Abstract
Background
Juvenile idiopathic arthritis (JIA) can cause reduced exercise capacity, deterioration in functional activities, and poor health-related quality of life. This study aims to objectively reveal lower extremity involvement in the peripheral predominant forms of juvenile idiopathic arthritis through qualitative evaluations and to determine the effects of these involvements on exercise, function, and quality of life.
Methods
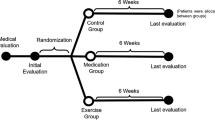
Thirty-two patients with a history of peripheral arthritis and aged between 7 and 16 years participated in the study. Demographics, JIA subtype, disease duration, arthritis and deformities of the lower extremity, disease activity score, 6-min walk test (6MWT), cycling exercise test (CYC-E), childhood health assessment questionnaire (CHAQ), and pediatric quality of life inventory (PedsQoL) scores were recorded. In case of clinical suspicion of arthritis, an ultrasonographic examination was performed for a definitive diagnosis. Regression analyses were performed to explore the most associated lower extremity involvement and patient characteristics for each of the dependent variables including 6MWT, CYC-E, CHAQ, and PedsQoL.
Results
Of the total number of patients, with a mean age of 12.91 (SD 2.37) years, 28.1% had knee arthritis, 15.6% foot arthritis, 12.5% hip arthritis, and 37.5% lower extremity deformity. The parameters that were most associated with CHAQ and PedsQoL were hip and knee arthritis, whereas CYC-E was found to be most associated with knee arthritis and height, and 6MWT was found to be most associated with hip arthritis, knee arthritis, and demographic characteristics.
Conclusion
This study emphasizes the importance of hip and knee arthritis, which are among the determinants of walking endurance, function, and quality of life; and knee arthritis, which is among the determinants of cycling performance in JIA with lower extremity involvement.
Similar content being viewed by others
Background
Juvenile idiopathic arthritis (JIA) is the most common pediatric rheumatologic disease. Subluxation, fusion, and permanent joint deformities occur with damage to the joint surfaces and their adjacent structures. In addition to joint involvement, muscle strength, atrophy, weak endurance, gait disturbances, decreased exercise capacity, and decreased function and quality of life can be seen [1,2,3,4]. The hip, knee, and ankle are the most frequently affected lower extremity joints in JIA, with a prevalence rate of 30–50% [5]. It is also known that the most common joints requiring surgical intervention in adult JIA are the hip, knee, and ankle [6].
Children with JIA have poor function and exercise scores than healthy children [3, 4, 7,8,9,10,11]. When investigating the factors affecting these results, quantitative assessment methods, such as the number of swollen joints and tender joints, are generally used. Ultimately, it is recommended to reduce the number of tender/swollen joints (or decrease the disease activity scale scores) [12, 13]. However, the joint which mostly affects daily activities and quality of life in childhood, including exercise, is still a matter of curiosity.
Foot/ankle and hips can be affected in JIA, but these symptoms are more difficult to diagnose than knee arthritis. The impact of their subclinical involvement of them on daily life may sometimes be neglected [14]. Further, treatments may not necessarily cause complete remission of active arthritis in these joints [5]. Physical examination can easily diagnose knee arthritis; however, conditions such as arthritis, bursitis, or tenosynovitis of the ankle and hip are more difficult than knee to distinguish by physical examination [5, 15, 16]. In recent years, the introduction of ultrasonography (USG) in clinical use has enabled clinicians to easily differentiate these conditions. USG can demonstrate ongoing active disease in locations that are difficult to examine in JIA. It is reported to be more sensitive and reliable than physical examination and correlates better with disease activity indices as well as the progression of structural damage [17, 18]. Hence, a more objective examination is required in cases where physical examination is insufficient for evaluating the results affected by joint involvement.
The involvement and deformities of the lower extremity and the need for orthosis in JIA begin to appear in childhood; however, there is insufficient data in the literature regarding the comprehensive assessment of deformities [5]. To our knowledge, there is one validated damage scale, Juvenile Arthritis Damage Index - Articular (JADI-A), which includes assessment of the contracture of the hip, knee, ankle, and metatarsal joints and valgus knee deformity [19]. Nevertheless, it is unclear whether deformities are risk factors (independent from arthritis) for the poor exercise results.
