Abstract
Background
Animal studies have shown that nutritional exposures during pregnancy can modify epigenetic marks regulating fetal development and susceptibility to later disease, providing a plausible mechanism to explain the developmental origins of health and disease. Human observational studies have shown that maternal peri-conceptional diet predicts DNA methylation in offspring. However, a causal pathway from maternal diet, through changes in DNA methylation, to later health outcomes has yet to be established. The EMPHASIS study (Epigenetic Mechanisms linking Pre-conceptional nutrition and Health Assessed in India and Sub-Saharan Africa, ISRCTN14266771) will investigate epigenetically mediated links between peri-conceptional nutrition and health-related outcomes in children whose mothers participated in two randomized controlled trials of micronutrient supplementation before and during pregnancy.
Methods
The original trials were the Mumbai Maternal Nutrition Project (MMNP, ISRCTN62811278) in which Indian women were offered a daily snack made from micronutrient-rich foods or low-micronutrient foods (controls), and the Peri-conceptional Multiple Micronutrient Supplementation Trial (PMMST, ISRCTN13687662) in rural Gambia, in which women were offered a daily multiple micronutrient (UNIMMAP) tablet or placebo. In the EMPHASIS study, DNA methylation will be analysed in the children of these women (~1100 children aged 5–7 y in MMNP and 298 children aged 7–9 y in PMMST). Cohort-specific and cross-cohort effects will be explored. Differences in DNA methylation between allocation groups will be identified using the Illumina Infinium MethylationEPIC array, and by pyrosequencing top hits and selected candidate loci. Associations will be analysed between DNA methylation and health-related phenotypic outcomes, including size at birth, and children’s post-natal growth, body composition, skeletal development, cardio-metabolic risk markers (blood pressure, serum lipids, plasma glucose and insulin) and cognitive function. Pathways analysis will be used to test for enrichment of nutrition-sensitive loci in biological pathways. Causal mechanisms for nutrition-methylation-phenotype associations will be explored using Mendelian Randomization. Associations between methylation unrelated to supplementation and phenotypes will also be analysed.
Conclusion
The study will increase understanding of the epigenetic mechanisms underpinning the long-term impact of maternal nutrition on offspring health. It will potentially lead to better nutritional interventions for mothers preparing for pregnancy, and to identification of early life biomarkers of later disease risk.
Similar content being viewed by others
Background
EMPHASIS (Epigenetic Mechanisms linking Pre-conceptional nutrition and Health Assessed in India and Sub-Saharan Africa, www.emphasisstudy.org) is a collaboration between investigators in the UK, India and The Gambia designed to profile genome-wide DNA methylation in children whose mothers participated in two pre- and peri-conceptional micronutrient supplementation trials (the Mumbai Maternal Nutrition Project in India, MMNP [1] and the Peri-conceptional Multiple Micronutrient Supplementation Trial, PMMST, in rural Gambia [2]). The main objectives of the study are to identify methylation differences associated with the interventions and correlate these with health-related phenotypes in the children, including size at birth, post-natal growth, and childhood body composition, skeletal health, cardiometabolic risk markers and cognitive function. We hypothesise that maternal nutritional supplementation around the time of conception will result in altered DNA methylation profiles in the children, and that the distinct methylation patterns identified will show potentially causal associations with phenotypic characteristics in the children. We further expect to identify methylation differences unrelated to supplementation that are associated with the measured phenotypes.
Context
Poor quality diets and the resulting micronutrient deficiencies are major public health problems in low-and-middle-income countries (LMICs). In pregnant women they impair fetal development, and recent evidence suggests that they are also associated with longer term health problems in the offspring including stunting [3], impaired neurodevelopment [4] and, through ‘metabolic programming’, with increased vulnerability to adult non-communicable chronic diseases (NCDs) such as obesity, type 2 diabetes, cardiovascular disease and osteoporosis [5,6,7].
Long-term effects of fetal nutrition on later health would require mechanisms by which a ‘memory’ of the early environment is retained into later life and influences metabolism. Epigenetic signatures, including patterns of DNA methylation that are modifiable by environmental exposures, are leading candidate mechanisms [8, 9]. DNA methylation is a mitotically heritable epigenetic mark that plays a key role in the transcriptional regulation of cellular processes, including cell differentiation, genomic imprinting and X-chromosome inactivation. DNA methylation depends on the supply of methyl groups through the 1-carbon pathway, which requires vitamins B2, B6, B12, folate, methionine, choline and betaine, and amino acids serine and glycine, for normal function. The peri-conceptional period is a critical window when the process of establishing methylation marks is sensitive to nutrition [8, 9].
The initial ‘proof of principle’ of nutritional programming mediated by changes in DNA methylation came from the Agouti mouse model, in which natural variation in methylation at the Agouti locus influences coat colour, adult adiposity and glucose tolerance [8]. This locus is a metastable epiallele (ME), a genomic region characterised by inter-individual variation in methylation patterns that are established in the early embryo before gastrulation, and are therefore highly correlated across tissues derived from all three germ layers. Feeding pregnant dams ‘methyl donor’ nutrients (vitamin B12, folic acid, betaine and choline) increased methylation of the agouti locus and reduced agouti gene expression, leading to fewer obese yellow offspring and more lean brown offspring, characteristics that persisted into adult life [8]. Dietary manipulations in pregnancy affect the methylation and expression of offspring genes other than MEs. For example, in rats, maternal protein-restriction reduces methylation of offspring peroxisome proliferator activated receptor 1 alpha (PPARα) and glucocorticoid and angiotensin receptor genes [10]. Maternal folic acid supplementation prevents both the methylation and phenotypic effects (e.g. high blood pressure) induced by maternal protein restriction in the offspring.
