Abstract
Background
Chronic knee osteoarthritis (OA) is a frequent disease among the elderly. Intra-articular corticosteroid injection (IACSI) was commonly adopted to alleviate knee OA-related pains. Recently, Genicular nerve block (GNB) has emerged as a new alternative technique. The current study aimed to investigate the efficacy of those two approaches when guided with ultrasound and to determine which one offers better results. This study included 40 patients with painful chronic knee OA (Nine males and 31 females, age ranged from 44 to 65 years) and were randomly assigned to two equal groups. Groups 1 was managed with ultrasound-guided IACSI and group 2 with ultrasound-guided GNB using a mixture of lidocaine and Triamcinolone Acetonide. The baseline mean visual analogue scale (VAS) and Oxford knee score (OKS) for the group 1 were 87.10 and 51.3, while for group 2 were 87.75 and 53.25 respectively. Follow up values were obtained at 2, 4 and 8 weeks using VAS and OKS.
Results
The VAS score and OKS score were significantly lower in the GNB group and IACSI group at 2, and 4 weeks after the procedure (p < 0.001 for all), then returned near baseline values at 8 weeks. When the two groups were compared according to changes in VAS and OKS from baseline at 2, 4, and 8 weeks, GNB group showed significant alleviation of pain (mean reduction of 58.5, 53.3, and 9.25 points at 2, 4, and 8 weeks versus 44.9, 39.4, and 5.6 points at the IACSI groups, p < 0.001 at 2 and 4 weeks, p < 0.006 at 8 weeks). Similarly at the OKS, the GNB group showed significantly better results (33.50, 28.60, and 8.5 at GNB and 26.45, 20.10, 5.25 at IACSI. p < 0.001 at all periods).
Conclusions
Both GNB and IACSI are effective methods to relieve chronic knee osteoarthritis-related pains. When compared to each other, GNB showed more significant pain relief and functional improvement than IACSI.
Similar content being viewed by others
Background
Chronic knee osteoarthritis (OA) is a common disease among elderly, with consequent pain and disability that might hinder their quality of life [1]. Management is usually conservative with light physical activity, weight management, aquatic therapy, acetaminophen and NSAIDs [2,3,4,5].When these measures fail, surgical treatment with total knee joint arthroplasty can be offered [6].
Ultrasound guided Intra-articular corticosteroid injection (IACSI) has immunosuppressive and anti-inflammatory effects by directly acting on the nuclear receptors, interfering with the inflammatory cascade and reducing the production and action of many inflammatory mediators [2, 7].
Ultrasound is used during IACSI to identify the supra-patellar bursa, which can be easily injected with no appreciable risk of extra-articular extravasation or injury to surrounding structures [8].
Ultrasound guided IACSI showed to be useful and viable alternative to reduce knee OA related pain and improve functional capacity mainly on short term bases as evidenced by many studies [9,10,11].
Genicular nerve block (GNB) has recently emerged as an alternative technique with very promising results to reduce OA related pains and improve functional status as evidenced by many recent studies [1, 12, 13]. It’s based on the fact that genicular nerves are accompanied with genicular arteries, which can be easily identified at certain anatomical land marks using ultrasound and confirmed with color Doppler [1].
Ultrasound is considered the best method to evaluate the nerves around the knee [14] and have many advantages as being readily available, accessible and cheaper without radiation hazards [13].
This study aimed to investigate the efficacy of ultrasound guided intra-articular corticosteroid injection and genicular nerve block to control knee OA related symptoms and to compare the results obtained after both techniques.
Methods
Patients
This randomized prospective blinded study was carried out on all consecutive patients with radiologically proven symptomatic knee joint osteoarthritis not responding to medical treatment, referred to the university hospital for pain management from January 2019 to November 2020. The study protocol was approved by the local ethics committee before the start of the study. Radiological severity was assessed using the Kellgren and Lawrence global scale [15] as follow: Grade 0; means absence of radiological finding; grade 1: suspected narrowing of joint space; grade 2 refers to osteophytes and possible narrowing; grade 3 is defined as multiple osteophytes, definite narrowing of joint space and grade 4 comprises large osteophytes, marked narrowing of joint space.
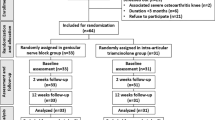
All patients were evaluated by a consultant of physical medicine, rheumatology and rehabilitation. Patients with knee pain of moderate or greater intensity on most or all days for ≥ 3 months, showing significant radiological OA (Kellgren-Lawrence grade 2 to 4) were initially included in the study. Patients with previous knee surgery, acute knee pain, connective tissue diseases affecting the knee joint, sciatic pain, previous intra-articular or peri-articular interventions and those who were lost to follow up to 8 weeks after knee joint injection were excluded. The study included 40 patients and were randomly distributed to two equal groups. Groups 1 was managed with ultrasound-guided IACSI and group 2 with ultrasound-guided GNB. All patients were blinded to the management procedure. Informed written consent to participate in the study was obtained from all participants.
