Abstract
Background and Scope of Review
Varying severities and frequencies of head trauma may result in dynamic acute and chronic pathophysiologic responses in the brain. Heightened attention to long-term effects of head trauma, particularly repetitive head trauma, has sparked recent efforts to identify neuroimaging biomarkers of underlying disease processes. Imaging modalities like structural magnetic resonance imaging (MRI) and positron emission tomography (PET) are the most clinically applicable given their use in neurodegenerative disease diagnosis and differentiation. In recent years, researchers have targeted repetitive head trauma cohorts in hopes of identifying in vivo biomarkers for underlying biologic changes that might ultimately improve diagnosis of chronic traumatic encephalopathy (CTE) in living persons. These populations most often include collision sport athletes (e.g., American football, boxing) and military veterans with repetitive low-level blast exposure. We provide a clinically-oriented review of neuroimaging data from repetitive head trauma cohorts based on structural MRI, FDG-PET, Aβ-PET, and tau-PET. We supplement the review with two patient reports of neuropathology-confirmed, clinically impaired adults with prior repetitive head trauma who underwent structural MRI, FDG-PET, Aβ-PET, and tau-PET in addition to comprehensive clinical examinations before death.
Review Conclusions
Group-level comparisons to controls without known head trauma have revealed inconsistent regional volume differences, with possible propensity for medial temporal, limbic, and subcortical (thalamus, corpus callosum) structures. Greater frequency and severity (i.e., length) of cavum septum pellucidum (CSP) is observed in repetitive head trauma cohorts compared to unexposed controls. It remains unclear whether CSP predicts a particular neurodegenerative process, but CSP presence should increase suspicion that clinical impairment is at least partly attributable to the individual’s head trauma exposure (regardless of underlying disease). PET imaging similarly has not revealed a prototypical metabolic or molecular pattern associated with repetitive head trauma or predictive of CTE based on the most widely studied radiotracers. Given the range of clinical syndromes and neurodegenerative pathologies observed in a subset of adults with prior repetitive head trauma, structural MRI and PET imaging may still be useful for differential diagnosis (e.g., assessing suspected Alzheimer’s disease).
Similar content being viewed by others
Introduction
Lifetime head trauma exposure is a risk factor for multiple neurodegenerative diseases including Alzheimer’s disease (AD), Parkinson disease, amyotrophic lateral sclerosis, and chronic traumatic encephalopathy (CTE) [1,2,3,4,5,6,7,8]. CTE is the only neurodegenerative disease occurring almost exclusively in individuals with prior repetitive head trauma exposure, which is often sustained in the context of collision sports and/or military service. Conversely, most individuals with non-CTE neurodegenerative diseases have no documented head trauma exposure history, especially repetitive. Neuroimaging plays a key role in informing differential diagnoses of suspected neurodegenerative diseases, but researchers thus far have had little success identifying diagnostic imaging biomarkers that are specific for CTE in living adults.
Several advanced neuroimaging techniques have helped rapidly advance our understanding of disease pathophysiology, though only a handful are utilized clinically. Structural magnetic resonance imaging (MRI) is routinely performed in clinical settings to rule out non-neurodegenerative causes of clinical impairment like mass lesions and stroke, but also provides topographic representation of atrophy patterns. In some neurodegenerative conditions, atrophy patterns are sensitive and specific enough that they improve diagnostic certainty of syndromes like Alzheimer’s-type dementias [9,10,11], primary progressive aphasia subtypes [12], and behavioral variant frontotemporal dementia [13]. However, frank volume loss observable on structural MRI is thought to represent the culmination of a complex process of protein misfolding and deposition, neuronal and glial dysfunction, and ultimately synaptic and neuronal loss. Structural MRI interpretation also can be complicated by image processing limitations. Brain structure visualization and volume quantification via MRI occurs indirectly through measurement of underlying physical–chemical properties of brain tissue. There is inherent risk of overattributing group differences to true structural changes when other potential confounds like tissue perfusion or water content variability also significantly influence the measurement outcomes [14].