There is evidence in humans that epigenetic changes induced by the nutritional environment in early life alter later phenotype, including body composition and cardiometabolic health. For example, DNA methylation at a number of loci (insulin-like growth factor 2 (IGF2), retinoid X receptor alpha (RXRA), endothelial nitric oxide synthase (eNOS), PGC1α, and cyclin-dependent kinase inhibitor 2 (CDKN2a) genes in cord tissue, cord blood or children’s leucocytes is associated with adiposity in later childhood [11,12,13,14]. Studies in The Gambia, where there is marked seasonal variation in maternal nutrition, have shown that season of conception is related to DNA methylation of human infant MEs [15], and that methylation is predicted by elements of the mother’s methyl donor metabolome at conception [16]. One implicated gene is the maternally imprinted tumour suppressor and immune function regulator vault RNA2–1 (VTRNA2–1) [17], making it a promising candidate for exploring mechanisms linking season of conception and infectious disease mortality in Gambians [18]. A methylation variant affecting expression of the pro-opio-melanocortin (POMC) gene has also been associated with child and adult obesity. This locus is an ME, and in Gambian infants methylation is associated with season of conception and maternal 1-carbon metabolites at conception [19].
Evidence for epigenetic programming in humans has hitherto relied mainly on observational studies. Randomised trials of peri-conceptional maternal nutritional interventions with follow-up of the children represent a stronger study design in which to examine effects on DNA methylation and health-related phenotypes, reducing the problems of confounding and bias that affect observational studies, thus providing stronger evidence of causality. The EMPHASIS study will be an important step towards understanding mechanisms underpinning the developmental origins of health and disease (DOHaD), identifying biomarkers of early life exposures associated with later disease risk, and designing more effective nutritional interventions for mothers preparing for pregnancy.
Design and methods
EMPHASIS is a follow-up study of two cohorts of children born to mothers who took part in separate randomized controlled trials of nutritional supplementation before and during pregnancy.
The original trials and the cohorts of children
Mumbai maternal nutrition project
MMNP (also known as Project SARAS [‘excellent’]; ISRCTN62811278) was a non-blinded individually randomized trial among Indian women living in Mumbai slums (2006–2012) [1]. The intervention was a daily snack, eaten in addition to normal diet, made from naturally micronutrient-rich local foods (green leafy vegetables, fruit and milk). Control snacks contained foods of low micronutrient content (e.g. potato, onion). Intervention snacks contained 10–23% of the WHO Reference Nutrient Intake (RNI) for β-carotene, vitamins B2 and B12, folate, calcium and iron, and 0.7 MJ of energy and 6 g of protein, compared with 0–7% RNI for the micronutrients, 0.4 MJ of energy and 2 g of protein in control snacks. At recruitment, non-pregnant women had detailed anthropometry, and data were collected on socio-economic status (Standard of Living Index [20]) and habitual diet by food frequency questionnaire. They received either intervention or control snacks; intake was supervised and recorded daily. Women who became pregnant continued supplementation until delivery, and were supplied with routine iron (100 mg) and folic acid (500 μg) supplements as per Indian government recommendations. Fetal biometry was recorded three times during pregnancy (at approximately 10, 20 and 29 weeks gestation, estimated from last menstrual period date and ultrasound measures) [21]. Plasma folate and vitamin B12 concentrations were measured in early pregnancy (~10 weeks gestation). An oral glucose tolerance test (WHO 1999 protocol) was performed at 28–32 weeks gestation [22]. Main outcomes were newborn anthropometry and gestational age at delivery. Of 6513 women recruited, 2291 became pregnant, leading to 1962 live singleton deliveries.
In the intention to treat analysis, there were no differences in birth weight or other newborn measurements between allocation groups [1]. In the per protocol analysis, limited to women who started supplementation at least 3 months before conception, a period that was considered long enough to achieve the maximal effect on maternal nutritional status, birth weight increased by a mean 48 g (p = 0.05). In both analyses there was an interaction between maternal BMI and the intervention, with a larger birth weight effect in mothers of BMI >18.5 kg/m2 (intention to treat: +63 g [95%CI 11, 115]; per protocol: +96 g [95%CI 35, 154]; p for interaction 0.001). The intervention reduced the prevalence of gestational diabetes (intention to treat: 7.3% compared with 12.4% in controls; OR: 0.56; 95% CI: 0.36, 0.86; P = 0.008) [22]. It had no effect on fetal size assessed using standard ultrasound measures [21].
The children of mothers who participated in MMNP are currently (2013–2018) being studied at 5–7 years of age (“SARAS KIDS” study) to measure anthropometry, body composition, skeletal development, cardio-metabolic risk markers and cognitive function (Fig. 1, Tables 1 and 2). Venous blood samples and buccal swabs are collected for DNA and RNA, and are stored in -80 °C freezers until transportation in batches to the laboratory on dry ice. The DNA samples and phenotype data will be used for the EMPHASIS study, in which we will limit the sample to the 1562 children born to mothers in the per protocol group. Data collection will be completed by the end of January 2018.
West kiang Peri-conceptional multiple micronutrient supplementation trial
PMMST (ISRCTN13687662) was a double-blind individually randomized trial among women living in rural West Kiang, The Gambia (2006–2008) [2] (Fig. 2). The intervention was a daily multiple micronutrient tablet (UNIMMAP) providing the RNI of vitamins A, B1, B2, niacin, B6, folic acid, B12, C, D and E and iron, zinc, copper, selenium and iodine [23]. Control women received matching placebo tablets. At recruitment, non-pregnant women had anthropometry. Compliance with supplementation was assessed by fortnightly tablet counts. Women stopped the supplement when they became pregnant, confirmed either by pregnancy test or by ultrasound at approximately 12 weeks gestation, and then both groups were supplied with routine iron (60 mg) and folic acid 250 μg) supplements and anti-malarial prophylaxis. Serial ultrasound scans were performed and newborn anthropometry was recorded. Primary outcomes were mid-gestation indices of utero-placental vascular-endothelial function (ratio of plasminogen-activator inhibitor [PAI] 1 to PAI-2), mean uterine-artery resistance index and fetal-to-maternal measles antibody ratio as an index of placental active transport capacity at delivery.
Of 1156 women recruited, 376 had live singleton deliveries. There were no differences in PAI-1/PAI-2 or measles antibody ratio between trial arms, but there was a 0.02-unit reduction in uterine artery resistance index between 18 and 32 weeks of gestation (95% CI: -0.03, −0.00; P = 0.040) among women in the intervention group [2]. There was no significant effect of supplementation on birth weight. Two small pilot studies subsequently identified preliminary evidence of intervention-associated methylation differences in cord blood DNA, and in peripheral blood at the age of 9 months [24, 25]; no analyses were conducted relating DNA methylation to phenotypes.