In light of the aforementioned data, there is no study conducted with both qualitative, comprehensive, and objective evaluation methods that have revealed lower extremity impairments affecting exercise and daily life outcomes in JIA. We believe that investigating the qualitative effect (based on the location) rather than the number of joints swollen, objectively diagnosing arthritis with the use of USG, and including deformity in the analysis can increase the scope and provide more reliable results.
This study aims to objectively reveal lower extremity involvement in peripheral predominant forms of juvenile idiopathic arthritis through qualitative evaluations and to determine the effects of these involvements on two different exercise performances, function, and quality of life.
Methods
Patients
We included patients aged between 7 and 16 years and diagnosed with JIA according to the International League of Associations for Rheumatology criteria in Ankara Dışkapı Yıldırım Beyazıt Training and Research Hospital [20]. The diagnosis of JIA was made by a pediatric rheumatologist. Patients with axial involvement, systemic JIA (to minimize the systemic effects of disease), active infections, and patients who were newly diagnosed were excluded. Informed consent was obtained from the participants and their parents. Demographic characteristics, disease duration, disease subtypes, medications, Disease Activity Score28 (DAS-28) results, and the data below were recorded.
DAS28 was calculated with ESR (mm/h), tender and swollen joint count among 28 joints, and the patient’s global assessment of disease activity on a visual analog scale. It predominantly evaluates the activity of the upper extremities.
Arthritis
Physical examination of the knee, hip, ankle, and foot joints was performed by the same physician. Patients with apparent arthritis were noted. Patients with suspicious arthritis (at least one of the following symptoms such as pain, tenderness, redness, warmth, or loss of function) were subjected to USG examination performed by an experienced specialist who was unaware of the clinical findings. For this purpose, General Electric Logiq 5 (frequency: 7–13 MHz) ultrasound device, linear probe, and gray scale were used. Definite arthritis on physical examination or at least grade 1 synovial fluid and/or grade 1 synovial hypertrophy on USG were considered arthritis positive [20].
Deformity
The patients’ physical examination and goniometric measurements were performed by a physical medicine and rehabilitation specialist. The deformity status was determined according to the JADI-A [19] in which joint contracture and other deformities were only be scored when they are not due to active arthritis and present for at least six months. In addition, we distinguished the patients according to the lower extremity deformity (LED) presence. Since there was no standardization for the deformity assessment, we considered LED positive if a patient had any of the followings: hip internal rotation < 10 degrees, hip ankylosis/prosthesis, knee valgus > 15 degrees, knee flexion contracture, knee prosthesis, fixed valgus of the ankle, ankle ankylosis/arthrodesis/prosthesis, visible deformity of the metatarsophalangeals due to arthritis, or arthroplasty of the forefoot (measurements are from JADI-A) [19].
Primary outcome measurements (in order of application)
-
1.
Function. The childhood health assessment questionnaire (CHAQ) was used for the assessment of functional ability. The ratings of the scale were determined by the physician with face-to-face encounters with the patients and their parents. For each item of CHAQ, the patient’s difficulty level experienced while performing a relevant activity is questioned. The scoring was done using a four-point scale ranging from 0 (without any difficulty), 1 (with some difficulty), 2 (with much difficulty), 3 (unable to do). If assistance was required of a person or device, the scoring was increased to 2 if 0 or 1 points whereas ratings of 2 and 3 points remained unaffected. The CHAQ score was calculated as the sum of the scores of all the eight sections divided by 8, which is in the range 0–3. The Turkish validity and reliability study of this score has been performed [21].
-
2.
Quality of life. The PedsQL 3.0 Arthritis Module (PedsQL-3A), which evaluates the QoL based on patient-reported outcomes, was used. There were 3 forms of the questionnaire, classified according to the following age groups: 5–7, 8–12, and 13–18 years. It consisted of 5 sub-items including pain/ache, activities of daily living, treatment, anxiety, and communication. The total score of Likert-type questions was between 0 and 100 and the best score was 100. It has been validated in Turkish [22]. The physician conducted the questionnaires face-to-face with patients.
-
3.