Other imaging techniques like positron emission tomography (PET) provide opportunities for detecting evidence of disease pathophysiology upstream of degeneration and potentially prior to symptom onset in individuals at risk for neurodegenerative disease. PET imaging is employed clinically to quantify metabolic brain changes or the burden and distribution of Aβ plaques and tau tangles using radiolabeled tracers. Uptake of fluorodeoxyglucose (FDG) is a marker of synaptic activity and brain metabolism. There is limited research applying FDG-PET in cases of repetitive head trauma or suspected CTE. Radiotracers have also been developed for binding Aβ plaques and tau tangles. Aβ tracers most often used in clinical practice include Florbetapir, Florbetaben, and Flutemetamol. Regarding tau PET, early small studies of repetitive head trauma cases used the FDDNP tracer, which has significant limitations, including nonselective binding to multiple insoluble protein aggregates (e.g., Aβ, tau, prion protein and others), low signal-to-noise ratio, and poor reproducibility across centers. Flortaucipir, the most studied tau PET tracer, was developed to bind paired helical filaments of tau that form neurofibrillary tangles (NFTs) in AD. AD research has rapidly facilitated development and clinical translation of Aβ and tau PET radiotracers. Together, these PET tracers can essentially confirm presence of AD plaque and tangle pathology in living patients. As we later discuss, initial excitement over the potential utility of tau PET tracers for identifying CTE tau pathology has significantly tempered in recent years. Other PET tracers detecting important disease processes like neuroinflammation (e.g., translocator protein, or TSPO-PET) [15] or synapse loss currently have relatively little data in repetitive head trauma populations.
The suspected higher prevalence of CTE in clinically impaired adults with repetitive head trauma exposure has motivated efforts targeting this population. Traumatic encephalopathy syndrome (TES) refers to the clinical manifestations of cognitive and/or neurobehavioral changes in individuals with repetitive head trauma exposure [16, 17]. Research criteria for TES were revised in 2021 [17] and require “substantial” exposure to repetitive head impacts from collision sports, military service, or other causes to qualify for diagnosis. There must be a predominant cognitive (episodic memory and/or executive functioning) and/or neurobehavioral syndrome (explosiveness, impulsivity, rage, etc.). Symptoms must be progressive and not fully accounted for by another neurologic, psychiatric, or medical condition, though suspicion of comorbid conditions (e.g., another neurodegenerative disease) is not exclusionary. A provisional level of certainty is assigned based on degree of head impact exposure and specific symptom manifestations - “Suggestive of CTE,” “Possible CTE,” or “Probable CTE”. Fluid and neuroimaging biomarkers do not factor into these research diagnostic criteria for TES due to lack of available data demonstrating specific associations with CTE pathology. “TES with definite CTE” can only be diagnosed by autopsy.
TES criteria were designed initially to maximize sensitivity over specificity to underlying CTE pathology. Earlier criteria [16] included several core and supportive symptoms also observed in relatively high frequency among adults without repetitive head trauma exposure or neurodegenerative disease (e.g., depression, anxiety, headaches) [18, 19]. Changes on structural neuroimaging (e.g., cavum septum pellucidum) or PET imaging of Aβ plaques and tau tangles previously were proposed to inform the likelihood that CTE is the cause of TES. However, neuroimaging correlates of repetitive head trauma, with or without presumed CTE, remain incompletely characterized. In particular, recent studies suggest that the proposed use of currently available tau PET tracers for increasing diagnostic certainty of CTE is premature.
The large number of review articles focused on neuroimaging of repetitive head trauma reflects the scientific interest in establishing neuroimaging biomarkers of CTE or other neurodegenerative effects of repetitive head trauma [20,21,22,23,24,25,26,27,28,29]. There are two key concepts that must be emphasized when reviewing and interpreting this literature: 1) clearly understanding the definition, frequency, severity, and timing of the head trauma exposure in any given study, and 2) resisting the temptation to assume that significant neuroimaging findings within repetitive head trauma cohorts reflect biomarkers specific to CTE. Despite CTE being highly associated with repetitive head trauma exposure [30, 31], CTE is only one possible neurodegenerative outcome of repetitive head trauma and often exists with other pathologies, such as Aβ plaques, alpha-synuclein, TDP-43 proteinopathies, and white matter rarefaction [5, 32]. In other words, the association of CTE with prior repetitive head trauma is much stronger than the association of repetitive head trauma with underlying CTE.
