Abstract
Background
Airway anesthesia is pivotal for successful awake intubation provided either topically or by nerve blocks. The widespread use of ultrasonography allows anesthesiologists to evaluate complex and varied anatomy before needle insertion. This study aims to evaluate the effect of ultrasound-guided technique for the block of the internal branch of the superior laryngeal nerve in difficult airway patients in comparison to blind anatomical technique. Sixty patients aged 18–60 years, of either sex, with the American Society of Anesthesiologists’ physical status (ASA) I–II were divided into two groups 30 patients of each. Group (L): using anatomical landmark technique to bilateral block internal branch of the superior laryngeal nerve (ibSLN) with 1 mL 2% Lidocaine and group (U): using ultrasound technique to bilateral block the ibSLN with 1 mL 2% Lidocaine. Assessment of the excellence of airway anesthesia during intubation by using the 5 points grading scale, time for intubation, effects on hemodynamic variables, and evaluation of patient awareness of pain and discomfort during fiber-optic intubation using numerical rating scale were compared.
Results
The duration of tracheal intubation was shorter in the ultrasound group as compared to the anatomical group; also, patient comfort was significantly better in the ultrasound group besides the effect of tracheal intubation on hemodynamics which was significant with a higher peak value during intubation and post-intubation in the anatomical group compared to the ultrasound group.
Conclusions
This study concludes that an ultrasound-guided block of ibSLN used as a part of the preparation of the airway for awake fiber-optic intubation enhances the quality of airway anesthesia and patient tolerance during the procedure.
Similar content being viewed by others
Background
Awake fiber-optic intubation is considered the gold standard for the endotracheal intubation of patients with a foreseen difficult airway. The pharmacological and psychological preparation of the patient contribute to the success of awake fiber-optic intubation (Ramkumar, 2011).
Since awake intubation makes inconvenient patients, different procedures were depicted to accomplish airway anesthesia, for example, topical application of local anesthetics and injection of local anesthetic agents at explicit anatomic milestones to block the afferent neural transmission from the oropharynx and larynx (Ambi et al., 2017).
The superior laryngeal nerve (SLN) has its origin from the vagus nerve. It descends, by the side of the pharynx, behind the internal carotid artery, and at the level of the hyoid bone, it divides into external and internal branches.
The internal branch supplies a sensory function to the lower part of the pharynx and the upper portion of the larynx above the vocal cords (base of the tongue, posterior epiglottis, aryepiglottic folds, and arytenoids) as it passes immediately inferior to the greater horn of the hyoid bone and enters the thyrohyoid membrane about 2–4 mm inferior to the greater cornu, proceeding submucosally in the piriform recess (Kundra et al., 2011).
In patients going through awake fiber-optic intubation as a part of airway anesthesia, an internal branch of SLN block is regularly performed and is ordinarily done by perceiving the greater horn of the hyoid bone and superior horn of the thyroid cartilage as anatomic milestones at the territory between the thyroid cartilage and the hyoid bone the ibSLN is the solitary nerve which traverses laterally to medial (Furlan, 2002).
Using ultrasound for nerve blocks is more successful, takes less time, and has a faster onset, longer duration of action, and fewer complications (such as intravascular or intraneural injection) than the anatomical landmark technique. The same advantages may be possible with an ultrasound-guided internal branch of the superior laryngeal nerve (ibSLN) block (Manikandan et al., 2010).
Few case reports are accessible surveying the advantages of ultrasound over the anatomical markers guided technique for blocking the internal branch of the superior laryngeal nerve (ibSLN).
Considering all these aspects, the present study was designed to assess the excellence of airway anesthesia using the ultrasound-guided technique for the block of the internal branch of the superior laryngeal nerve in a surgical patient in comparison to blind anatomical landmark technique which was our primary outcome under investigation. Secondary outcomes were to evaluate patient awareness of pain and discomfort during fiber-optic intubation, time for intubation, and effects on hemodynamic variables.