Cycling exercise performance. The cycling exercises (CYC-E) were applied on the CareFusion Type MasterScreen-CPX device to simulate home cycling. Since there was not a standardized and validated cycling protocol for home exercise in JIA, a cycling protocol was created for this study [13, 23]. The protocol should be partially achievable for healthy and active children, with no floor and ceiling effect for children with JIA [23]. Therefore, pilot tests were performed on 11 JIA and 11 age-matched healthy children to decide on the protocol. The final cycling protocol was developed where the results of the healthy subjects exhibited a ceiling effect in a 20-min exercise without observing floor or ceiling effect in patients (no more than 15% of respondents having the lowest and highest possible response) and close to submaximal difficulty: After warming up at 90–100 rpm without any load for 3 min, the participants continued the test with a load equivalent to half of their weight at 90–100 rpm, then a 20-min exercise was performed with a 1-watt load increase every 3 min. Participants were informed about 3 h of fasting, maximal effort, degree of strain, and possible symptoms before cycling. Simultaneously, the heart rate was measured with a probe. The age-predicted maximum heart rate (HRmax) was calculated for each participant and the peak heart rate (HRpeak) reached during the test was measured [23, 24]. The exercise test was terminated prematurely if the patient stated that he could not continue the exercise for any reason or when indications for termination of the exercise test occurred [25]. Cycling exercise duration (CYC-ED) was recorded as an outcome.
-
4.
Walking endurance. The 6-min walk test (6MWT) was used for this purpose. Unlike all other evaluations, the 6MWT was performed on the next day so that the cycling test would not affect the 6MWT results. It was conducted in a straight 8-m corridor. Patients were instructed to walk the longest possible distance within 6 min at their normal walking pace with turning points at both ends of the 8-m distance. The patient was motivated at each turn. The distance covered at the end of the exercise was recorded. The 6MWT is a reliable method for evaluating exercise capacity in JIA [26, 27].
All exercise tests were performed during noontime and under the control of a physical medicine and rehabilitation specialist experienced in cardiac rehabilitation.
Statistics
Statistical analysis was done using the SPSS V.20. Descriptive statistics were presented as percentages for categorical variables, as mean (with SD) for normally distributed continuous data, and as median (with IQR) for non-normal distributed continuous data. To determine relationships with potential independent variables (age, gender, height, weight, BMI, disease duration, hip arthritis, knee arthritis, foot/ankle arthritis, JADI-A, and LED score) that may affect primary outcome measurements (CHAQ, PedsQL-3A, CYC-ED, 6MWT), Pearson test for normally distributed continuous quantitative data, Spearman test for non-normally distributed continuous quantitative data, Student T-test for normally distributed categorical variables, and Mann–Whitney U test for non-normally distributed categorical variables were performed. Backward multivariate linear regression analysis was used to determine the best predictors of CHAQ, PedsQl-3A, CYC-E, and 6MWT. In addition to hip, knee, and foot/ankle arthritis, the parameters that were found to be significant in the tests mentioned above were included in the models. P < 0.05 was considered significant.
Results
Thirty-two patients with a diagnosis of JIA (13 boys, 19 girls) were included in the study. 6MWT data of 2 patients (1 boy, 1 girl) were missing. There was no other missing data. Data regarding demographics, clinical, and exercise tests of the patients with a diagnosis of JIA are shown in Table 1. Bilateral knee arthritis was found in one patient and unilateral or no lower extremity arthritis in all other patients.
During CYC-E, the heart rate increased to an average of 83% (95% CI 0.80–0.87) of maximal heart rate and stabilized after 3–6 min. A significant correlation was found between the 6MWT and CYC-E results of the patients (Pearson’s correlation coefficient 0.534, p: 0.002).
Associations between the dependent and independent variables are shown in Table 2. Several individual and disease-related characteristics were associated with various outcome measures.
For each primary outcome measure, foot/ankle, knee, and hip arthritis that were likely to clinically affect the outcomes were included in each regression model. In addition, the independent variables shown in italics in Table 2 were included in the relevant model, except JADI-A. The JADI-A was not included as it showed collinearity with the presence of lower limb deformity. The final models of the backward multivariate linear regression analysis for each primary outcome measure are shown in Table 3.
