Abstract
Background
Treating rectal cancer presents challenges due to postoperative complications and reduced quality of life (QOL). Recent evidence supports the watch-and-wait (WW) approach for patients with a clinical complete response (cCR) following preoperative treatment. In this report, we discuss a case of metastatic rectal cancer with deficient mismatch repair (dMMR) treated successfully with pembrolizumab.
Case presentation
A 47-year-old male with dMMR rectal cancer and a single liver metastasis underwent treatment with pembrolizumab as neoadjuvant therapy. After 10 courses, the rectal lesion achieved cCR, prompting the selection of the WW approach. The liver metastasis showed significant shrinkage; however, the presence of a residual tumor was suspected, leading to a metastasectomy. A pathological complete response (pCR) was confirmed via histological examination. During a 24-month follow-up, there was no evidence of tumor regrowth, local recurrence, or distant metastasis.
Conclusions
The WW strategy is increasingly accepted for patients achieving cCR after preoperative treatment. While pCR in dMMR rectal cancer patients treated with immune checkpoint inhibitors (ICIs) has been documented, accurately predicting pCR from imaging remains challenging. This case illustrates that integrating ICI therapy, surgical interventions, and the WW approach can effectively achieve both oncological safety and improved QOL in the treatment of dMMR metastatic rectal cancer.
Similar content being viewed by others
Background
Deficient mismatch repair (dMMR), a genetic anomaly, occurs in approximately 15% of colorectal cancer (CRC) cases in Western populations, compared to only 3.8–7% in Japanese individuals [1,2,3,4]. The prevalence of dMMR in rectal cancer is relatively low, estimated between 4% and 6.9% [5, 6]. Notably, the frequency of dMMR decreases with advancing stages of CRC, dropping to about 5% in metastatic cases [7]. CRC with dMMR has shown resistance to cytotoxic chemotherapeutic agents compared with proficient mismatch repair (pMMR) [8]. However, both locally advanced and metastatic rectal cancers with dMMR respond favorably to immune checkpoint inhibitors (ICIs) [9,10,11].
Persistent concerns about postoperative complications and a decline in quality of life (QOL) associated with surgery for lower rectal cancer have been documented [12]. The watch-and-wait (WW) strategy, applied to patients who achieve a clinical complete response (cCR) after preoperative treatment, has gained traction due to increasing evidence of its effectiveness [13].
Despite the presumed rarity of dMMR in metastatic rectal cancer, the favorable outcomes observed with ICIs suggest potential benefits such as avoiding surgery and preserving anal function. However, definitive treatment protocols have not been established due to insufficient evidence. Here, we present a case of metastatic rectal cancer treated with ICIs where primary rectal lesions that showed cCR were managed using the WW approach. Although multiple imaging modalities suggested a residual tumor, surgical resection of the metastatic liver lesion confirmed a pathologic complete response (pCR).
Case presentation
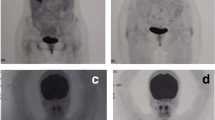
A 47-year-old male presented with bloody stools and was referred to our hospital. Colonoscopy revealed tumor in the lower rectum near the dentate line, which was pathologically diagnosed as moderately differentiated adenocarcinoma (Fig. 1a). Magnetic resonance imaging (MRI) staged the rectal tumor as T2, with no evidence of extramural vascular invasion (EMVI) or circumferential resection margin (CRM) involvement (Fig. 1b). Contrast-enhanced computed tomography (CECT) and gadoxetic acid (Gd-EOB-DTPA)-enhanced MRI identified a solitary 50 mm metastatic lesion in the caudate lobe of the liver (Fig. 1c, d). There was no obvious lymph node metastasis identified. Carcinoembryonic antigen (CEA) and carbohydrate antigen 19-9 (CA19-9) levels were 23.1 ng/mL and 29.6 U/mL, respectively. Immunohistochemical mismatch repair analysis showed loss of MSH6 with retained MLH1, MSH2, and PMS2 in the tumor. MSH6 sequencing identified c.3261del (p.Phe1088Serfs*2), leading to a diagnosis of Lynch syndrome, and genetic counseling was provided. Additionally, multiplex PCR confirmed MSI-high status. The KRAS gene had a G13D mutation, and BRAF was wild-type. The liver metastasis was classified as borderline resectable based on the institution’s criteria, which include having four or more