Methods
After obtaining approval from the medical ethical committee number MS19/2020, this randomized comparative prospective study was conducted in El Demerdash Teaching Hospital Cairo, Egypt, during the period from May 2018 to June 2020
Sixty patients with ASA (American Society of Anesthesiologists) physical statuses I and II, age between 40 and 60 years, and with an anticipated difficult airway Modified Mallampati classes III–IV were scheduled for awake fiber-optic intubation after explaining the procedure and obtained written informed consent from every patient. The patients were randomly divided by computer-generated random sequence into group L: (n =30 patients) using anatomical landmark technique and group U (n =30 patients) using ultrasound-guided technique.
Patients with local pathology of the neck, bleeding diathesis, allergy to the local anesthetic agent, or uncooperative patients (due to confusion or learning disabilities), and patients with body mass index ≥30 kg/m2 were excluded from this study.
Preoperative assessment including history taking, clinical examination, and laboratory investigations was done the day before surgery. Patients were instructed to fast for 8 h.
Intraoperative basic monitoring including ECG, pulse oximetry, and non-invasive blood pressure (NIBP) was applied to all patients. Basal measurements were taken.
Inhalation of nebulized 3ml lidocaine 4% was given over 10 min to all patients, a 20G intravenous cannula was secured, and they were premedicated with intravenous midazolam 0.03 mg/kg. Oxygen supplementation was given during the technique.
In group L (anatomical landmark), the patient is placed in the supine position with a slight degree of neck extension to facilitate identification of the hyoid bone. Once identified, under aseptic precautions a 24-gauge needle is embedded from the lateral side of the neck, pointing toward the greater cornu. After contact, the needle is separated from the bone inferiorly and advanced a few millimeters, it will penetrate the thyrohyoid membrane, and a “give” is felt. Injecting 1 mL of 2% lidocaine will block the internal branch of the superior laryngeal nerve cautious aspiration was performed before injection; this technique was repeated on the opposite side.
In group U (ultrasound-guided) (Sonosite Micromax-HFL linear 38 probes (6–13 MHz), the probe was placed in a sterile plastic sheath to keep sterility, then located on the submandibular area, recognizing the hyoid bone, which appears as a hyperechoic curved bright structure on ultrasound in the midline; the probe is moved laterally, and greater cornu of the hyoid bone can be seen as a bright structure medial to the superior laryngeal artery. The internal branch of the superior laryngeal nerve runs with the superior laryngeal artery just underneath the level of the greater cornu of the hyoid bone. Utilizing an in-plane method, a needle is passed perpendicular to the skin, directed below the greater cornu of the hyoid bone and 1ml lidocaine 2% was injected with a 24-gauge needle after negative aspiration (Fig. 1). The technique was repeated on the opposite side. A 3 mL of 2% lidocaine was injected through the cricothyroid membrane into the trachea in all patients.
Measurements
The primary outcome was to assess the excellence of airway anesthesia during intubation which was graded by a participant who was blinded to the anesthetic group assignment; the 5-point grading scale (Reasoner et al., 1995) was defined as follows:
-
0 = no coughing or gagging in response to fiber-optic manipulation
-
1 = mild coughing or gagging that did not prevent fiber-optic manipulation
-
2 = moderate coughing or gagging that opposed minimally
-
3 = severe coughing or gagging that made fiber-optic manipulation difficult
-
4 = very severe coughing or gagging that required additional local anesthetic and change in technique to achieve successful fiber-optic intubation.
The secondary outcomes were to evaluate patient awareness of pain and discomfort during fiber-optic intubation, time for intubation, and effects on hemodynamic variables.
Time to intubation was demarcated as the time between insertion of fiberscope through the mouth to the successful location of endotracheal tube and verification by the presence of end-tidal CO2. Effect on hemodynamic variables such as means arterial pressure (MAP), heart rate (HR), and oxygen saturation were documented before intubation as baseline values—also its peak value during intubation, and 1 min after intubation. Patient awareness of pain and discomfort during intubation was evaluated 12 h postoperatively using a numerical rating scale (NRS) (Jensen et al., 1986) (0–10 scale, with 0 being no discomfort and 10 being worst discomfort).