Discussion
This study is the first to investigate the contribution of lower limb arthritis, particularly hip and knee arthritis, in poor outcomes in walking, cycling, function, and quality of life in children with JIA with peripheral arthritis. In JIA with lower extremity involvement, the most important determinants of walking endurance, function, and quality of life are hip and knee arthritis, whereas knee arthritis is crucial in cycling performance. The literature search showed us when investigating factors affecting poor outcomes in children with JIA, quantitative assessment methods, such as the number of swollen joints and tender joints, have often been used. It has been proposed to ultimately reduce the number of tender/swollen joints (or lower disease activity scale scores) [12, 13, 28]. On the other hand, the present study indicates that different joints affect the result differently with the qualitative assessment.
In this study, knee arthritis was observed at a rate of 28.1%, foot/ankle 15.6%, and hip 12.5% when clinical and subclinical arthritis were evaluated together. These rates correspond with the findings in the literature. In a study conducted in patients under one year of treatment, the prevalence of knee, ankle, foot, and hip synovitis was 8–20%, 6–12%, 5, and < 5%, respectively, and walking difficulty was observed at rates of 25–30% [29]. The joint involvement that would best explain this difficulty in walking seen in the majority of the patients is not specified, and the diagnosis of arthritis is based solely on physical examination. However, it is important to distinguish subclinical synovitis in children, especially in feet and hip joints, and not to omit them while investigating the causes associated with the result. Each patient should be specifically evaluated for these joints by clinical and, if necessary, subclinical examination [15, 16].
It is well known that children with JIA have a decreased functional competence and quality of life than healthy children [4]. In a previous large sample study, predictors of disability assessed by HAQ were female gender, symmetrical arthritis, hip joint involvement, long-term high ESR, and rheumatoid factor [11]. Regarding the quality of life, the effect of the number of swollen joints was highlighted in another study [30]. It is noteworthy that in the current study, a significant part of the variance in both functional loss and quality of life was explained by hip and knee arthritis.
The average of 6MWT in our study was at expected levels when compared with the previous study [31] and was lower than healthy Turkish children [32]. The findings of our study highlight that out of all the factors, hip arthritis may have the greatest impact on this low score of 6MWT. In addition to hip arthritis, knee arthritis, gender, age, and weight explain 70.1% of the variance in 6MWT. This result suggests that walking endurance can be widely affected by active hip and knee arthritis. However, 6MWT is a widely used method to assess cardiovascular exercise capacity, and it has also been included in home exercise programs given to children with JIA in clinical trials [27, 33,34,35]. Hence, we also investigated a different exercise performance that was less likely to be affected by the effect of active arthritis in assessing actual cardiovascular performance. Although respiratory and metabolic requirements differ during cycling and walking exercise [36], we hypothesized that the effect of arthritis on cycling performance would not be as great as that on walking endurance.
In our study, a protocol that can provide a cycling exercise result with a wide variance was applied. CYC-E correlated moderately with 6MWT and remained at the submaximal exercise level determined by heart rate measurement. Ultimately, as intended, an intense home exercise cycling performance was provided [23]. When we investigated the contribution of lower extremity involvement to cycling performance, it was seen that 29.9% of the variance was explained by the presence of knee arthritis and height. Although this data is similar to the effect of height determined in the study of Paap et al. [27], our study is unique in that it also includes the contributing joints. In conclusion, this study contributes to the literature by indicating that walking and cycling endurances are affected by different factors in these patients and hip arthritis has a greater influence on walking than cycling.
Although lower extremity deformity examined in this study is not found as an independent risk factor for poor outcome, it can be assumed that there is a questionable effect on walking endurance. On the other hand, it was not associated with CHAQ, unlike a previous study [37]. The failure to identify lower extremity deformities as an independent factor may be since it is indeed not so or may be because our sample did not include a great sample size. Future studies are required to investigate the effect of the presence of deformity on adverse outcomes with larger samples and established disease. Apart from arthritis and deformity, one of the conditions most likely to be associated with reduced physical activity in children with inflammatory diseases is pain [10]. However, the pain was not included in independent factors in this study, because it is a subjective complaint and our outcome variables could be influenced by any pain in children [38]. Hence, a definite diagnosis of arthritis has provided more reliable observations in understanding the contribution of lower extremity arthritis to the results. In addition to all, there is a need to design and validate tools assessing optimal LED (especially other deformities of the foot) and home exercise performances [5]. The pilot study that we conducted because of a lack of protocol that can be considered as a home program for cycling exercise in the literature, has ensured that this issue is relatively tolerated [23].