For EMPHASIS, we aimed to study as many as possible of the 376 children; 356 were re-traced using the West Kiang Demographic Surveillance System [26], 298 of these were studied during 2016–2017 at the age of 7–9 years (Fig. 2). Similar outcomes were measured as in MMNP, using harmonised methods (Table 2). Blood samples and buccal swabs were collected for DNA and RNA and stored at -80 °C; DNA was isolated in The Gambia and DNA samples were transported to the laboratory in India on dry ice.
DNA methylation profiling
DNA methylation profiling for both cohorts will be carried out at the CSIR-Centre for Cellular and Molecular Biology, Hyderabad, India. In a stage 1 ‘discovery’ analysis, genome-wide DNA methylation will be measured at >850,000 CpG methylation sites in ~700 Mumbai children and all the Gambian children with available DNA (N = 293) using the Illumina Infinium MethylationEPIC array (EPIC) (Illumina Inc., San Diego, USA), to identify differentially methylated positions (DMPs), regions (DMRs), and variably methylated positions and regions (VMPs and VMRs). Technical validation of significant DMPs and DMRs will be performed by pyrosequencing a subset of samples spanning the range of observed methylation values, using a Pyromark 96 pyrosequencer (Qiagen, Hilden, Germany). In addition, a small number of selected candidate loci not present on the EPIC array will also be assayed in both cohorts by pyrosequencing. These have been selected a priori following a literature review (manuscript in preparation) of other studies in which DNA methylation has been associated with maternal nutritional exposures and/or health outcomes of interest (Table 3). Replication of the technically validated loci will be performed using pyrosequencing in an independent sample of size n = 200–400 MMNP samples (sample size will depend on the observed effect size in the discovery analysis). In a cross-tissue analysis, technically validated significant loci will be examined in buccal DNA samples (n~50 from each cohort). All samples from both cohorts will also be genotyped using the Illumina Global Screening Array (GSA). Blood samples collected into Paxgene tubes for RNA isolation will be stored for later transcriptomic studies.
Data analysis
A detailed analysis plan can be found on the EMPHASIS website (www.emphasisstudy.org).
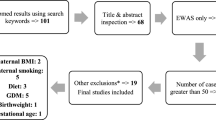
Stage 1: Intervention-methylation associations (Fig. 3 ): Data from the two cohorts will be analysed separately. In a ‘hypothesis-free’, genome-wide analysis, the raw intensity data from the EPIC arrays will undergo pre-processing, quality control and normalization. Intervention-methylation associations will be identified at DMRs and DMPs using appropriate methods, and controlling for the false discovery rate (FDR). Loci and regions showing differences in methylation variance (VMPs and VMRs) will be identified, both genome wide and in an analysis targeted to MEs and imprinting control regions (ICRs). The candidate gene data will be analysed in parallel, using a similar strategy to the one outlined above to identify methylation differences associated with nutritional intervention. Technical validation will be carried out in a sub-set (10%) of samples using pyrosequencing. Significant hits will be those with p value <0.05 after correction for multiple testing. For the cross-tissue analysis, correlations of blood versus buccal methylation will be assessed using Pearson correlations.
Statistical power is estimated based on a sample size of 700 in the Indian cohort and 293 in The Gambia, to detect DMPs at a single locus using two-sample t-tests with alpha = 0.05, using a conservative assumption that tested loci have a methylation standard deviation at the 95th percentile of those observed (ie. within the 5% most variable probes). Significance thresholds were Bonferroni-adjusted assuming 800,000 independent tests, allowing for some filtering of probes. We estimate that we will be able to detect mean methylation differences between intervention and control groups, with 80% power, of 3 and 5% in the Indian and Gambian cohorts respectively. For the replication study using pyrosequencing in independent samples from the Indian cohort, and in the candidate loci studies in both cohorts, we estimate 80% power to detect a 2% difference in the Indian cohort and 3% in the Gambian cohort.
Stage 2: Methylation-outcome associations (Figs. 4 and 5 , Table 4 ): Significant loci associated with the nutritional intervention in either cohort from the EPIC array analysis, and all candidate loci, will be tested for associations with phenotype data measured in the children at the time of DNA collection, and also with birth outcomes (newborn anthropometry and gestation) (Table 4, Fig. 4). Loci identified in a separate meta-analysis of Stage 1 associations across both cohorts will also be considered. We will additionally carry out a ‘hypothesis-free’ analysis to identify loci where methylation is associated with outcomes, irrespective of intervention-methylation associations (Fig. 5).
Other analyses
To gain insights into underlying mechanisms, gene pathways analysis will be performed for the intervention-methylation-outcome genome wide association analysis. We will compare results from the intervention-methylation, methylation-outcome, and pathways analyses between the cohorts to identify commonalities and differences and explore further opportunities for meta-analysis. We will examine potential single nucleotide polymorphism (SNP) effects on methylation through methylation Quantitative Trait Loci (mQTL) analysis using the genome-wide genotype data on the children. We will also consider options for performing causal analysis with generated genotype data using Mendelian Randomisation (MR) [27,28,29].
DNA methylation assays for the discovery sample of Mumbai children and all of the Gambian children are scheduled to be completed in late 2017. Assays for the replication sample of Mumbai children will be completed in early 2018. The full EMPHASIS analysis (Stages 1 and 2) will be completed by mid-late 2018.
Discussion
EMPHASIS is the first study in humans to examine the effects of maternal pre- and peri-conceptional nutrition on genome wide DNA methylation in children in a randomized controlled trial setting and to relate nutrition-related DNA methylation to a range of health outcomes. Recent technical advances offer the ability to study the methylome at high resolution and affordable cost. This gives us an unprecedented opportunity to investigate the effects of nutrition on methylation at a critical period (peri-conception), when the epigenome undergoes extensive remodelling. Most previous studies investigating these effects in humans have been observational, with limited scope for causal inference due to issues of confounding and reverse causality, or are quasi-experimental (eg famine studies) with imprecise exposure measures and/or large losses to follow-up. EMPHASIS is a unique opportunity to test the developmental origins of health and disease (DOHaD) hypothesis [5, 6, 9] and its underlying mechanisms.