Scope of the Review and Relevant Terminology
Here we provide an overview of structural MRI and PET neuroimaging data from repetitive head trauma populations, with a focus on literature published within approximately the past 5 years. We chose to highlight structural MRI and PET given their direct clinical applications. Data from advanced neuroimaging modalities like diffusion tensor imaging (DTI), functional MRI, cerebral perfusion, and other modalities advance our understanding of repetitive head trauma pathophysiology. However, these modalities currently have minimal clinical footprint and largely are not validated for informing differential diagnosis.
“Head trauma” represents a complicated clinical spectrum that spans asymptomatic to symptomatic trauma. Table 1 describes classifications of commonly used terms in head trauma research as applied in this review. We focused our overview on repetitive head trauma populations, which we defined by individuals exposed, at a minimum, to repetitive, asymptomatic head impacts (i.e., “subconcussive” trauma without observable or reported acute symptoms). Typically, these populations are current or former collision sport athletes exposed to up to tens of thousands of asymptomatic head blows throughout a playing career, or military servicemembers subjected to repeated blast exposures. These groups inherently are at high risk of sustaining multiple symptomatic events, often mild TBI or concussion, in addition to repetitive asymptomatic blows. Other research has focused on acute and chronic neuroimaging outcomes in groups defined by discrete, symptomatic TBI events. Occasionally, such studies incorporate “repeat TBI” groups defined by having more than one symptomatic TBI. Such populations differ from those highlighted in our review based on the absence of repetitive, asymptomatic trauma, which currently is believed to be more strongly associated with TES and CTE.
In most cases, the repetitive head trauma studies referenced throughout include individuals who fulfill the minimum exposure criterion proposed in the TES research diagnosis [17]. We reserve the use of “TES” for populations defined by clinical symptomatology in the context of prior repetitive head trauma exposure, without presumption of known underlying CTE pathology. “CTE” will be used when referring to neuropathologic changes found in the brain at autopsy per consensus diagnosis recommendations [33], without presumption of a specific clinical manifestation.
General Challenges and Limitations of Current Research
Validating neuroimaging modalities as CTE biomarkers currently has significant challenges. Existing diagnostic criteria aimed at identifying living adults with underlying CTE are likely to capture many “false positive” patients given the criteria’s emphasis on sensitivity over specificity. Repetitive head trauma exposure places individuals at higher risk of CTE, but most will not develop CTE, so research cohorts defined by exposure alone may not have a high rate of CTE. Autopsy is currently the only gold standard for developing CTE biomarkers, and CTE cases with antemortem clinical and neuroimaging data are exceedingly rare [34,35,36,37]. There is also little research that has directly compared patients with and without prior head trauma with the cognitive and neurobehavioral features of the proposed TES criteria, which may help clarify syndrome profiles with greater specificity to head trauma-related neurodegenerative disease, like CTE.
Variability in acquisition of head trauma exposure data also complicates interpretation of current literature. Most neuroimaging studies of repetitive head trauma cohorts draw comparisons to either clinically normal or impaired controls considered free of lifetime head trauma exposure. Head trauma researchers frequently raise concerns about inaccurate characterization of exposure, though discussions usually focus on improving accuracy of exposure estimates in the head trauma cohorts themselves. Arguably, this issue is just as relevant for identifying appropriate control groups. Screening questionnaires inquiring about prior brain injury can be markedly insensitive and rarely query for lifetime participation in high-risk activities like collision sports [38]. Many questionnaires also require LOC or PTA for an event to qualify as a brain injury. There is therefore a high likelihood that many “control” groups used in these studies include some individuals with exposure to milder head trauma (e.g., concussion without LOC or PTA) or repetitive asymptomatic impacts, especially if drawn from existing study cohorts that were not recruited explicitly to serve as unexposed controls in comparison to a repetitive head trauma group. Inclusion of comparison groups with participants that have prior head trauma exposure may reduce the likelihood of identifying significant differences in various neuroimaging outcomes. However, matching controls on non-head trauma variables also presents challenges because high risk groups like elite athletes may disproportionately include individuals with sociodemographic, personality factors (e.g., risk-taking behaviors), and cognitive strengths (e.g., visuospatial or processing speed abilities) that are not representative of the general population.