The results might have been different if the majority had been diagnosed with polyarticular or systemic JIA. The variances in the primer outcome measures might have probably not been explained that well. However, the main purpose of this study was to find out the value of lower extremity involvement type in itself. The results should not be generalized to all JIAs. Future research is needed to explain the variance of disability or QoL in the general JIA population.
Conclusions
This study highlights that hip and knee arthritis are the most important determinants of poor outcome in walking, function, and quality of life in children with JIA with peripheral arthritis alone; in addition, considering the cycling performance, the hip arthritis factor is relatively eliminated. Each patient should be evaluated especially in terms of these joints with clinical and, if necessary, subclinical examination.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- JIA:
-
Juvenile idiopathic arthritis
- 6MWT:
-
6-min walk test
- CYC-E:
-
Cycling exercise test
- CHAQ:
-
Childhood Health Assessment Questionnaire
- PedsQoL:
-
Pediatric Quality of Life Inventory Arthritis Module
- USG:
-
Ultrasonography
- JADI-A:
-
Juvenile Arthritis Damage Index Articular
- DAS-28:
-
Disease Activity Score 28
- LED:
-
Lower extremity deformity
References
Oen K. Long-term outcomes and predictors of outcomes for patients with juvenile idiopathic arthritis. Best Pract Res Clin Rheumatol. 2002;16(3):347–60. https://doi.org/10.1053/berh.2002.0233.
Packham JC, Hall MA. Long-term follow-up of 246 adults with juvenile idiopathic arthritis: functional outcome. Rheumatology. 2002;41(12):1428–35. https://doi.org/10.1093/rheumatology/41.12.1428.
Van Brussel M, Lelieveld OTHM, Van Der Net J, et al. Aerobic and anaerobic exercise capacity in children with juvenile idiopathic arthritis. Arthritis Care Res. 2007;57(6):891–7. https://doi.org/10.1002/art.22893.
Takken T, Van Der Net J, Helders PJM. Relationship between functional ability and physical fitness in juvenile idiopathic arthritis patients. Scand J Rheumatol. 2003;32(3):174–8. https://doi.org/10.1080/03009740310002524.
Fellas A, Singh-Grewal D, Santos D, Coda A. Physical examination tools used to identify swollen and tender lower limb joints in juvenile idiopathic arthritis: a scoping review. Arthritis. 2018;2018:1–7. https://doi.org/10.1155/2018/3408162.
Malviya A, Johnson-Lynn S, Avery P, Deehan D, Foster H. Juvenile idiopathic arthritis in adulthood and orthopaedic intervention. Clin Rheumatol. 2009;28(12):1411–7. https://doi.org/10.1007/s10067-009-1266-0.
van Pelt PA, Takken T, van Brussel M, et al. Aerobic capacity and disease activity in children, adolescents and young adults with juvenile idiopathic arthritis (JIA). Pediatr Rheumatol Online J. 2012;10(1):25. https://doi.org/10.1186/1546-0096-10-25.
Takken T, Van Der Net J, Kuis W, Helders PJM. Physical activity and health related physical fitness in children with juvenile idiopathic arthritis. Ann Rheum Dis. 2003;62(9):885–9. https://doi.org/10.1136/ard.62.9.885.
Takken T, Hemel A, Van Der Net J, Helders PJM. Aerobic fitness in children with juvenile idiopathic arthritis: a systematic review. J Rheumatol. 2002;29(12):2643–7.
Bos GJ, Lelieveld OT, Armbrust W, et al. Physical activity in children with Juvenile Idiopathic Arthritis compared to controls. Pediatr Rheumatol Online J. 2016;14(1):42. https://doi.org/10.1186/s12969-016-0102-8.
Flatø B, Lien G, Smerdel A, et al. Prognostic factors in juvenile rheumatoid arthritis: a case-control study revealing early predictors and outcome after 14.9 years. J. Rheumatol. 2003;30(2):386–93.
Giannini EH, Ruperto N, Ravelli A, Lovell DJ, Felson DT, Martini A. Preliminary definition of improvement in juvenile arthritis. Arthritis Rheum. 1997;40(7):1202–9. https://doi.org/10.1002/1529-0131(199707)40:7<1202::AID-ART3>3.0.CO;2-R.