liver metastases, any metastasis larger than 5 cm, or the presence of concomitant resectable extrahepatic metastases [14]. During the multidisciplinary team (MDT) conference, pembrolizumab was recommended as neoadjuvant therapy according to the MMR status. Figure 2 illustrates the timelines of treatments and assessments. After initiating treatment with pembrolizumab at a fixed dose of 200 mg administered intravenously every 3 weeks, an assessment after three courses showed shrinkage in both the liver and the primary lesion (non-CR), prompting consideration of surgical resection. However, considering the patient's preference for preserving anal function, the treatment continued. After a total of 10 courses of pembrolizumab, a cCR was achieved in the primary lesion (confirmed by digital rectal examination, MRI, and endoscopy), and the liver metastasis significantly reduced to 11 mm, without any immune-related adverse events (Fig. 3a–d). Tumor markers decreased to normal ranges, with CEA at 1.3 ng/mL and CA19-9 at 2.1 U/mL. The MDT recommended the WW approach for the rectal tumor and surgical intervention for the liver metastasis based on imaging that suggested the liver metastases were resectable. Additionally, their proximity to the inferior vena cava (IVC) was considered because of the risk that the tumors could become unresectable if they grew further. The rectal tumor was assessed as having achieved a cCR. The high likelihood of successful salvage surgery in the event of regrowth, coupled with the goal of preserving anal function, justified the decision for a WW approach. Subsequently, we performed a laparoscopic caudate resection with partial IVC resection for the liver metastasis, and the pathological examination confirmed a pCR. There was no evidence of rectal regrowth, recurrence, or metastasis of the primary tumor during the 24-month follow-up period without any treatment.
Imaging findings of primary and metastatic lesions before ICI therapy. a Inverted view of the endoscopic image at the rectum, showing a slightly elevated tumor located in the lower rectum. b Axial MRI sections of the rectal tumor, with arrowheads indicating a T2, EMVI-, CRM- rectal tumor. c CECT and d EOB-MRI of the liver, where the dashed line marks a 50 mm-sized solitary liver metastasis in the caudate
Timeline of treatment and evaluation. Day 0 marks the first course of pembrolizumab. i.v.: intravenous administration; MDT conference: multidisciplinary team conference; cCR: clinically complete response. *Assessment was conducted using multiple modalities, including endoscopy, CT, MRI, and digital rectal examination. **Tumor size was evaluated using gadoxetic acid (Gd-EOB-DTPA)-enhanced MRI
Imaging findings after ICI therapy. a The standard view of the endoscopic image at the lower rectum shows a flat scar without irregularities. b Axial MRI sections of the rectal area, with an arrowhead indicating the scar in the lower rectum with no evidence of residual tumor. c CECT and d EOB-MRI of the liver, with arrows pointing to a significantly shrunken liver metastasis
Discussion
Surgical treatment remains a cornerstone of therapeutic strategies for lower rectal cancer; however, preserving anal or defecatory function poses challenges, potentially leading to a significant decrease in postoperative QOL. Balancing oncological thoroughness with quality of life remains a continual dilemma. Increasing evidence supports the utility of the WW approach for patients with advanced lower rectal cancer who have achieved a cCR after neoadjuvant chemoradiotherapy [15, 16]. Additionally, Garcia-Aguilar et al. reported that total neoadjuvant therapy (TNT) could potentially obviate the need for surgery in approximately half of the patients with locally advanced lower rectal cancer, specifically in those with pMMR [17]. Meanwhile, in patients with dMMR CRC, 60–79% who underwent primary tumor resection after preoperative ICI treatment achieved a pCR, and 50% of those who underwent metastasectomy achieved a pCR in metastatic lesions[18,19,20]. In this case, we opted for the WW approach for the primary rectal lesion after achieving a cCR. For the liver metastasis, where imaging indicated a residual tumor, we chose surgical intervention, which resulted in a pCR. While recent reports on the WW strategy for locally advanced rectal cancer after treatment with ICIs raise expectations of its effectiveness, there are no reported experiences of combining surgery and WW for metastatic rectal cancer [9, 21].