Statistical analysis
Recorded information was analyzed utilizing the statistical package for social sciences, version 20.0 (SPSS Inc., Chicago, Illinois, USA). Quantitative data were set as mean ± standard deviation (SD). Comparison of quantitative variables between the two study groups was done by using independent t test when the records were normally distributed and Mann-Whitney test in non-parametric data. Qualitative data were set as frequency and percentage, and the differences between the two groups were compared using the chi-square (χ2) test and/or Fisher’s exact test. The confidence interval was set to 95%, and the margin of error accepted was set to 5%. P < 0.05 was considered statistically significant. The sample size was determined utilizing the STATA program, based on previous studies (Ambi et al., 2017). The authors recruited 40 patients in 2 groups of 20 each to achieve a power of 0.8 and a type-1 error (alpha) of 0.05. We recruited 60 patients (30 patients for each group) to avoid possible dropout and to have a better power of study. The sample size was adequate with a power of 0.8 and a significance level of 0.05.
Results
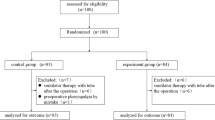
The total number of patients included was 60 with no dropouts. Figure 2 shows the joined values of reporting trials’ flow chart.
There were no significant demographic differences between both groups as regards age, sex, and ASA Physical Status (Table 1).
The quality of airway anesthesia during intubation was statistically significant with better outcomes in group U as compared to group L (Table 2).
The effect of tracheal intubation on HR was significantly higher in group L with a higher peak value (P value =0.017) during intubation and post-intubation peak values (P value=0.009) with reference to pre-intubation baseline value (P value =0.198) in contrast to group U (Table 3).
The effect of tracheal intubation on MAP was significantly higher in group L with a higher peak (P value=0.008) during intubation and post-intubation values (P value=0.006) with reference to pre-intubation baseline value (P value=0.106) in contrast to group U in (Table 3).
There was a statistically significant increase in the mean duration of intubation in group L compared to group U. The duration of tracheal intubation takes less time in group U (mean 61.52±9.79) as compared to group L (mean 97.28±30.70) (Table 4) because of the higher block success rate and quality of airway anesthesia. There was no difference between the groups as regards the success rate of intubation
There was a statistically significant lower perception of pain and discomfort during intubation assessed 12 h postoperatively based on numerical rating scales (NRS) with better patient tolerance in group U compared to group L (Table 4).
Discussion
When a difficult airway is foreseen, this should preferably be done under regional anesthesia which permits the patient to breathe spontaneously, keep up airway patency, and cooperate with the operator. If any difficulties are experienced, then the procedure can be abandoned with minimum risk to the patient.
There are several techniques described to anesthetize the trachea-bronchial tree. The likely preferences of utilizing ultrasound imaging for nerve blocks include a reduction in the amount of local anesthetic required, improved success rate, reduced time to perform the block, and diminished complication rate (Ambi et al., 2017).
In our study, we used ultrasound guidance for the block of the internal branch of the superior laryngeal nerve and compared it with the blind anatomical landmark.
The patient’s perception of discomfort and pain at the time of intubation evaluated postoperatively by numerical rating scale was significantly lower with better patient tolerance in the ultrasound group with a mean NRS score of 2.60±0.49 as compared to an anatomical group with a mean NRS score of 3.80±0.72 (P < 0.001). The requirement for profound palpation of hyoid bone and manipulation of the larynx in the anatomical group resulted in a higher patient perception of pain and discomfort at the time of intubation represented by a significantly higher numerical rating scale score in an anatomical group as compared to the ultrasound group. Similarly, a study by Wiles et al. (Wiles et al., 1989) concluded that deep palpation of the hyoid bone may be uncomfortable to the patients in addition to the hypotension and bradycardia which might be related to excessive manipulation of the larynx causing a vasovagal response.
In a study by Kundra et al. (Kundra et al., 2011), a combination of a bilateral block of superior laryngeal nerves with topical airway anesthesia was reported to produce better hemodynamic stability and patient comfort. However, in our study, hemodynamic stability was statistically significantly better in group U compared to group L, and there was no difference between the groups as regards the success rate of intubation, but there were significantly higher in gag reflex in an anatomical group compared to the ultrasound group.
A study was done by Chatrath and his colleagues (Chatrath et al., 2016), they have blocked the three significant reflexes of the patient including gag reflex, cough reflex, and glottis closure reflex by bilateral glossopharyngeal nerves block, bilateral superior laryngeal nerves block, and recurrent laryngeal nerves block, respectively. They concluded that combined regional nerve blocks give great intubating conditions, patient comfort, and security.