Cavallo S, Brosseau L, Toupin-April K, Wells GA, Smith CA, Pugh AG, et al. Ottawa panel evidence-based clinical practice guidelines for structured physical activity in the management of juvenile idiopathic arthritis. Arch Phys Med Rehabil. 2017;98(5):1018–41. https://doi.org/10.1016/j.apmr.2016.09.135.
Spraul G, Koenning G. A descriptive study of foot problems in children with juvenile rheumatoid arthritis (JRA). Arthritis Rheum. 1994;7(3):144–50. https://doi.org/10.1002/art.1790070308.
Magni-Manzoni S, Epis O, Ravelli A, Klersy C, Veisconti C, Lanni S, et al. Comparison of clinical versus ultrasound-determined synovitis in juvenile idiopathic arthritis. Arthritis Care Res. 2009;61(11):1497–504. https://doi.org/10.1002/art.24823.
Collado P, Jousse-Joulin S, Alcalde M, Naredo E, D’Agostino MA. Is ultrasound a validated imaging tool for the diagnosis and management of synovitis in juvenile idiopathic arthritis? A systematic literature review. Arthritis Care Res. 2012;64(7):1011–9. https://doi.org/10.1002/acr.21644.
Grassi W. Clinical evaluation versus ultrasonography: who is the winner? J Rheumatol. 2003;30(5):908–9.
Hendry GJ, Gardner-Medwin J, Steultjens MPM, Woodburn J, Sturrock RD, Turner DD. Frequent discordance between clinical and musculoskeletal ultrasound examinations of foot disease in juvenile idiopathic arthritis. Arthritis Care Res. 2012;64(3):441–7. https://doi.org/10.1002/acr.20655.
Viola S, Felici E, Magni-Manzoni S, Pistorio A, Buoncompagni A, Ruperto N, et al. Development and validation of a clinical index for assessment of long-term damage in juvenile idiopathic arthritis. Arthritis Rheum. 2005;52(7):2092–102. https://doi.org/10.1002/art.21119.
Szkudlarek M, Court-Payen M, Jacobsen S, Klarlund M, Thomsen HS, Østergaard M. Interobserver agreement in ultrasonography of the finger and toe joints in rheumatoid arthritis. Arthritis Rheum. 2003;48(4):955–62. https://doi.org/10.1002/art.10877.
Ruperto N, Ravelli A, Pistorio A, et al. Cross-cultural adaptation and psychometric evaluation of the Childhood Health Assessment Questionnaire (CHAQ) and the Child Health Questionnaire (CHQ) in 32 countries. Review of the general methodology. Clin. Exp. Rheumatol. 2001;19(4 SUPPL. 23):S1–9.
Tarakci E, Baydogan SN, Kasapcopur O, Dirican A. Cross-cultural adaptation, reliability, and validity of the Turkish version of PedsQL 3.0 arthritis module: a quality-of-life measure for patients with juvenile idiopathic arthritis in Turkey. Qual. Life Res. 2013;22(3):531–6. https://doi.org/10.1007/s11136-012-0180-0.
Noonan V, Dean E. Submaximal exercise testing: clinical application and interpretation. Phys Ther. 2000;80(8):782–807. https://doi.org/10.1093/ptj/80.8.782.
Machado FA, Denadai BS. Validity of maximum heart rate prediction equations for children and adolescents. Arq Bras Cardiol. 2011;97(2):136–40. https://doi.org/10.1590/S0066-782X2011005000078.
Washington RL, Bricker JT, Alpert BS, et al. Guidelines for exercise testing in the pediatric age group: From the Committee on Atherosclerosis and Hypertension in Children, Council on Cardiovascular Disease in the Young, the American Heart Association. Circulation. 1994;90(4 I):2166–79.
Pritchard L, Verschuren O, Roy M, Kaup C, Rumsey DG. Reproducibility of the Six-Minute Walk Test in Children and Youth with Juvenile Idiopathic Arthritis. Arthritis Care Res (Hoboken). 2020;10.1002/acr.24492. https://doi.org/10.1002/acr.24492.
Paap E, Van Der Net J, Helders PJM, Takken T. Physiologic response of the six-minute walk test in children with juvenile idiopathic arthritis. Arthritis Care Res. 2005;53(3):351–6. https://doi.org/10.1002/art.21175.