Evaluating the CR to ICIs using radiographic assessments is complex. Further, differentiating between tumor cells, infiltrating immune cells, mucin, and necrotic tissue complicates the evaluation [11]. Additionally, unique phenomena such as pseudo-progression have been reported, where the tumor appears to enlarge following treatment; however, this enlargement often indicates an effective response to therapy [22]. It should be noted that in this case, if the pCR of the liver lesion had been predicted before surgery, the WW approach might have been a viable option for liver metastasis as well. Compared to rectal lesions, which can be comprehensively assessed using methods such as endoscopy, CT, MRI, and digital rectal examination, the evaluation of metastatic lesions is limited to fewer modalities, such as CT, MRI, and ultrasound. This highlights the limitations in accurately determining CR for metastatic lesions. Developing methods that can accurately predict pCR is highly desirable. Several biomarkers, including circulating tumor DNA (ctDNA), have been suggested to better reflect the true response compared to radiographic evaluations [23]. However, their clinical application has not yet been widely adopted, and resection is inevitable when a residual tumor is clearly evident on imaging. Nonetheless, as demonstrated in this case, the impact on postoperative QOL after partial hepatectomy is often not as severe as that after lower rectal surgery.
The WW approach following ICI treatment involves significant uncertainties regarding oncological safety, the establishment of optimal follow-up protocols, and therapeutic choices for tumor regrowth. Therefore, caution is crucial in making these decisions, and it is essential to provide patients with a thorough explanation and obtain their informed consent. Nevertheless, given the characteristics of ICIs mentioned above, we believe that our chosen strategy of surgical intervention for liver metastases with residual tumors, coupled with a WW approach for primary sites where cCR is achieved, is a viable option in the treatment strategy for metastatic rectal cancer.
In this case, a loss of MSH6 with MSI-high status was observed in the tumor tissue, and germline mutation testing confirmed Lynch syndrome. MSH6 accounts for approximately 10% of Lynch syndrome cases, which is less frequent than MLH1 or MSH2 [24]. CRC with loss of MSH6 has been reported to exhibit different characteristics compared to loss of MLH1 or MSH2. While dMMR CRCs are more common on the right side of the colon, loss of MSH6 is more frequent on the left side [25]. In particular, 25% of tumors associated with MSH6 develop in the rectum, compared to 5% for MLH1 or MSH2 tumors [26]. It has also been reported that loss of MSH6 is expected to display lower instability, and MSS status with loss of MSH6 is the most common discordance [27, 28]. In MSH6 mutation carriers, the risk for CRC was lower than in those with MLH1 or MSH2 mutations [29]. There is limited data on the effectiveness of ICIs for the loss of MSH6, although this case showed a remarkable effect, the response to ICI treatment for MSH6 may be lower than for other mutations considering the lower instability. It has been reported the efficacy of ICIs varies depending on different MMR alterations, and there are cases where ICIs were ineffective in MSS CRC with MSH6 loss [30, 31]. Further accumulation of data is warranted to clarify these observations.
Conclusions
This case demonstrates the potential for achieving both oncological safety and QOL by effectively integrating ICI therapy, surgical intervention, and the WW approach in the treatment of metastatic dMMR rectal cancer.
Availability of data and materials
Not applicable.
Abbreviations
- dMMR:
-
Deficient mismatch repair
- CRC:
-
Colorectal cancer
- pMMR:
-
Proficient mismatch repair
- ICIs:
-
Immune checkpoint inhibitors
- QOL:
-
Quality of life
- WW:
-
Watch-and-wait
- cCR:
-
Clinical complete response
- pCR:
-
Pathological complete response
- MRI:
-
Magnetic resonance imaging
- EMVI:
-
Extramural vascular invasion
- CRM:
-
Circumferential resection margin
- CECT:
-
Contrast-enhanced computed tomography
- CEA:
-
Carcinoembryonic antigen
- CA19-9:
-
Carbohydrate antigen 19-9
- MDT:
-
Multidisciplinary team
- IVC:
-
Inferior vena cava
References
Funkhouser WK, Lubin IM, Monzon FA, Zehnbauer BA, Evans JP, Ogino S, et al. Relevance, pathogenesis, and testing algorithm for mismatch repair-defective colorectal carcinomas. J Mol Diagnostics. 2012;14(2):91–103.
Rajagopalan H, Bardelli A, Lengauer C, Kinzler KW, Vogelstein B, Velculescu VE. RAF/RAS oncogenes and mismatch-repair status. Nature. 2002;418(6901):934–934.
Ishikubo T, Nishimura Y, Yamaguchi K, Khansuwan U, Arai Y, Kobayashi T, et al. The clinical features of rectal cancers with high-frequency microsatellite instability (MSI-H) in Japanese males. Cancer Lett. 2004;216(1):55–62.