The two-country design has strong advantages. Findings replicated in both cohorts will provide persuasive evidence for globally-relevant mechanisms with implications for policy. Differences between the cohorts will delineate some of the complex interrelationships between ethnicity, environment, nutrition and epigenetics, highlighting important context-specific factors. The two trials have commonalities and differences. The intervention comprised multiple micronutrients in both (from foods in MMNP and tablets in PMMST); the quantities of micronutrients were about fourfold higher in PMMST, while the MMNP food-based supplements provided some nutrients not present in the tablets used in PMMST (e.g. fatty acids). The timing of the intervention differed (continued throughout pregnancy in MMNP, stopped in early pregnancy in PMMST). The baseline nutritional status of the populations differed (the mothers in India were thinner and shorter, and the babies more growth restricted, than in PMMST (Table 2)). Vitamin B12 deficiency is common in India but not in The Gambia; and seasonal variation in diets is more marked in West Kiang than in Mumbai. We therefore expect the findings to reflect these commonalities and differences, revealing both shared and cohort-specific effects.
Evidence of cross-tissue, genotype-independent stochastic variation in DNA methylation at nutrition-associated loci will provide strong evidence that these loci are MEs, programmed in the early embryo. Evidence of nutrition-related epigenetic programming at peri-conception with the potential to influence gene expression in multiple tissue types would be an important finding. Methylation data from two tissues of different developmental origin will give further information about their stability across populations. The potential utility of buccal cells to measure epigenetic changes will in future allow non-invasive testing at multiple points in the lifecourse and relationships with disease progression to be followed.
High resolution genomic data will enable the investigation of potential confounding effects due to mQTL, genetic variants that influence methylation [30,31,32,33,34]. This may be particularly relevant for cross-cohort replication where differences in genetic background between cohorts should be taken into account. The mQTL can also be used as genetic instruments for causal analysis using MR [27,28,29]. Our study design is particularly well suited for ‘two-sample’ MR where instruments (mQTL) are identified in one sample, and analysed for their association with phenotype in the other. A related and particularly powerful approach is to use existing large genome wide association study (GWAS) datasets with relevant phenotypes and a similar genetic background as the second cohort in a two-sample MR analysis.
A limitation of EMPHASIS is the relatively small size of the Gambian sample, reducing the power to detect small methylation changes. The lack of perinatal DNA samples, in both cohorts, for methylation assays makes it more difficult to establish evidence for the direction of causality when correlating methylation with birth outcomes, although causal analysis would be expected to help to in this respect.
South Asian and sub-Saharan African countries stand out on the world map of maternal undernutrition and micronutrient deficiencies, low birth weight and childhood stunting [35]. Despite large investment in supplementation programmes for pregnant women there has been slow progress in reducing intra-uterine growth restriction and stunting. The evidence that adult non-communicable disease (NCD) risk is increased by fetal and infant under-nutrition suggests that these persistent problems contribute to the high and rising burden of NCDs in these countries [36, 37]. EMPHASIS will improve understanding of the biology linking maternal nutrition to fetal development and later health, potentially leading to better interventions.
Abbreviations
- BA:
-
Bone area
- BMAD:
-
Bone mineral apparent density
- BMC:
-
Bone mineral content
- BMD:
-
Bone mineral density
- BMI:
-
Body mass index
- CDC:
-
Centers for disease control and prevention
- CpG:
-
Cytosine (phosphate) guanine di-nucleotide
- CSIR:
-
Council of Scientific and Industrial Research, India
- DMP:
-
Differentially methylated position
- DMR:
-
Differentially methylated region
- DOHaD:
-
Developmental origins of health and disease
- DXA:
-
Dual-energy X-ray absorptiometry
- EMPHASIS:
-
Epigenetic mechanisms linking pre-conceptional nutrition and health assessed in india and Sub-Saharan Africa
- EPIC:
-
Illumina Infinium methylationEPIC beadChip
- FDR:
-
False discovery rate
- GSA:
-
Illumina global screening array
- GWAS:
-
Genome wide association study
- HDL:
-
High density lipoprotein
- HOMA-IR:
-
Homeostasis model assessment – insulin resistance
- ICR:
-
Imprinting control region
- LDL:
-
Low density lipoprotein
- LMICs:
-
Low- and middle-income countries
- ME:
-
Metastable epiallele
- MMNP:
-
Mumbai maternal nutrition project (Mumbai, India)
- mQTL:
-
Methylation quantitative trait loci
- MR:
-
Mendelian randomization
- NCD:
-
Non-communicable chronic disease
- PAI:
-
Plasminogen activator inhibitor
- PMMST:
-
Peri-conceptional multiple micronutrient supplementation trial (The Gambia)
- pQCT:
-
Peripheral quantitative computed tomography
- RNA:
-
Ribonucleic acid
- RNI:
-
Reference nutrient intake, sufficient to meet the needs of >97% of people
- SGA:
-
Small for gestational age
- SNP:
-
Single nucleotide polymorphism
- UNIMMAP:
-
United nations multiple micronutrient preparation
- vBMD:
-
Volumetric bone mineral density
- VMP:
-
Variably methylated position (differential variance in methylation)
- VMR:
-
Variably methylated region (differential variance in methylation)
- WHO:
-
World Health Organization
References
Potdar RD, Sahariah SA, Gandhi M, Kehoe SH, Brown N, Sane H, Dayama M, Jha S, Lawande A, Coakley PJ, Marley-Zagar E, Chopra H, Shivshankaran D, Chheda-Gala P, Muley-Lotankar P, Subbulakshmi G, Wills AK, Cox VA, Taskar V, DJP B, Jackson AA, Margetts BM, CHD F. Improving women’s diet quality pre-conceptionally and during gestation: effects on birth weight and prevalence of low birth weight; a randomized controlled efficacy trial in India (Mumbai maternal nutrition project). Am J Clin Nutr. 2014;100:1257–68.
Owens S, Gulati R, Fulford AJ, Sosseh F, Denison FC, Brabin BJ, Prentice AM. Periconceptional multiple-micronutrient supplementation and placental function in rural Gambian women: a double-blind, randomized, placebo-controlled trial. Am J Clin Nutr. 2015;102:1450–9.
Bhutta ZA, Das JK, Rizvi A, Gaffey MF, Walker N, Horton S, Webb P, Lartey A, Black RE, and the Lancet Nutrition Interventions Review Group, and the Maternal and Child Nutrition Study Group. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet. 2013;382:452–77.