Giannini MJ, Protas EJ. Exercise response in children with and without juvenile rheumatoid arthritis: a case-comparison study. Phys Ther. 1992;72(5):365–72. https://doi.org/10.1093/ptj/72.5.365.
Hendry GJ, Shoop-Worrall SJ, Riskowski JL, et al. Prevalence and course of lower limb disease activity and walking disability over the first 5 years of juvenile idiopathic arthritis: results from the childhood arthritis prospective study. Rheumatol Adv Pract. 2018;2(2):rky039. https://doi.org/10.1093/rap/rky039.
Ezzahri M, Amine B, Rostom S, Badri D, Mawani N, Gueddari S, et al. Factors influencing the quality of life of Moroccan patients with juvenile idiopathic arthritis. Clin Rheumatol. 2014;33(11):1621–6. https://doi.org/10.1007/s10067-014-2489-2.
Lelieveld OTHM, Takken T, Van Der Net J, Van Weert E. Validity of the 6-minute walking test in juvenile idiopathic arthritis. Arthritis Care Res. 2005;53(2):304–7. https://doi.org/10.1002/art.21086.
Kanburoglu MK, Ozdemir FM, Ozkan S, Tunaoglu FS. Reference values of the 6-minute walk test in healthy Turkish children and adolescents between 11 and 18 years of age. Respir Care. 2014;59(9):1369–75. https://doi.org/10.4187/respcare.02891.
Tarakci E, Yeldan I, Nilay Baydogan S, Olgar S, Kasapcopur O. Efficacy of a land-based home exercise programme for patients with juvenile idiopathic arthritis: a randomized, controlled, single-blind study. J Rehabil Med. 2012;44(11):962–7. https://doi.org/10.2340/16501977-1051.
Sule SD, Fontaine KR. Slow speed resistance exercise training in children with polyarticular juvenile idiopathic arthritis. Open Access Rheumatol Res Rev. 2019;11:121–6.
Klepper S, Mano Khong TT, Klotz R, Gregorek AO, Chan YC, Sawade S. Effects of structured exercise training in children and adolescents with juvenile idiopathic arthritis. Pediatr Phys Ther. 2019;31(1):3–21. https://doi.org/10.1097/PEP.0000000000000555.
Palange P, Forte S, Onorati P, Manfredi F, Serra P, Carlone S. Ventilatory and metabolic adaptations to walking and cycling in patients with COPD. J Appl Physiol. 2000;88(5):1715–20. https://doi.org/10.1152/jappl.2000.88.5.1715.
Sarma PK, Misra R, Aggarwal A. Physical disability, articular, and extra-articular damage in patients with juvenile idiopathic arthritis. Clin Rheumatol. 2008;27(10):1261–5. https://doi.org/10.1007/s10067-008-0901-5.
Costa MDC, Natour J, Oliveira HAV, Terreri MT, Len CA. Gait in children and adolescents with idiopathic musculoskeletal pain. Adv. Rheumatol. (London, England). 2019;59(1):7.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and analysis were performed by SAK and AÇ. Data collection and diagnosis were made by ÖB and BÇA. Sonographic assessments were made by ABH. Exercise tests were made under the control of ÖZK and HHG. The first draft of the manuscript was written by SAK and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Authors’ information
SAK and HHG: Physicians specialized in Physical Medicine and Rehabilitation and Rheumatology. ÖZK: Associate Professor specialized in Physical Medicine and Rehabilitation. ABH: Professor specialized in Physical Medicine and Rehabilitation. ÖB: Physician specialized in Pediatric Rheumatology. BÇA: Professor specialized in Pediatric Rheumatology. AÇ: Physician specialized in Physical Medicine and Rehabilitation and the Chairperson.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by Institutional Research Ethics Committee (21042014–15/17). All patients and their parents signed written informed consent.
Consent for publication
All authors read and approved the final manuscript and give their consent for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Acer Kasman, S., Karaahmet, Ö.Z., Bal Hastürk, A. et al. The importance of lower extremity involvement type on exercise performances, function, and quality of life in peripheral predominant forms of juvenile idiopathic arthritis. Adv Rheumatol 61, 39 (2021). https://doi.org/10.1186/s42358-021-00195-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42358-021-00195-3