Interventional procedures
All procedures were performed with patients placed in supine position, under complete aseptic conditions and were guided with ultrasound (ACUSON X 300, Siemens Healthineers AG, Erlangen, Germany) using a 10 MHz linear transducer. Single operator with four years’ experience in ultrasound guided interventions performed all the injections. Evaluation of the management response at all follow up periods were assessed by another physician who was blind to the management procedure.
For the GNB group, GNB was carried out using the same technique previously described by Kim et al. [1]. GNB target points for injection were close to the superior lateral, superior medial, and inferior medial genicular arteries that were identified near the periosteal areas at the junctions of the epicondyle and the shafts of the femur and tibia and this was confirmed with Doppler ultrasound [1] (Fig. 1).
Target point for the IACSI group was the suprapatellar bursa, determined as a thin anechoic space in the mid-longitudinal ultrasound view, deep to the quadriceps tendon, and superficial to the metaphysis of the femur, referring the superior margin of patella as a landmark to identify its inferior aspect [8] (Fig. 2).
All procedures were performed with a spinal needle (22 G) introduced with ultrasound guidance till reaching the designated target points at both groups. For the GNB group, a mixture of 20 mg of Triamcinolone Acetonide (TA) and 6 mL of lidocaine was equally divided and injected near each of three genicular arteries [1]. While for the IACSI group, a total mixture of 6 cc consisting of 1 mL TA (40 mg) and 5 mL lidocaine inside the suprapatellar bursa [16, 17].
Outcome measurements and follow-up
The severity of pain and the functional capacity of the managed knee joint were evaluated before procedures (as a baseline) and at 2, 4 and 8 weeks after injection at both groups using the visual analog score (VAS) and Oxford knee score (OKS) respectively.
VAS consisted of a graded scale from 0 to 100 (point zero: no pain and point 100 is unbearable pain) and patients were asked to plot a point that corresponds to their pain severity. OKS consist of 12-item questionnaires. Each question was scored from 1 to 5 (one is the least symptoms). Scores from the 12 questions were added to end with a total score between 12 and 60 (12 presents the most favorable outcome) [18]. The absolute values of these scores were collected and compared. The overall benefit from either techniques was evaluated and the differences between the mean values of VAS and OKS obtained at initial pre-procedural baseline and those obtained at 2, 4 and 8 weeks were recorded separately.
Clinical success was defined as decrease of VAS score by at least 5 points [19].
After the injection and during the whole period of follow up, patients were not instructed to adopt any particular recommendations or precautions, didn't receive any oral analgesics, and were not assigned to any rehabilitation program.
Statistical analysis
Data were fed to the computer and analyzed using IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp). Qualitative data were described using number and percent. The Kolmogorov–Smirnov test was used to verify the normality of distribution. Quantitative data were described using range (minimum and maximum), mean, standard deviation, median, and interquartile range (IQR). Significance of the obtained results was judged at the 5% level.
Chi-square test was used for categorical variables to compare between different groups, Fisher’s Exact Correction for chi-square when more than 20% of the cells have expected count less than 5, Student t-test For normally distributed quantitative variables, to compare between two studied groups, ANOVA with repeated measures for normally distributed quantitative variables, to compare between more than two periods or stages, Post Hoc test (Bonferroni adjusted) for pairwise comparisons, and Mann Whitney test For abnormally distributed quantitative variables, to compare between two studied groups.
Results
The current study included 40 patients with symptomatic knee OA. Nine (22.5%) were males and 31 (77.5%) were females, their age ranging from 44 to 65 years. Twenty patients were managed with US guided IACSI and 20 with US guided GNB. For all patients, only a single knee with the most noticeable symptoms was injected.
There were no significant differences between patients treated with either techniques regarding demographics, disease duration, side of managed knee joint, or baseline radiographic disease severity (Table 1).
Technical success was achieved in all patients, as all genicular arteries and suprapatellar bursae were identified and injected successfully with ultrasound guidance. No drug or procedural-related adverse effects were recorded.