Britto PR, Lye SJ, Proulx K, Yousafzai AK, Matthews SG, Vaivada T, Perez-Escamilla R, Rao N, Ip P, LCH F, MacMillan H, Hanson M, Wachs TD, Yao H, Yoshikawa H, Cerezo A, Leckman JF, Bhutta ZA, and the Early Childhood Development Interventions Review Group, for the Lancet Early Childhood Development Series Steering Committee. Nurturing care: promoting early childhood development. Lancet. 2017;389:91–102.
Barker DJ, Gluckman PD, Godfrey KM, Harding JE, Owens JA, Robinson JS. Fetal nutrition and cardiovascular disease in adult life. Lancet. 1993;341:938–41.
Sutton EF, Gilmore LA, Dunger DB, Heijmans BT, Hivert MF, Ling C, Martinez JA, Ozanne SE, Simmons RA, Szyf M, Waterland RA, Redman LM, Ravussin E. Developmental programming: state-of-the-science and future directions. Obesity (Silver Spring). 2016;24:1018–26.
Ganpule A, Yajnik CS, Fall CH, Rao S, Fisher DJ, Kanade A, Cooper C, Naik S, Joshi N, Lubree H, Deshpande V, Joglekar C. Bone mass in Indian children--relationships to maternal nutritional status and diet during pregnancy: the Pune maternal nutrition study. J Clin Endocrinol Metab. 2006;91:2994–3001.
Waterland RA, Michels KB. Epigenetic epidemiology of the developmental origins hypothesis. Ann Rev Nutr. 2007;27:363–88.
Burdge GC, Lillycrop KA. Nutrition, epigenetics, and developmental plasticity: implications for understanding human disease. Ann Rev Nutr. 2010;30:315–39.
Lillycrop KA, Phillips ES, Jackson AA, Hanson MA, Burdge GC. Dietary protein restriction of pregnant rats induces and folic acid supplementation prevents epigenetic modification of hepatic gene expression in the offspring. J Nutr. 2005;135:1382–6.
Perkins E, Murphy SK, Murtha AP, Schildkraut J, Jirtle RL, Demark-Wahnefried W, Forman MR, Kurtzberg J, Overcash F, Huang Z, Hoyo C. Insulin-like growth factor 2/H19 methylation at birth and risk of overweight and obesity in children. J Pediatrics. 2012;161:31–9.
Godfrey KM, Sheppard A, Gluckman PD, Lillycrop KA, Burdge GC, McLean C, Rodford J, Slater-Jefferies JL, Garratt E, Crozier SR, Emerald BS, Gale CR, Inskip HM, Cooper C, Hanson MA. Epigenetic gene promoter methylation at birth is associated with child's later adiposity. Diabetes. 2011;60:1528–34.
Clarke-Harris R, Wilkin TJ, Hosking J, Pinkney J, Jeffery AN, Metcalf BS, Godfrey KM, Voss LD, Lillycrop KA, Burdge GC. Peroxisomal proliferator activated receptor-gamma-co-activator-1alpha promoter methylation in blood at 5-7 years predicts adiposity from 9 to 14 years (EarlyBird 50). Diabetes. 2014;63:2528–37.
Lillycrop K, Murray R, Cheong C, Teh AL, Clarke-Harris R, Barton S, Costello P, Garratt E, Cook E, Titcombe P, Shunmuganathan B, Liew SJ, Chua Y-C, Lin X, Wu Y, Burdge GC, Cooper C, Inskip HM, Karnani N, Hopkins JC, Childs CE, Chavez CP, Calder PC, Yap F, Lee YS, Chong YS, Melton PE, Beilin L, Huang R-C, Gluckman PD, Harvey N, Hanson MA, Holbrook JD, the EpiGen Consortium, Godfrey KM. ANRIL promoter DNA methylation: a perinatal marker for later adiposity. EBiomed. 2017;19:60–72.
Waterland RA, Kellermayer R, Laritsky E, Rayco-Solon P, Harris RA, Travisano M, Zhang W, Torskaya MS, Zhang J, Shen L, Manary MJ, Prentice AM. Season of conception in rural gambia affects DNA methylation at putative human metastable epialleles. PLoS Genet. 2010;6:e1001252. doi: 10.1371/journal.pgen.1001252.
Dominguez-Salas P, Moore SE, Baker MS, Bergen AW, Cox SE, Dyer RA, Fulford AJ, Guan Y, Laritsky E, Silver MJ, Swan GE, Zeisel SH, Innis SM, Waterland RA, Prentice AM, Hennig BJ. Maternal nutrition at conception modulates DNA methylation of human metastable epialleles. Nat Commun. 2014;29(5):3746. doi: 10.1038/ncomms4746.
Silver MJ, Kessler NJ, Hennig BJ, Dominguez-Salas P, Laritsky E, Baker MS, Coarfa C, Hernandez-Vargas H, Castelino JM, Routledge MN, Gong YY, Herceg Z, Lee YS, Lee K, Moore SE, Fulford AJ, Prentice AM, Waterland RA. Independent genomewide screens identify the tumor suppressor VTRNA2-1 as a human epiallele responsive to periconceptional environment. Genome Biol. 2015;16:118. doi: 10.1186/s13059-015-0660-y.
Moore SE, Cole TJ, Poskitt EM, Sonko BJ, Whitehead RG, McGregor IA, Prentice AM. Season of birth predicts mortality in rural Gambia. Nature. 1997;388:434.
Kühnen P, Handke D, Waterland RA, Hennig BJ, Silver M, Fulford AJ, Dominguez-Salas P, Moore SE, Prentice AM, Spranger J, Hinney A, Hebebrand J, Heppner FL, Walzer L, Grötzinger C, Gromoll J, Wiegand S, Grüters A, Krude H. Interindividual variation in DNA methylation at a putative POMC metastable epiallele is associated with obesity. Cell Metab. 2016;24:502–9.
International Institute for Population sciences (IIPS) and Operations Research Centre (ORC) Macro. National Family Health survey (NFHS-2), India, 1998–99: Maharashtra. Mumbai: IIPS; 2001.