This study showed that the duration of intubation was shorter in the ultrasound group as compared to a blind anatomical group because of the higher block success rate and quality of airway anesthesia and better patient’s tolerance.
Manikandan et al. (Manikandan et al., 2010) described the first case reported for ultrasound-guided ibSLN block. They set the transducer in the transverse orientation and utilized an in-plane technique while performing an ibSLN block in a patient with a history of posterior cervical spine fixation. Under ultrasonography, the authors recognized the superior laryngeal artery and an internal branch of the superior laryngeal nerve, which advanced along with the superior laryngeal artery. They injected local anesthetic agents close to the superior laryngeal artery after negative aspiration of blood. Their report revealed that utilizing ultrasound in nerve block for conscious intubation takes less time to perform, with quicker onset, longer duration of action, and fewer complications.
Lan et al. (Lan et al., 2013) study the feasibility of ultrasound-guided ibSLN block utilizing fresh cadavers. They put the probe longitudinally over the submandibular area, and after identification of the greater horn of the hyoid bone and thyroid cartilage, 2 ml methylene blue dye was injected utilizing an out-of-plane method. Then, an anatomist dissected the tissue to decide whether the nerve was bathed in the dye. They concluded that ultrasound-guided nerve block was effective in 11 of 12 ibSLN cases.
Another study by Pintarič et al. (Pintarič et al., 2015) is that anatomical dissection was done utilizing an operating microscope in 5 cadaver heads, fixed in formalin, to expose the point of (ibSLN) piercing through the thyrohyoid membrane and stated that anatomically, the ibSLN was noticed in all formalin-preserved cadavers. Sonographically, the ibSLN was not seen, while the hyoid bone and the thyrohyoid membrane were seen in all cadavers. After the US-guided injection, the dye deposition was seen around the ibSLN in all cadaver specimens.
Using landmarks as a guide is reliable; in our study, the greater horn of the hyoid bone was used as a landmark to define SLN space, also, the pulse of the superior laryngeal artery which can be easily detected by using color Doppler and used as a surrogate to locate the position of the internal branch of superior laryngeal nerve with the probe placed longitudinally over the submandibular area.
Some clinicians have been unable to pinpoint the superior laryngeal nerve utilizing ultrasound imaging techniques. Barberry et al. (Barberey et al., 2010) and Vaghadia et al. (Vaghadia et al., 2011) agree that there may be initial difficulty to identify the superior laryngeal nerve, but in our study, we identified pulsations of the superior laryngeal artery (as a landmark in our block) by placing the ultrasound probe gently, because firm placement can compress the artery and distort the anatomy as the internal branch of the SLN is accompanied by the superior laryngeal artery so by following their relationship to the greater horn of hyoid bone blocking the ibSLN performed successfully. In agreement with our study, Manikandan et al. (Manikandan et al., 2010) described in their case reported that they succeed to perform ultrasound-guided ibSLN block. Another case was reported by Takafumi (Iida & Suzuki, 2012) in a patient prepared for drainage of a laryngeal abscess. They perform superior laryngeal nerve block (SLNB) under ultrasound guidance in an in-plane technique; they reported that ultrasound-guided SLNB can be another method for airway anesthesia when the anatomic landmark for SLNB procedure fails because it is difficult to palpate the hyoid bone due to swollen tissue.
Conclusions
For patients who are expected to have difficulty in intubation ultrasound-guided technique for the block of the internal branch of the superior laryngeal nerve as a part of the preparation of the airway to aid awake fiber-optic intubation provides excellent assistance in airway anesthesia and patient tolerance for intubation.
Availability of data and materials
The datasets used and/or analyzed during the current study are available for the corresponding author on reasonable request.