Clinical success in term of pain reduction and improved knee joint movements were achieved in all patients at both groups. Mean VAS had significantly dropped from 87.10 and 87.75 at IACSI and GNB groups respectively to a mean of 42.2 and 29.25 at 2 weeks and a mean of 47.7 and 34.25 at 4 weeks. This was statistically significant (p < 0.001). At 8 weeks’ post injection, patients reported recurrence of pain intensity to approach the pre-procedure baseline at both groups (81.5 and 78.5), nevertheless this was not statistically significant (p < 0.804 and p < 0.764) (Table 2).
Similarly, the overall functional capacity of managed knee joints had significantly improved at 2 and 4 weeks after the procedure (mean pre-procedure baseline of 51.3 and 53.25, was reduced to 24.85 and 19.75 at 2 weeks and to 31.20 and 24.65 at 4 weeks for the IACSI and GNB respectively). Improvement was statistically significant for both groups (p < 0.001). At 8 weeks, this result was not sustained (mean increased to 46.05 and 44.75), yet was not statistically significant (p < 0.802 and p < 0.795) (Table 3).
When comparing the mean change of VAS and OKS at 2, 4 and 8 weeks from baseline values for both groups, GNB group showed significantly improved pain and functional capacity at all follow up periods as compared to IACSI group. At VAS, GNB group attained a mean reduction of 58.5, 53.3 and 9.25 points at 2, 4 and 8 weeks respectively compared to 44.9, 39.4 and 5.6 points at IACSI gorups (p < 0.001 at 2 and 4 weeks and was < 0.006 at 8 weeks) (Table 4).
Simiarly at OKS, the GNB group showed siginifctanly better results ( 33.50, 28.60 and 8.5 at GNB and 26.45, 20.10, 5.25 at IACSI (p < 0.001 at all periods) (Table 5).
Discussion
Knee joint Osteoarthritis presents a common health problem that compromises the quality of life of the elderly population. Medical treatment is not always successful and total knee arthroplasty may not be suitable for every patient who might not be candidate for such a major surgery [6].
GNB is a relatively novel technique developed to relieve chronic OA related pains with reported high efficacy [20]. Ultrasound guided GNB showed more effective clinical results when compared to blind injections in a randomized clinical trial of 40 patients [12]. Furthermore, Kim et al. [13] compared the efficacy of GNB when performed with ultrasound and with fluoroscopy in a series of 61 patients. They showed no significant difference in terms of efficacy between both groups, nevertheless ultrasound guidance has the merit to avoid exposure to radiation for the physician and the patients. In this study we referred only to ultrasound to guide our procedures for many reasons. First, due to lacking enough experience to perform blind injections. Furthermore, ultrasound is readily available and accessible in intervention unit without disturbing the workflow of the busy and irradiating angio-suits.
In the present study, patients reported a significant reduction in pain intensity and functional improvement at 2 and 4 weeks following GNB. However, this favorable result was not maintained at 8 weeks. Similar favorable results were published in a series of 48 patients till 4 weeks after GNB, and had returned to baseline at 8 weeks post-procedure [1].
In the current study GNB was performed using a mixture of corticosteroids (TA) and local anesthetic (2% lidocaine). Efficacy of this mixture was shown in the study of Kim et al. [1] who divided their enrolled 48 patients in two equal groups, group one was injected with this same mixture and group two with only anesthetic. They showed that the addition of steroids yielded better results in VAS and OKS at 2 and 4 weeks, still regression of results to baseline occurred at 8 weeks.
In a series of 28 patients with refractory pain after total knee arthroplasty, GNB with steroid analgesic mixture yielded the same short term effect when compared to radiofrequency ablation of the genicular nerves, yet the improvement after radiofrequency was sustained till 6 month [21].
Intra-articular corticosteroid injection (IACSI) is a traditional way to control OA related pains [22, 23]. IACSI was performed through suprapatellar bursal injection and under ultrasound guidance. IACSI was usually carried out blindly, however in a study of 99 patients; US-guided IASCI showed significantly better results than blind injections, with lower incidence of soft tissue infiltration and better intraarticular delivery of the drug [8]. Similarly, results with US guidance surpassed those guided with fluoroscopy [8].
Moreover, as compared to fluoroscopy, ultrasound offers more precise localization of the bursa while avoiding all fluoroscopy related radiation hazards [8].
In a meta-analysis of 1767 patients, Jüni et al. [9] compared the efficacy of intraarticular injection of steroids versus a placebo. Steroids injection showed moderate improvement of pain at 2 weeks, and declined to small and no effect at 13 weeks. At 26 weeks’ post injection, no effect was recorded. Function improvement showed to be small to moderate after steroid injection at 1–2 weeks, with no evident effect at 13 weeks. All data were finally pointing to short term beneficial effect of steroids and no recorded benefits at 6 months after injection. This was coherent to our results showing favorable response only till 4 weeks. When the results of steroid injection were compared to intraarticular injection of hyaluronic acid (HA), steroids were more effective in short term reduction of pain (up to one month), whereas HA injection carried long term effect up to 6 months [24].