Lawande A, Di Gravio C, Potdar RD, Sahariah SA, Gandhi M, Chopra H, Sane H, Kehoe SH, Marley-Zagar E, Margetts BM, Jackson AA, Fall CHD. Effect of a micronutrient-rich snack taken pre-conceptionally and throughout pregnancy on ultrasound measures of fetal growth: the Mumbai maternal nutrition project (MMNP). Mat Child Nutr. 2017 (e-pub; doi: 10.1111/mcn.12441.
Sahariah SA, Potdar RD, Gandhi M, Kehoe SH, Brown N, Sane H, Coakley PJ, Marley-Zagar E, Chopra H, Shivshankaran D, Cox VA, Jackson AA, Margetts BM, Fall CHD. A daily snack containing green leafy vegetables, fruit and milk before and during pregnancy prevented gestational diabetes in a randomized controlled trial in Mumbai. India J Nutr. 2016;146(Suppl):1453S–60S.
World Health Organization and Food and Agriculture Organization of the United Nations. Vitamin and mineral requirements in human nutrition (2nd edition). Report of a joint FAO/WHO expert consultation. Rome: Food and Agriculture Organization; 2004.
Cooper WN, Khulan B, Owens S, Elks CE, Seidel V, Prentice AM, Belteki G, Ong KK, Affara NA, Constância M, Dunger DB. DNA methylation profiling at imprinted loci after periconceptional micronutrient supplementation in humans: results of a pilot randomized controlled trial. FASEB J. 2012;26:1782–90.
Khulan B, Cooper WN, Skinner BM, Bauer J, Owens S, Prentice AM, Belteki G, Constancia M, Dunger D, Affara NA. Periconceptional maternal micronutrient supplementation is associated with widespread gender related changes in the epigenome: a study of a unique resource in the Gambia. Hum Mol Genet. 2012;21:2086–101.
Hennig BJ, Unger SA, Dondeh BL, Hassan J, Hawkesworth S, Jarjou L, Jones KS, Mooe SE, Nabwera HM, Ngum M, Prentice A, Sonko B, Prentice AM, Fulford AJ. Cohort profile: the KiangWest longitudinal population study (KWLPS)—a platform for integrated research and health care provision in rural Gambia. Int J Epidemiol. 2015; doi: 10.1093/ije/dyv206.
Relton CL, Davey SG. Two-step epigenetic Mendelian randomization: a strategy for establishing the causal role of epigenetic processes in pathways to disease. Int J Epidemiol. 2012;41:161–76.
Relton CL, Davey SG. Mendelian randomization: applications and limitations in epigenetic studies. Epigenomics. 2015;7:1239–43.
Lawlor D, Commentary A. Two-sample Mendelian randomization: opportunities and challenges. Int J Epidemiol. 2016;45:908–15.
Teh AL, Pan H, Chen L, Ong ML, Dogra S, Wong J, MacIsaac JL, Mah SM, McEwen LM, Saw SM, Godfrey KM, Chong YS, Kwek K, Kwoh CK, Soh SE, Chong MF, Barton S, Karnani N, Cheong CY, Buschdorf JP, Stünkel W, Kobor MS, Meaney MJ, Gluckman PD, Holbrook JD. The effect of genotype and in utero environment on interindividual variation in neonate DNA methylomes. Genome Res. 2014;24:1064–74.
Gaunt TR, Shihab HA, Hemani G, Min JL, Woodward G, Lyttleton O, Zheng J, Duggirala A, McArdle WL, Ho K, Ring SM, Evans DM, Davey Smith G, Relton CL. Systematic identification of genetic influences on methylation across the human life course. Genome Biol. 2016;17:61. doi: 10.1186/s13059-016-0926-z.
Hoffmann A, Ziller M, Spengler D. The future is the past: Methylation QTLs in schizophrenia. Genes. 2016;7:E104.
Banovich NE, Lan X, McVicker G, van de Geijn B, Degner JF, Blischak JD, Roux J, Pritchard JK, Gilad Y. Methylation QTLs are associated with coordinated changes in transcription factor binding, histone modifications, and gene expression levels. PLoS Genet. 2014;10:e1004663.
Gibbs JR, van der Brug MP, Hernandez DG, Traynor BJ, Nalls MA, Lai SL, Arepalli S, Dillman A, Rafferty IP, Troncoso J, Johnson R, Zielke HR, Ferrucci L, Longo DL, Cookson MR, Singleton AB. Abundant quantitative trait loci exist for DNA methylation and gene expression in human brain. PLoS Genet. 2010;6:e1000952.
Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, Ezzati M, Grantham-McGregor S, Katz J, Martorell R, Uauy R. Maternal and child nutrition study group. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–51.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: pooled analysis of 751 population-based measurement studies with over 4.4 million participants. Lancet. 2016;387:1513–30.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1,479 population-based measurement studies with 19.1 million participants. Lancet. 2017;7(389):37–55.
Kaufman AS, Kaufman LN. Kaufman assessment battery for children, second edition: manual. Circle Pines: AGS Publishing; 2004.
Korkman M, Kemp SL, Kirk U. Effects of age on neurocognitive measures of children ages 5 to 12: a cross-sectional study on 800 children from the United States. Dev Neuropsychol. 2001;20:331–54.
Kohs SC. Intelligence measurement: a psychological and statistical study based upon the block-design test. New York: Macmillan; 1923.
Wechsler D. Manual for the Wechsler intelligence scale for children. 3rd ed. San Antonio: Psychological Corporation; 1991.
Lillycrop KA, Costello PM, Teh AL, Murray RJ, Clarke-Harris R, Barton SJ, Garratt ES, Ngo S, Sheppard AM, Wong J, Dogra S, Burdge GC, Cooper C, Inskip HM, Gale CR, Gluckman PD, Harvey NC, Chong YS, Yap F, Meaney MJ, Rifkin-Graboi A, Holbrook JD, Epigen Global Research Consortium, Godfrey KM. Association between perinatal methylation of the neuronal differentiation regulator HES1 and later childhood neurocognitive function and behaviour. Int J Epidemiol. 2015;44:1263–76.