Structural MRI
Brain Volume Differences Associated with Repetitive Head Trauma
Head trauma can result in diffuse axonal injury (DAI) resulting from the shear-strain forces imparted on white matter tracts [39]. Severe forms of TBI can result in DAI, focal contusions, or hemorrhages observable on conventional clinical MRI or CT. Prevailing theories suggest that repetitive asymptomatic head trauma, concussion, and mTBIs result in damage to cortical and subcortical microstructures despite observable findings on conventional MRI being rare [40]. Several studies of white matter integrity using DTI support this assertion. Among long white matter tracts in the brain, the genu and body of the corpus callosum most consistently show evidence of microstructural changes associated with head trauma [26, 41]. Presumably, accumulated exposure to repetitive head trauma would therefore ultimately lead to brain tissue loss and measurable differences in brain volume compared to otherwise healthy individuals without repetitive head trauma. Multiple studies have compared groups across the adult lifespan with and without repetitive head trauma. Collision sport athletes are the most studied population.
Professional Collision Sport Athletes
Former professional American football players and boxers represent the extreme of repetitive head trauma exposure and are a highly selected subgroup of collision sport athletes. As such, study samples are often small. Findings suggest that symptomatic (i.e., with cognitive and/or behavior and mood changes) former professional American football athletes may have lower amygdala [42], hippocampus [42,43,44], cingulate gyrus [42], fronto-insular [43], and anterior temporal [43, 45] brain volumes than age-matched healthy controls without head trauma. A study of active and recently retired professional rugby players similarly found lower bilateral hippocampal and left amygdala volumes than controls; differences were attributed partially to alcohol use [46]. Hippocampal volume differences in particular may result from steeper age-related atrophy in those with repetitive head trauma [47]. Subcortically, lower thalamic volumes have been associated with earlier age of initiating American football participation among retired professionals [48]. The Professional Fighters Brain Health Study investigated 476 active and former professional fighters (boxers and mixed martial artists; 92% active fighters and otherwise healthy) compared to 63 unexposed controls and found lower thalamus and corpus callosum volumes among fighters [49].
Conversely, some studies of former professional American football and hockey athletes without objective cognitive impairment showed no brain volume differences compared to controls [50]. Soccer participation has also raised concerns for brain health because of exposure to headers and high concussion risk [2], and one small study of former professional male soccer players noted areas of lower cortical thickness in inferior parietal, temporal, and occipital cortices [51]. Data from multi-site studies targeting former professional collision sport athletes, like DETECT (Diagnosing and Evaluating Traumatic Encephalopathy using Clinical Tests) and DIAGNOSE CTE (Diagnostics, Imaging, and Genetics Network for the Objective Study and Evaluation of Chronic Traumatic Encephalopathy), are expected to advance development of clinically applicable neuroimaging biomarkers.