In the current study a mixture corticosteroid and a local anesthetic was used as in the IASCI group. Local anesthetic has the merit to provide immediate relief of pain from intra-articular pathology, to dilute the steroid agent, and to decrease or avoid the post-injection flare [25, 26]. Added beneficial effect of mixing a local anesthetic with steroids for intraarticular injection was reported by Jørgensen et al. [27] who showed significant immediate pain reduction that was maintained up to 2 weeks.
When the results obtained after GNB and IACSI were compared, it was found that GNB was significantly more effective than IACSI to relieve pain and to improve the knee function.
To the best of our knowledge, results of IASCI and GNB had not been directly compared in the available literature. Yilmaz et al. [28] compared results of IACSI alone and when combined with GNB. They showed significantly better results when GNB was added as it seemed to enhance the analgesic effect, significantly improved the functional capacity and contributed to better healing process (expressed in increased thickness of the knee cartilage, patellar and quadriceps tendons and quadriceps muscle cross-sectional area).
Many limitations exist in this study. First; the included number of patients is still limited and this could have affected the power of statistics. Second, most of included patients had different educational levels and already suffered from different comorbidities, this could alter their subjective perception to pain improvement. Moreover, a change in emotional status of the patient (notably when long time passes after the intervention) might definitely alter their perception to long term beneficial results of such loco regional treatments. Third; the study lacked a control group, consequently we couldn’t asses the placebo effect especially in the first weeks after treatment. Lastly; single operator performed all the injections.
Conclusions
Both GNB and IACSI are effective to alleviate knee osteoarthritis-related pains and improve functional status up to 4 weeks. When compared to each other, GNB is found to be more effective. Still comparative studies with larger populations are required to validate this data.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- GNB:
-
Genicular nerve block
- IACSI:
-
Intra-articular corticosteroid injection
- VAS:
-
Visual analog scale
- OKS:
-
Oxford knee score
- OA:
-
Osteoarthritis
- TA:
-
Triamcinolone acetonide
- HA:
-
Hayluronic acid
References
Kim DH, Choi SS, Yoon SH, Lee SH, Seo DK, Lee IG et al (2018) Ultrasound-guided genicular nerve block for knee osteoarthritis: a double-blind, randomized controlled trial of local anesthetic alone or in combination with corticosteroid. Pain Phys 21(1):41–52
Robinson WH, Lepus CM, Wang Q, Raghu H, Mao R, Lindstrom TM et al (2016) Low-grade inflammation as a key mediator of the pathogenesis of osteoarthritis. Nat Rev Rheumatol 12(10):580–592
Nelson AE, Allen KD, Golightly YM, Goode AP, Jordan JM (2014) A systematic review of recommendations and guidelines for the management of osteoarthritis: the chronic osteoarthritis management initiative of the U.S. bone and joint initiative. Semin Arthritis Rheum 43(6):701–712
Sharma V, Anuvat K, John L, Davis M (2017) Scientific American pain management-arthritis of the knee. Pain related disease states, Decker
Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J et al (2012) American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 64(4):465–474
Santaguida PL, Hawker GA, Hudak PL, Glazier R, Mahomed NN, Kreder HJ et al (2008) Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg 51(6):428–436
Richards MM, Maxwell JS, Weng L, Angelos MG, Golzarian J (2016) Intra-articular treatment of knee osteoarthritis: from anti-inflammatories to products of regenerative medicine. Phys Sports Med 44(2):101–108
Bum Park Y, Ah Choi W, Kim YK, Chul Lee S, Hae Lee J (2012) Accuracy of blind versus ultrasound-guided suprapatellar bursal injection. J Clin Ultrasound 40(1):20–25
Jüni P, Hari R, Rutjes AWS, Fischer R, Silletta MG, Reichenbach S et al (2015) Intra-articular corticosteroid for knee osteoarthritis. Cochrane Database Syst Rev 10:CD005328.