Abbreviations
- ASA:
-
American Society of Anesthesiologists’ physical status
- IbSLN:
-
Internal branch of superior laryngeal nerve
- SLN:
-
Superior laryngeal nerve
- HR:
-
Heart rate
- MAP:
-
Mean arterial pressure
- NRS:
-
Numerical rating scale
- SLNB:
-
Superior laryngeal nerve block
References
Ambi US, Arjun BK, Masur S, Endigeri A, Hosalli V, Hulakund SY (2017) Comparison of ultrasound and anatomical landmark-guided technique for superior laryngeal nerve block to aid awake fibre-optic intubation: a prospective randomised clinical study. Indian journal of anesthesia 61(6):463–468. https://doi.org/10.4103/ija.IJA_74_17
Barberey G, Henry Y, Boillot A, Pili-Floury S, Samain E (2010,October) Ultrasound imaging of the superior laryngeal nerve containing space. From Proceedings of the Annual Meeting of the American Society Anesthesiologists 16
Chatrath V, Sharan R, Jain P, Bala A, Ranjana S (2016) The efficacy of combined regional nerve blocks in awake orotracheal fiberoptic intubation. Anesth Essays Res 10:255–261
Furlan JC (2002) Anatomical study applied to anesthetic block technique of the superior laryngeal nerve. Acta anasthesiologica scandinavica 46(2):199–202
Takafumi Iida, Akihiro Suzuki, Takayuki Kunisawa, Hiroshi Iwasaki. Ultrasound-guided superior laryngeal nerve block and translaryngeal block for awake tracheal intubation in a patient with laryngeal abscess, Journal of Anesthesia 2012 27:309–331, 2, DOI: https://doi.org/10.1007/s00540-012-1492-5.
Jensen MP, Karoly P, Braver S (1986) The measurement of clinical pain intensity. A comparison of six methods of pain:117–126
Kundra P, Mishra SK, Ramesh A (2011) Ultrasound of the airway. Indian J Anasth. 55(5):456–462. https://doi.org/10.4103/0019-5049.89868
Lan CH, Cheng WC, Yang YL (2013) A new method for ultrasound-guided superior laryngeal nerve block. Tzu Chi Med J 25(3):161–163. https://doi.org/10.1016/j.tcmj.2013.05.001
Manikandan S, Neema PK, Rathod RC (2010) Ultrasound guided bilateral superior laryngeal nerve block to aid awake endotracheal intubation in a patient with cervical spine disease for emergency surgery. Anasth Intensive Care 38(5):9468–9948. https://doi.org/10.1177/0310057X1003800523
Pintarič TS, Kamen V V, Azman J, Cvetko E (2015) The thyro-hyoid membrane as a target for ultra-sound-guided block of the internal branch of the superior laryngeal nerve. Journal of Clinical Anesthesia 07:016
Ramkumar V (2011) Preparation of the patient and the airway for awake intubation. Indian J Anasth. 55(5):442–447. https://doi.org/10.4103/0019-5049.89863
Reasoner DK, Warner DS, Todd MM, Hunt SW, Kirchner J (1995) A comparison of anesthetic techniques for awake intubation in neurosurgical patients. J Neurosurg Anesthesiol 7(2):94–99. https://doi.org/10.1097/00008506-199504000-00004
Vaghadia H, Lawson R, Tang R, Sawka A (2011) Failure to visualize the superior laryngeal nerve using ultrasound imaging. Anaesth Intensive Care 39:503
Wiles JR, Kelly J, Mostafa SM (1989) Hypotension, and bradycardia following superior laryngeal nerve block. Br J Anaesth. 63(1):125–127. https://doi.org/10.1093/bja/63.1.125
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
ASME designed the study, revised the literature, followed the patients, and critically reviewed the manuscript. AMS designed the study, analyzed the data, and wrote and critically revised the manuscript. SMF and AME revised the literature, followed the patients, collected the data, performed the analysis, and wrote the manuscript. The authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Approval of the research ethical committee of the Faculty of Medicine, Ain Shams University, was obtained (code number: FMASU M S 19/2020), and written informed consent was obtained from all patients.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El Deek, A.M., Shafik, A.M., Eltohry, A.S.M.A. et al. Comparison between ultrasound-guided and anatomical landmark-guided block of internal branch of the superior laryngeal nerve for awake fiber-optic intubation in suspected difficult intubation: a randomized controlled study. Ain-Shams J Anesthesiol 13, 62 (2021). https://doi.org/10.1186/s42077-021-00181-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-021-00181-3