Non-Professional Collision Sport Athletes (High School, Collegiate)
Collegiate and high school collision sport athletes better represent general athlete population exposure levels to repetitive head trauma. Typically, these individuals have less overall lifetime head trauma exposure than professionals given the earlier “retirement” from their sport. The Concussion Assessment, Research, and Education (CARE) Consortium is a national multi-site study of sport-related head trauma (concussion and repetitive asymptomatic exposure) [52] that has produced several recent reports on structural brain changes in active collegiate athletes [53,54,55]. Brett and colleagues found that active, healthy collision sport athletes showed an association of more years of sport participation—a proxy for cumulative head trauma exposure—with lower thalamic volumes [56]. This effect was not observed in non-contact sport athletes. In a separate smaller study of active collegiate American football players, cortical thickness was lower than controls in several frontal lobe regions, but only in American football players who also had a history of symptomatic concussion [57]. This suggests a potential moderating or synergistic effect of symptomatic events with repetitive asymptomatic trauma on brain volume development or tissue loss. A longitudinal investigation of collegiate American football players found several regions of lower volume compared to non-contact athletes (volleyball) at baseline [58]. However, the American football athletes paradoxically exhibited less grey matter volume loss and cortical thinning over up to 4 years of follow-up than the non-contact athletes. This was interpreted as a potential pathologic disruption to normal neurodevelopmental and myelination dynamics seen in adolescence and early adulthood [59].
Most American football participants do not play past high school. Data indicate that older adults with prior high school level exposure are indistinguishable on brain health metrics from older adults without prior head trauma exposure [60,61,62]. Former high school football players reporting multiple symptomatic concussions did not have significantly different brain volumes than former high school players without prior concussion, but no pure control group without head trauma exposure was included [63]. While our focus in this review is on structural MRI, multiple studies of active high school and collegiate American football athletes have reported evidence for altered white matter microstructure and functional connectivity associated with repetitive head impacts even in the absence of symptomatic injuries [26, 41, 64,65,66,67,68,69]. The chronicity of these changes, relation to volume loss, and relevance for later-life brain health remain unclear.
Military Service and Repetitive Blast Exposure
Few studies have directly evaluated brain volume changes associated with repetitive blast exposure in military servicemembers, which contrasts the frequent study of acute and chronic outcomes of discrete TBI events [70,71,72]. Breachers are a unique subpopulation of military servicemembers (and of law enforcement) frequently exposed to repeated, low-intensity blasts during training and active duty. One small study of 20 breachers reporting between 100 and 35,000 estimated career blast exposures found greater cortical thickness in occipital lobe and default mode network regions (medial frontal, medial temporal, inferior parietal, precuneus, posterior cingulate cortices) compared to unexposed controls [73]. Authors speculated that this finding may reflect alterations in cortical myelination, intracortical connections, or glial scarring at the gray-white matter junction that image processing pipelines miscalculate when distinguishing between tissue types [73]. Baseline (i.e., pre-exposure) group structural differences, as well as other factors that influence volumetric measurements also cannot be ruled out. Another small study of 10 military veterans reporting frequent low-level blast exposures found no volumetric differences from unexposed controls, but noted areas of nonspecific white matter hyperintensity signal in 5 of the 10 blast-exposed veterans [74].
Cavum Septum Pellucidum: A “Canary in the Coal Mine” for Repetitive Head Trauma-Related Neurodegenerative Disease
Cavum septum pellucidum (CSP) refers to separation of the septum pellucidum usually best observed on coronal view of conventional T1 MRI as hypointense (CSF filled) space between the two septal leaflets (Fig. 1). CSP was first detectable using air encephalography in the 1930s. Forster (1933) recognized CSP in a patient who suffered a brain injury and later died, at which point CSP was confirmed at autopsy. A smattering of additional cases was reported in subsequent decades before Spillane’s case series of “Five Boxers” in 1962 [75], wherein he observed septum pellucidum damage in three of the five boxers. One year later, Mawdsley & Ferguson reported CSP in 7 of 10 ex-boxers with chronic neurologic impairment [76]. The authors contended that “Changes in septum pellucidum probably cause no neurological deficit. Radiologic demonstration of a cavum, by implicating boxing as its probable cause, is helpful diagnostically” [76]. Growing evidence over the following 60 years largely supports Mawdsley’s and Ferguson’s prescient conclusions.

