analg 97(5):1474–1478. https://doi.org/10.1213/01.ANE.0000085640.69855.51
Wasinwong W, Termthong S, Plansangkate P, Tanasansuttiporn J, Kosem R, Chaofan S (2022) A comparison of ondansetron and lidocaine in reducing injection pain of propofol: a randomized controlled study. BMC Anesthesiol. https://doi.org/10.1186/s12871-022-01650-4
Zaazouee MS, Mahmoud AM, Elfar WH, Hana K, Shamshoon KF, Adly MH, Hussein TA, Hamza MM, Aly AA, Eguzo MA, Farhat AM, Elsnhory AB, Morsy MH, Ammar MF, Alnaji AA, Elshanbary AA, Shah J, Abdelqadir YH (2023) Effect of ondansetron compared to lidocaine and placebo for reducing propofol injection pain: a systematic review and meta-analysis of randomized controlled trials. Medicine (United States) 102(38):E35021. https://doi.org/10.1097/MD.0000000000035021
Jokela R, Ahonen J, Seitsonen E, Marjakangas P, Korttila K (2010) The influence of ondansetron on the analgesic effect of acetaminophen after laparoscopic hysterectomy. Clin Pharmacol Ther 87(6):672–678. https://doi.org/10.1038/clpt.2009.281
Macor JE, Gurley D, Lanthorn T, Loch J, Mack RA, Mullen G, Tran O, Wright N, Gordon JC (2001) The 5-HT 3 antagonist tropisetron (ICS 205-930) is a potent and selective α7 nicotinic receptor partial agonist. Bioorg Med Chem Lett 11(3):319–321. https://doi.org/10.1016/S0960-894X(00)00670-3
Liu, J., Liu, M., Shi, S., Jiang, F., Zhang, Y., Guo, J., & Gong, X. (2024). Evaluation of the effect of intraoperative tropisetron on postoperative rebound pain after brachial plexus block: A randomized controlled trial. Pain Reports 9(3):E1163. https://doi.org/10.1097/PR9.0000000000001163
Yuan W, Wang Q, Chen X (2019) Perioperative acupuncture medicine: a novel concept instead of acupuncture anesthesia. Chin Med J (Engl) 132(6):707–715. https://doi.org/10.1097/CM9.0000000000000123
Coutaux A (2017) Non-pharmacological treatments for pain relief: TENS and acupuncture. Joint Bone Spine 84:657–661
Lin CWC, Haas M, Maher CG, MacHado LAC, Van Tulder MW (2011) Cost-effectiveness of guideline-endorsed treatments for low back pain: a systematic review. Eur Spine J 20:1024–1038
Yamashita H, Ac L, Tsukayama H, Tanno Y, Nishijo K, Ac L (1999) Adverse events in acupuncture and moxibustion treatment: a six-year survey at a national clinic in Japan. Mary Ann Liebert Inc, New York
Lee J-H, Choi T-Y, Lee MS, Lee H, Shin B-C, Lee H (2013) Acupuncture for Acute Low Back Pain. Clin J Pain 29(2):172–185. https://doi.org/10.1097/AJP.0b013e31824909f9
Chen J, Zhang Y, Li X, Wan Y, Ji X, Wang W, Kang X, Yan W, Fan Z (2020) Efficacy of transcutaneous electrical acupoint stimulation combined with general anesthesia for sedation and postoperative analgesia in minimally invasive lung cancer surgery: a randomized, double-blind, placebo-controlled trial. Thorac Cancer 11(4):928–934. https://doi.org/10.1111/1759-7714.13343
Chen CC, Yang CC, Hu CC, Shih HN, Chang YH, Hsieh PH (2015) Acupuncture for pain relief after total knee arthroplasty: a randomized controlled trial. Reg Anesth Pain Med 40(1):31–36. https://doi.org/10.1097/AAP.0000000000000138
Cho YH, Kim CK, Heo KH, Lee MS, Ha IH, Son DW, Choi BK, Song GS, Shin BC (2015) Acupuncture for acute postoperative pain after back surgery: a systematic review and meta-analysis of randomized controlled trials. Pain Pract 15:279–291
Yeh ML, Tsou MY, Lee BY, Chen HH, Chung YC (2010) Effects of auricular acupressure on pain reduction in patient-controlled analgesia after lumbar spine surgery. Acta Anaesthesiol Taiwan 48(2):80–86. https://doi.org/10.1016/S1875-4597(10)60018-5
Jackson SA (1996) Does post-laparoscopy pain relate to residual carbon dioxide? Anaesthesia 51(5):485–487. https://doi.org/10.1111/j.1365-2044.1996.tb07798.x
Tsai H-W (2011) Maneuvers to decrease laparoscopy-induced shoulder and upper abdominal pain. Arch Surg 146(12):1360. https://doi.org/10.1001/archsurg.2011.597
Atak I, Ozbagriacik M, Akinci OF, Bildik N, Subasi IE, Ozdemir M, Ayta Nİ (2011) Active gas aspiration to reduce pain after laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech 21(2):98–100. https://doi.org/10.1097/SLE.0b013e318213c301