Akagi K, Oki E, Taniguchi H, Nakatani K, Aoki D, Kuwata T, et al. Real-world data on microsatellite instability status in various unresectable or metastatic solid tumors. Cancer Sci. 2021;112(3):1105–13.
Pretta A, Donisi C, Persano M, Pinna G, Cimbro E, Parrino A, et al. Mismatch repair proteins (MMR) expression as predictive factor in locally advanced rectal cancer. J Clin Oncol. 2022;40(4):182–182. https://doi.org/10.1200/JCO.2022.40.4_suppl.182.
Ni K, Zhan Y, Liu Z, Yuan Z, Wang S, Zhao XZ, et al. Survival outcomes in locally advanced dMMR rectal cancer: surgery plus adjunctive treatment vs surgery alone. BMC Cancer. 2023;23(1):1–11. https://doi.org/10.1186/s12885-023-11525-7.
Venderbosch S, Nagtegaal ID, Maughan TS, Smith CG, Cheadle JP, Fisher D, et al. Mismatch repair status and BRAF mutation status in metastatic colorectal cancer patients: a pooled analysis of the CAIRO, CAIRO2, COIN, and FOCUS studies. Clin Cancer Res. 2014;20(20):5322–30.
Sargent DJ, Marsoni S, Monges G, Thibodeau SN, Labianca R, Hamilton SR, et al. Defective mismatch repair as a predictive marker for lack of efficacy of fluorouracil-based adjuvant therapy in colon cancer. J Clin Oncol. 2010;28(20):3219–26.
Cercek A, Lumish M, Sinopoli J, Weiss J, Shia J, Lamendola-Essel M, et al. PD-1 blockade in mismatch repair-deficient, locally advanced rectal cancer. N Engl J Med. 2022;386(25):2363–76.
Krekeler C, Wethmar K, Mikesch JH, Kerkhoff A, Menck K, Lenz G, et al. Complete metabolic response to combined immune checkpoint inhibition after progression of metastatic colorectal cancer on pembrolizumab: a case report. Int J Mol Sci. 2023;24(15):1–12.
Ludford K, Cohen R, Svrcek M, Foo WC, Colle R, Parc Y, et al. Pathological tumor response following immune checkpoint blockade for deficient mismatch repair advanced colorectal cancer. J Natl Cancer Inst. 2021;113(2):208–11.
van Heinsbergen M, den Haan N, Maaskant-Braat AJ, Melenhorst J, Belgers EH, Leijtens JW, et al. Functional bowel complaints and quality of life after surgery for colon cancer: prevalence and predictive factors. Color Dis. 2020;22(2):136–45.
Smith JJ, Strombom P, Chow OS, Roxburgh CS, Lynn P, Eaton A, et al. Assessment of a watch-and-wait strategy for rectal cancer in patients with a complete response after neoadjuvant therapy. JAMA Oncol. 2019;5(4): e185896.
Ichida H, Mise Y, Ito H, Ishizawa T, Inoue Y, Takahashi Y, et al. Optimal indication criteria for neoadjuvant chemotherapy in patients with resectable colorectal liver metastases. World J Surg Oncol. 2019;17(1):100. https://doi.org/10.1186/s12957-019-1641-5.
Dossa F, Chesney TR, Acuna SA, Baxter NN. A watch-and-wait approach for locally advanced rectal cancer after a clinical complete response following neoadjuvant chemoradiation: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2017;2(7):501–13.
Renehan AG, Malcomson L, Emsley R, Gollins S, Maw A, Myint AS, et al. Watch-and-wait approach versus surgical resection after chemoradiotherapy for patients with rectal cancer (the OnCoRe project): a propensity-score matched cohort analysis. Lancet Oncol. 2016;17(2):174–83.
Garcia-Aguilar J, Patil S, Gollub MJ, Kim JK, Yuval JB, Thompson HM, et al. Organ preservation in patients with rectal adenocarcinoma treated with total neoadjuvant therapy. J Clin Oncol. 2022;40(23):2546–56. https://doi.org/10.1200/JCO.22.00032.
Chalabi M, Fanchi LF, Dijkstra KK, Van den Berg JG, Aalbers AG, Sikorska K, et al. Neoadjuvant immunotherapy leads to pathological responses in MMR-proficient and MMR-deficient early-stage colon cancers. Nat Med. 2020;26(4):566–76.