adapted from Gardner et al. 2016, J Neurotrauma, 33(1):157–61 (permissions pending review and acceptance of manuscript)
Enlarged views of representative T1 coronal images for each “grade” of cavum septum pellucidum (CSP). A “Grade 0” septum pellucidum appears crisp without any evidence of cyst or separation (CSP absent). “Grade 1” CSP shows slight interior hypointensity that is not clearly CSF signal intensity (septum unclear/CSP equivocal). Grades 2–4 show clear evidence of CSF signal between separated leaves of the septum pellucidum. The degree of separation between the leaves is used to assign a grade of 2–4: Grade 2 CSP is not wider than the septum, Grade 3 CSP is wider than the septum but less than half the intraventricular width, and Grade 4 CSP is greater than half the intraventricular width. Grading is based on the coronal slice that shows the greatest evidence of separation of the leaves of the septum pellucidum. Figure and caption
CSP has been observed at a striking, but variable, rate within repetitive head trauma cohorts in recent years. Researchers have questioned the sensitivity and specificity of CSP to repetitive head trauma exposure, but the frequency with which this phenomenon occurs in such cases warrants attention. Two 2016 publications reported higher rates of CSP in clinically impaired, former professional American football players. The first study showed CSP was more frequent compared to cognitively impaired, matched case-controls without prior head trauma (16/17, 94% vs. 3/17, 18%) [77]. The second study found higher rates compared to healthy, former noncontact sport athletes (66/72, 92% vs. 8/14, 57%) [78]. In both studies, CSP length was also significantly longer in the symptomatic former American football groups. Within the large Professional Fighter Brain Health Study cohort, 53% of 499 active and former fighters had CSP compared to 17% of 62 unexposed controls. CSP length was again significantly greater in the former fighters [79]. The high frequency of CSP in repetitive head trauma cohorts, particularly those experiencing neurologic changes, has prompted proposals that CSP may be a neuroimaging biomarker for CTE in living patients [16]. Autopsy case series reporting up to 65% of CTE cases with CSP [80, 81] support such recommendations, but the predictive value of CSP for identifying CTE remains unclear. The current evidence linking CSP to repetitive head trauma outweighs the evidence linking CSP to underlying CTE pathology as currently defined [34]. A key gap in the repetitive head trauma-CSP literature is a large-scale evaluation of CSP in asymptomatic, clinically normal individuals with repetitive head trauma. This would inform relevance of CSP to clinical symptoms or potential prognostic risk for later development of neurodegenerative disease.
CSP has also been observed in other patient populations and in variable rates among otherwise healthy individuals. A meta-analysis of CSP prevalence in psychiatric populations found 1.4 × greater likelihood of CSP compared to psychiatrically healthy controls and almost 2 × greater likelihood of a large CSP (≥ 6 mm length), though there was significant heterogeneity across included studies [82]. Schizophrenia, in particular, is classically linked to higher rates of CSP but data suggest that this association may be limited to risk for larger CSP than presence per se [83]. Similar associations with CSP enlargement have been noted in adolescent-onset opiate dependence [84] and obsessive–compulsive disorder [85], though data are mixed [86]. It remains unclear whether CSP presence is congenital, develops over time, or is directly and meaningfully associated with clinical symptoms. Limited evidence from a small subset of serially imaged boxers suggests CSP develops and increases in size in the course of repetitive trauma exposure [87, 88]. It is also essential to consider that other populations with high rates of CSP, like those with psychiatric illness, are at significantly higher risk of lifetime head trauma exposure [89,90,91]. As discussed previously, studies not focused on head trauma may not assess participants for possible exposure or may rely on insensitive methods to rule out exposure. Anecdotally, CSP with fenestrations or a “ratty” appearance may imply a traumatic etiology as some have speculated rapid acceleration-deceleration or fluid percussion force causes shearing of the two septal leaflets.