Harvey NC, Lillycrop KA, Garratt E, Sheppard A, McLean C, Burdge G, Slater-Jefferies J, Rodford J, Crozier S, Inskip H, Emerald BS, Gale CR, Hanson M, Gluckman P, Godfrey K, Cooper C. Evaluation of methylation status of the eNOS promoter at birth in relation to childhood bone mineral content. Calcif Tissue Int. 2012;90:120–7.
Peter CJ, Fischer LK, Kundakovic M, Garg P, Jakovcevski M, Dincer A, Amaral AC, Ginns E, Galdzicka M, Bryce CP, Ratner C, Waber DP, Mokler D, Medford G, Champagne FA, Rosene DL, McGaughy JA, Sharp AJ, Galler JR, Akbarian S. DNA Methylation signatures of early childhood malnutrition associated with impairments in attention and cognition. Biol Psychiatry. 2016;80:765–74.
Wilmot B, Fry R, Smeester L, Musser ED, Mill J, Nigg JT. Methylomic analysis of salivary DNA in childhood ADHD identifies altered DNA methylation in VIPR2. J Child Psychol Psychiatry. 2016;57:152–60.
Harvey NC, Sheppard A, Godfrey KM, McLean C, Garratt E, Ntani G, Davies L, Murray R, Inskip HM, Gluckman PD, Hanson MA, Lillycrop KA, Cooper C. Childhood bone mineral content is associated with methylation status of the RXRA promoter at birth. J Bone Miner Res. 2014;29:600–7.
Hoyo C, Murtha AP, Schildkraut JM, Jirtle RL, Demark-Wahnefried W, Forman MR, Iversen ES, Kurtzberg J, Overcash F, Huang Z, Murphy SK. Methylation variation at IGF2 differentially methylated regions and maternal folic acid use before and during pregnancy. Epigenetics. 2011;6:928–36.
Steegers-Theunissen RP, Obermann-Borst SA, Kremer D, Lindemans J, Siebel C, Steegers EA, Slagboom PE, Heijmans BT. Periconceptional maternal folic acid use of 400 μg per day is related to increased methylation of the IGF2 gene in the very young child. PLoS One. 2009;4:e7845. doi: 10.1371/journal.pone.0007845.
Heijmans BT, Tobi EW, Stein AD, Putter H, Blauw GJ, Susser ES, Slagboom PE, Lumey LH. Persistent epigenetic differences associated with prenatal exposure to famine in humans. Proc Natl Acad Sci U S A. 2008;105:17046–9.
Hoyo C, Daltveit AK, Iversen E, Benjamin-Neelon SE, Fuemmeler B, Schildkraut J, Murtha AP, Overcash F, Vidal AC, Wang F, Huang Z, Kurtzberg J, Seewaldt V, Forman M, Jirtle RL, Murphy SK. Erythrocyte folate concentrations, CpG methylation at genomically imprinted domains, and birth weight in a multiethnic newborn cohort. Epigenetics. 2014;9:1120–30.
Villar J, Cheikh Ismail L, Victora CG, Ohuma EO, Bertino E, Altman DG, Lambert A, Papageorghiou AT, Carvalho M, Jaffer YA, Gravett MG, Purwar M, Frederick IO, Noble AJ, Pang R, Barros FC, Chumlea C, Bhutta ZA, Kennedy SH. International fetal and newborn growth consortium for the 21st century (INTERGROWTH-21st). International standards for newborn weight, length, and head circumference by gestational age and sex: the newborn cross-sectional study of the INTERGROWTH-21st project. Lancet. 2014;384:857–68.
Utzschneider KM, Prigeon RL, Faulenbach MV, Tong J, Carr DB, Boyko EJ, Leonetti DL, McNeely MJ, Fujimoto WY, Kahn SE. Oral disposition index predicts the development of future diabetes above and beyond fasting and 2-h glucose levels. Diabetes Care. 2009;32:335–41.
Phillips DI, Clark PM, Hales CN, Osmond C. Understanding oral glucose tolerance: comparison of glucose or insulin measurements during the oral glucose tolerance test with specific measurements of insulin resistance and insulin secretion. Diabetic Med. 1994;11:286–92.
Acknowledgements
We thank the parents and children in India and The Gambia for participating, and field teams in both centres. We are grateful to our partners and advisors Caroline Relton (Steering Committee Chair), Partha Majumdar and Frank Dudbridge (Steering Committee members).
The EMPHASIS study group includes:
Lena Acolatse, MRC Unit The Gambia lenaacolatse@gmail.com; Meraj Ahmed, CSIR-Centre for Cellular and Molecular Biology, Hyderabad, India meraj@ccmb.res.in; Modupeh Betts, MRC Unit The Gambia mbetts@mrc.gm; Giriraj R Chandak, CSIR-Centre for Cellular and Molecular Biology, Hyderabad, India chandakgrc@ccmb.res.in; Harsha Chopra, Centre for the Study of Social Change, Mumbai, India harshac3@gmail.com; Cyrus Cooper, MRC Lifecourse Epidemiology Unit, University of Southampton, UK cc@mrc.soton.ac.uk; Momodou K Darboe, MRC Unit The Gambia mdarboe@mrc.gm; Chiara Di Gravio, MRC Lifecourse Epidemiology Unit, University of Southampton, UK cdg@mrc.soton.ac.uk; Caroline HD Fall, MRC Lifecourse Epidemiology Unit, University of Southampton, UK chdf@mrc.soton.ac.uk; Meera Gandhi, Centre for the Study of Social Change, Mumbai, India mira_gandhi@rediffmail.com; Gail R Goldberg, MRC Elsie Widdowson Laboratory, Cambridge, UK Gail.Goldberg@mrc-ewl.cam.ac.uk; Prachand Issarapu, CSIR-Centre for Cellular and Molecular Biology, Hyderabad, India prachand@ccmb.res.in; Philip James, MRC Unit, The Gambia and MRC International Nutrition Group, London School of Hygiene and Tropical Medicine, UK philip.james@lshtm.ac.uk; Ramatoulie Janha, MRC Unit The Gambia rjanha@mrc.gm; Landing MA Jarjou, MRC Unit The Gambia ljarjou@mrc.gm; Lovejeet Kaur, CSIR-Centre for Cellular and Molecular Biology, Hyderabad, India lovejeetkaur@ccmb.res.in; Sarah H Kehoe, MRC Lifecourse Epidemiology Unit, University of Southampton, UK sk@mrc.soton.ac.uk; Kalyanaraman Kumaran, MRC Lifecourse Epidemiology Unit, University of Southampton, UK and CSI Holdsworth Memorial Hospital, Mysore, India kk@mrc.soton.ac.uk; Karen A Lillycrop, University of Southampton, UK