Saltychev M, Mattie R, McCormick Z, Laimi K (2020) The magnitude and duration of the effect of intra-articular corticosteroid injections on pain severity in knee osteoarthritis: a systematic review and meta-analysis. Am J Phys Med Rehabil 99(7):617–625
Najm A, Alunno A, Gwinnutt JM, Weill C, Berenbaum F (2021) Efficacy of intra-articular corticosteroid injections in knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Joint Bone Spine 88(4):105198
Cankurtaran D, Karaahmet OZ, Yildiz SY, Eksioglu E, Dulgeroglu D, Unlu E (2020) Comparing the effectiveness of ultrasound guided versus blind genicular nerve block on pain, muscle strength with isokinetic device, physical function and quality of life in chronic knee osteoarthritis: a prospective randomized controlled study. Korean J Pain 33(3):258–266
Kim DH, Lee MS, Lee S, Yoon SH, Shin JW, Choi SS (2019) A prospective randomized comparison of the efficacy of ultrasound- vs fluoroscopy-guided genicular nerve block for chronic knee osteoarthritis. Pain Phys 22(2):139–146
Sconfienza LM, Albano D, Allen G, Bazzocchi A, Bignotti B, Chianca V et al (2018) Clinical indications for musculoskeletal ultrasound updated in 2017 by European Society of Musculoskeletal Radiology (ESSR) consensus. Eur Radiol 28(12):5338–5351
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Sh SN, Ram GG (2019) Is intra articular injection of triamcinolone acetonide a better option in management for primary osteoarthritis knee than methylprednisolone acetate? Int J Res Orthop 5(3):515
Cardone DA, Tallia AF (2002) Joint and soft tissue injection. Am Fam Phys 66(2):283–288
Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br 80(1):63–69
Sconfienza LM, Albano D, Messina C, Gitto S, Guarrella V, Perfetti C et al (2020) Ultrasound-guided percutaneous tenotomy of the long head of biceps tendon in patients with symptomatic complete rotator cuff tear in vivo non-controlled prospective study. J Clin Med 9(7):2114
McCormick ZL, Korn M, Reddy R, Marcolina A, Dayanim D, Mattie R et al (2017) Cooled radiofrequency ablation of the genicular nerves for chronic pain due to knee osteoarthritis: six-month outcomes. Pain Med 18(9):1631–1641
Qudsi-Sinclair S, Borrás-Rubio E, Abellan-Guillén JF, Padilla Del Rey ML, Ruiz-Merino G (2017) A comparison of genicular nerve treatment using either radiofrequency or analgesic block with corticosteroid for pain after a total knee arthroplasty: a double-blind, randomized clinical study. Pain Pract 17(5):578–588
Sharif B, Kopec J, Bansback N, Rahman MM, Flanagan WM, Wong H et al (2015) Projecting the direct cost burden of osteoarthritis in Canada using a microsimulation model. Osteoarthritis Cartilage 23(10):1654–1663
Ostergaard M, Halberg P (1998) Intra-articular corticosteroids in arthritic disease: a guide to treatment. BioDrugs 9(2):95–103
He WW, Kuang MJ, Zhao J, Sun L, Lu B, Wang Y et al (2017) Efficacy and safety of intraarticular hyaluronic acid and corticosteroid for knee osteoarthritis: a meta-analysis. Int J Surg 39:95–103
Centeno LM, Moore ME (1994) Preferred intraarticular corticosteroids and associated practice: a survey of members of the American College of Rheumatology. Arthritis Care Res 7(3):151–155
Martin CL, Browne JA (2019) Intra-articular corticosteroid injections for symptomatic knee osteoarthritis: what the orthopaedic provider needs to know. J Am Acad Orthop Surg 27(17):e758–e766
Jørgensen TS, Graven-Nielsen T, Ellegaard K, Danneskiold-Samsøe B, Bliddal H, Henriksen M (2014) Intra-articular analgesia and steroid reduce pain sensitivity in knee OA patients: an interventional cohort study. Pain Res Treat 2014:710490
Yilmaz V, Umay E, Gundogdu I, Aras B (2019) The comparison of efficacy of single intraarticular steroid injection versus the combination of genicular nerve block and intraarticular steroid injection in patients with knee osteoarthritis: a randomised study. Musculoskelet Surg:doi. https://doi.org/10.1007/s12306-12019-00633-y
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
AR: designed the work, acquisition and analysis and interpretation of data. SH: designed the work and substantively revised it. RE: designed the work and data analysis. AA: designed the work, acquisition and analysis and substantively revised it. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee of the Faculty of Medicine at Alexandria University in Egypt (IRB NO: 00012098, FWA NO: 00018699) on 24/10/2019 with serial number 0106129. All patients included in this study gave written informed consent to participate in this research.
Consent for publication
All patients included in this research gave written informed consent to publish the data contained within this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ragab, A.R., Hegab, S., Elnemr, R. et al. Intra-articular corticosteroid injection and genicular nerve block under ultrasound guidance in pain control of knee osteoarthritis. Egypt J Radiol Nucl Med 52, 196 (2021). https://doi.org/10.1186/s43055-021-00577-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-021-00577-z