Haneef AK, Aljohani EA, Alzahrani RS, Alowaydhi HM, Alarif GA, Bukhari MM, Abdulhamid AS, AlRajhi B, Ageel AH (2024) Active gas aspiration in reducing pain after laparoscopic cholecystectomy: a systematic review and meta-analysis of randomized controlled trials. Surg Endosc 38:597–606
Lee JS, Kim EY, Lee SH, Han JH, Park SK, Na GH, You YK, Kim DG, Hong TH (2014) A simple method of reducing residual intraperitoneal carbon dioxide after laparoscopic cholecystectomy: a prospective, randomized, controlled study. J Laparoendosc Adv Surg Tech 24:563–566
Fredman B, Jedeikin R, Olsfanger D, Flor P, Gruzman A (1994) Residual pneumoperitoneum: a cause of postoperative pain after laparoscopic cholecystectomy. Anesth Analg 79(1):152–154
Das K, Karateke F, Menekse E, Ozdogan M, Aziret M, Erdem H, Cetinkunar S, Ozdogan H, Sozen S (2013) Minimizing shoulder pain following laparoscopic cholecystectomy: a prospective, randomized, controlled trial. J Laparoendosc Adv Surg Tech 23(3):179–182. https://doi.org/10.1089/lap.2012.0410
Bruno RR, Wolff G, Wernly B, Masyuk M, Piayda K, Leaver S, Erkens R, Oehler D, Afzal S, Heidari H, Kelm M, Jung C (2022) Virtual and augmented reality in critical care medicine: the patient’s, clinician’s, and researcher’s perspective. Crit Care. https://doi.org/10.1186/s13054-022-04202-x
Smith V, Warty RR, Sursas JA, Payne O, Nair A, Krishnan S, da Silva CF, Wallace EM, Vollenhoven B (2020) The effectiveness of virtual reality in managing acute pain and anxiety for medical inpatients: systematic review. J Med Internet Res 22:e17980
Wismeijer AAJ, Vingerhoets AJJM (2005) The use of virtual reality and audiovisual eyeglass systems as adjunct analgesic techniques: A review of the literature. Annal Behav Med 30(3):268–278. https://doi.org/10.1207/s15324796abm3003_11
Li A, Montaño Z, Chen VJ, Gold JI (2011) Virtual reality and pain management: current trends and future directions. Pain Manag 1(2):147–157. https://doi.org/10.2217/pmt.10.15
Hoffman HG, Patterson DR, Seibel E, Soltani M, Jewett-Leahy L, Sharar SR (2008) Virtual Reality Pain Control During Burn Wound Debridement in the Hydrotank. Clin J Pain 24(4):299–304. https://doi.org/10.1097/AJP.0b013e318164d2cc
Mosso-Vázquez JL, Gao K, Wiederhold BK, Wiederhold MD (2014) Virtual reality for pain management in cardiac surgery. Cyberpsychol Behav Soc Netw 17(6):371–378. https://doi.org/10.1089/cyber.2014.0198
Nilsson S, Finnström B, Kokinsky E, Enskär K (2009) The use of Virtual Reality for needle-related procedural pain and distress in children and adolescents in a paediatric oncology unit. Eur J Oncol Nurs 13(2):102–109. https://doi.org/10.1016/j.ejon.2009.01.003
Mosso Vázquez JL, Mosso Lara D, Mosso Lara JL, Miller I, Wiederhold MD, Wiederhold BK (2019) Pain distraction during ambulatory surgery: virtual reality and mobile devices. Cyberpsychol Behav Soc Netw 22(1):15–21. https://doi.org/10.1089/cyber.2017.0714
Bekelis K, Calnan D, Simmons N, Mackenzie TA, Kakoulides G (2017) Effect of an immersive preoperative virtual reality experience on patient reported outcomes: a randomized controlled trial. Ann Surg 265(6):1068–1073. https://doi.org/10.1097/SLA.0000000000002094
Acknowledgements
None.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
HMB collected, distributed, and organized the datasets and prepared the first draft of the manuscript. NOES and DHA contributed to the conception and design of the study. The final manuscript was revised by ERB, DHA, NOES, and Sherif Boraii. All the authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bayoumi, H.M., Abdelaziz, D.H., El Said, N.O. et al. Postoperative pain management following laparoscopic cholecystectomy-non-opioid approaches: a review. Futur J Pharm Sci 10, 125 (2024). https://doi.org/10.1186/s43094-024-00697-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43094-024-00697-z