Ludford K, Ho WJ, Thomas JV, Raghav KPS, Murphy MB, Fleming ND, et al. Neoadjuvant pembrolizumab in localized microsatellite instability high/deficient mismatch repair solid tumors. J Clin Oncol. 2023;41(12):2181–90. https://doi.org/10.1200/JCO.22.01351.
Marolleau P, Tougeron D, Allignet B, Cohen R, Sefrioui D, Gallet B, et al. Complete pathological response after chemotherapy or immune checkpoint inhibitors in deficient MMR metastatic colorectal cancer: results of a retrospective multicenter study. Int J Cancer. 2023;153(7):1376–85.
Zhang J, Cai J, Deng Y, Wang H. Complete response in patients with locally advanced rectal cancer after neoadjuvant treatment with nivolumab. Oncoimmunology. 2019;8(12): e1663108. https://doi.org/10.1080/2162402X.2019.1663108.
Xie Y, Lin J, Zhang N, Wang X, Wang P, Peng S, et al. Prevalent pseudoprogression and pseudoresidue in patients with rectal cancer treated with neoadjuvant immune checkpoint inhibitors. J Natl Compr Cancer Netw. 2023;21(2):133-142.e3.
Cabel L, Proudhon C, Romano E, Girard N, Lantz O, Stern MH, et al. Clinical potential of circulating tumour DNA in patients receiving anticancer immunotherapy. Nat Rev Clin Oncol. 2018;15(10):639–50.
Lynch HT, de la Chapelle A. Hereditary colorectal cancer. N Engl J Med. 2003;348(10):919–32. https://doi.org/10.1056/NEJMra012242.
Terui H, Tachikawa T, Kakuta M, Nishimura Y, Yatsuoka T, Yamaguchi K, et al. Molecular and clinical characteristics of MSH6 germline variants detected in colorectal cancer patients. Oncol Rep. 2013;30(6):2909–16. https://doi.org/10.3892/or.2013.2781.
Klarskov L, Holck S, Bernstein I, Okkels H, Rambech E, Baldetorp B, et al. Challenges in the identification of MSH6-associated colorectal cancer. Am J Surg Pathol. 2011;35(9):1391–9.
Pagin A, Zerimech F, Leclerc J, Wacrenier A, Lejeune S, Descarpentries C, et al. Evaluation of a new panel of six mononucleotide repeat markers for the detection of DNA mismatch repair-deficient tumours. Br J Cancer. 2013;108(10):2079–87.
Verma L, Kane MF, Brassett C, Schmeits J, Evans DG, Kolodner RD, et al. Mononucleotide microsatellite instability and germline MSH6 mutation analysis in early onset colorectal cancer. J Med Genet. 1999;36(9):678–82.
Hendriks YMC, Wagner A, Morreau H, Menko F, Stormorken A, Quehenberger F, et al. Cancer risk in hereditary nonpolyposis colorectal cancer due to MSH6 mutations: impact on counseling and surveillance. Gastroenterology. 2004;127(1):17–25.
Xie T, Feng Q, Li Z, Lu M, Li J, Lizaso A, et al. Heterogeneous constitutional mismatch repair deficiency with MSH6 missense mutation clinically benefits from pembrolizumab and regorafenib combination therapy: a case report and literature review. Hered Cancer Clin Pract. 2021;19(1):7. https://doi.org/10.1186/s13053-021-00165-2.
Khushman MM, Toboni MD, Xiu J, Manne U, Farrell A, Lou E, et al. Differential responses to immune checkpoint inhibitors are governed by diverse mismatch repair gene alterations. Clin Cancer Res. 2024;30(9):1906–15.
Acknowledgements
We would like to thank Editage (www.editage.jp) for English language editing.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
YA wrote the manuscript and prepared all figures. YS supported writing the manuscript and edited it. IN administered the neoadjuvant treatment. AO performed the surgical procedures. YS conducted the pathological evaluation. CA conducted the endoscopic evaluation. All authors participated in the treatment of the patient. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study adhered to the ethical guidelines of the 1964 Declaration of Helsinki and was approved by our institutional review board (2018-GA-1109). Written informed consent was obtained from the patient.
Consent for publication
Written informed consent was obtained from the patient's relative to publish this case report.
Competing interests
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ando, Y., Sakurai, T., Ozaki, K. et al. Integrating surgical intervention and watch-and-wait approach in dMMR metastatic rectal cancer with pembrolizumab: a case report. surg case rep 10, 198 (2024). https://doi.org/10.1186/s40792-024-01994-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-024-01994-8