K.A.Lillycrop@soton.ac.uk; Mohammed Ngum, MRC Unit The Gambia mngum@mrc.gm; Suraj S Nongmaithem, CSIR-Centre for Cellular and Molecular Biology, Hyderabad, India suraj.nong@ccmb.res.in; Stephen Owens, Newcastle University Trust Hospital, UK Stephen.Owens@nuth.nhs.uk; Ramesh D Potdar, Centre for the Study of Social Change, Mumbai, India rdpotdar@snehamrc.com; Andrew M Prentice, MRC Unit, The Gambia and MRC International Nutrition Group, London School of Hygiene and Tropical Medicine, UK Andrew.Prentice@lshtm.ac.uk; Ann Prentice, MRC Unit, The Gambia, Elsie Widdowson Laboratory, Cambridge, UK and MRC Lifecourse Epidemiology Unit, University of Southampton Ann.prentice@mrc-ewl.cam.ac.uk; Tallapragada Divya Sri Priyanka, CSIR-Centre for Cellular and Molecular Biology, Hyderabad, India priyankapragada@ccmb.res.in; Ayden Saffari, MRC Unit, The Gambia and MRC International Nutrition Group, London School of Hygiene and Tropical Medicine, UK Ayden.Saffari@lshtm.ac.uk; Sirazul Ameen Sahariah, Centre for the Study of Social Change, Mumbai, India drsahariah@yahoo.com; Sara Sajjadi, CSIR-Centre for Cellular and Molecular Biology, Hyderabad, India sara.sajjadi@ccmb.res.in; Harshad Sane, Centre for the Study of Social Change, Mumbai, India datamanager@snehamrc.com; Smeeta Shrestha, CSIR-Centre for Cellular and Molecular Biology, Hyderabad, India smeeta@ccmb.res.in; Matt J Silver, MRC Unit The Gambia and MRC International Nutrition Group, London School of Hygiene and Tropical Medicine, UK matt.silver@lshtm.ac.uk; Ashutosh Singh Tomar, CSIR-Centre for Cellular and Molecular Biology, Hyderabad, India ashutosh.tomar87@ccmb.res.in; Kate A Ward, MRC Elsie Widdowson Laboratory, Cambridge and MRC Lifecourse Epidemiology Unit, University of Southampton, UK kate.ward@mrc-ewl.cam.ac.uk; Dilip Kumar Yadav, CSIR-Centre for Cellular and Molecular Biology, Hyderabad, India dilip@ccmb.res.in; Chittaranjan S Yajnik, Diabetes Unit, KEM Hospital and Research Centre, Pune, India csyajnik@hotmail.com
Funding
MMNP was funded by the Wellcome Trust, Parthenon Trust, ICICI Bank Ltd., Mumbai, the UK Medical Research Council (MRC) and the UK Department for International Development (DFID) under the MRC/DFID Concordat. The children’s follow-up is funded by MRC (MR/M005186/1). PMMST was supported by MRC (U1232661351, U105960371 and MC-A760-5QX00) and DFID under the MRC/DFID Concordat, and other members of the Gambian team are supported by MRC grants U105960371, U123261351 and U123261351. The EMPHASIS study is jointly funded by MRC, DFID and the Department of Biotechnology (DBT), Ministry of Science and Technology, India under the Newton Fund initiative (MRC grant no.: MR/N006208/1 and DBT grant no.: BT/IN/DBT-MRC/DFID/24/GRC/2015–16). The funding bodies played no role in the design of the study and collection, analysis, interpretation of data or writing the manuscript.
Availability of data and materials
Data collection is ongoing in Mumbai and will be completed in early 2018. The analysis plan is available on the study website (www.emphsisstudy.org). Participant information sheets, and study instruments/questionnaires are available from the corresponding author. The EMPHASIS study group is open to data sharing with other bona fide researchers; applicants should e-mail the corresponding author, attaching a completed form, which can be found on the study website, and a decision will be made by the study’s data sharing committee. Data will be made available in the public domain after publication of the main results (expected 2018–2019) subject to official permission, according to national regulations in India and The Gambia.
Author information
Authors and Affiliations
Consortia
Contributions
The study was conceived and designed by GRC, CHDF, AMP and MJS. LA, MA, MB, CC, GRC, HC, MKD, GRG, MG, PI, LMAJ, PJ, RJ, KK, LK, SHK, KAL, MN, SSN, SO, AP, RDP, TDSP, AST, HS, SAS, SS, SS, KAW, DKY and CSY contributed significantly to data acquisition. Data analysis will be performed by GRC, CDG, PI, KAL, SSN, TDSP, AS, AST, MJS, SS, SS and DKY. All authors contributed to critical review of this manuscript for intellectual content, and have approved the submitted version. All Authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
MMNP (ISRCTN62811278) was approved by the ethics committees of BYL Nair and TN Medical College, Grant Medical College, and Sir JJ Group of Hospitals, Mumbai. PMMST (ISRCTN13687662) was approved by the joint Gambia Government / MRC Unit The Gambia’s Ethics Committee. Ethics approval for the follow-up of the children in Mumbai (‘SARAS KIDS’) was obtained from the Intersystem Biomedica Ethics Committee, Mumbai on 31st May 2013 (Serial no. ISBEC/NR-54/KM/JVJ/2013). Ethics approval for the EMPHASIS study in the Gambia, was obtained from the joint Gambia Government/MRC Unit The Gambia’s Ethics Committee on 19th October 2015 (Serial no. SCC 1441). The EMPHASIS study is registered as ISRCTN14266771. Signed informed consent was obtained from parents, and verbal assent from the children.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chandak, G.R., Silver, M.J., Saffari, A. et al. Protocol for the EMPHASIS study; epigenetic mechanisms linking maternal pre-conceptional nutrition and children’s health in India and Sub-Saharan Africa. BMC Nutr 3, 81 (2017). https://doi.org/10.1186/s40795-017-0200-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40795-017-0200-0