Structural White Matter Abnormalities
White matter susceptibility to traumatic forces underscores the potential for findings on clinically relevant structural MRI sequences. Active collegiate hockey players were found to have a similar number of white matter hyperintensity (WMH) counts to controls on T2/fluid attenuated inversion recovery (FLAIR) imaging [92]. However, WMH lesions in the athlete group were located more closely to the grey-white matter junction and to sulcal depths, regions associated with early CTE pathology in affected brains. There was also a slight predominance for the frontal lobes (75% of all lesions) relative to controls (56%). Lesion counts did not change over the course of a single hockey season and did not increase acutely after concussion. In a small study of collegiate American football players, a subset of athletes exhibited general decreased susceptibility weighted imaging (SWI) signal after one season of participation, which was interpreted as potential evidence for asymptomatic, trauma-related microbleeds [64]. Alosco et al. reported higher frequency of white matter signal abnormalities on high-resolution T1 in former professional American football athletes than controls, the number of which correlated with the estimated amount of head trauma exposure throughout their playing career [93]. To date, there is less research using clinically available MRI sequences to characterize white matter abnormalities in repetitive head trauma cohorts than exists for acute brain injury patients.
It is unclear whether these structural white matter findings reflect neurodegenerative changes, especially in younger, asymptomatic participants. However, several studies document cerebrovascular pathophysiology associated with repetitive head trauma, including altered cerebral perfusion dynamics [64, 94,95,96,97] and blood–brain-barrier dysfunction [98, 99], which may produce white matter signal abnormalities on MRI. In CTE cases, more severe white matter rarefaction is associated with greater exposure to repetitive head trauma, severity of neurofibrillary tangle deposition, and likelihood of developing dementia [32].
Take-Home Points on Structural MRI in Repetitive Head Trauma
No characteristic atrophy pattern has emerged as specific to repetitive head trauma exposure. There are somewhat consistent findings of lower medial temporal and subcortical (thalamus, corpus callosum) volumes in repetitive head trauma cohorts compared to controls across the lifespan, though interpreting group level volume differences in younger, active athletes is complicated by neurodevelopmental dynamics. We cannot readily attribute volumetric differences to a specific neurodegenerative pathology (e.g., CTE) but susceptibility of these regions to traumatic forces implicates repetitive head trauma regardless of the underlying pathophysiologic process. Collective evidence indicates that presence of CSP in clinically impaired adults with repetitive head trauma exposure should increase suspicion that the presence of any neurodegenerative disease, whether CTE or otherwise, is attributable at least in part to the patient’s repetitive head trauma. Emerging research suggests repetitive head trauma exposure may also lead to white matter alterations observable on clinically available structural MRI sequences (i.e., T2/FLAIR). White matter pathologies seen in CTE and their direct relevance for clinical impairment [80, 100,101,102] strongly implicate the importance of further studying neuroimaging modalities that characterize white matter changes in repetitive head trauma cohorts.
Positron Emission Tomography (PET) Metabolic and Molecular Neuroimaging
FDG-PET Neuroimaging of Repetitive Head Trauma
FDG-PET (2-deoxy-2-(18F)fluoro-deoxyglucose) provides in vivo evidence of the severity and spatial distribution of changes in brain metabolism presumed to represent altered synaptic activity. Few studies have used FDG-PET to evaluate participants with a history of repetitive head trauma. Two small studies of active and former boxers found lower FDG uptake (i.e., hypometabolism) in multiple but inconsistent regions including posterior cingulate [103], bilateral frontal lobes [104], parieto-occipital cortex [103], and the cerebellum [103]. Former American football players had significantly lower frontotemporal metabolism than controls [43]. In one study of military veterans, higher number of prior blast exposures correlated with lower cerebellar metabolism [105]. An antemortem PET-to-autopsy case report (CTE stage IV with hippocampal sclerosis) showed mild FDG hypometabolism corresponding with medial temporal and frontal atrophy. Medial temporal structures contained multiple degenerative protein aggregates, while frontal lobe pathology was predominantly CTE (see [106] and description of Patient #1 below).
Aβ-PET Neuroimaging of Repetitive Head Trauma
In 2012, Florbetapir became the first Aβ-PET tracer approved by the U.S. Food and Drug Administration (FDA) for detecting moderate to frequent neuritic Aβ plaques, a core neuropathological feature of AD. Two similar radiotracers received approval shortly thereafter (Flutemetamol, Florbetaben). Widespread clinical implementation of Aβ-PET imaging remains limited in the U.S. and other countries due to lack of insurance reimbursement. However, emerging data from the Imaging Dementia – Evidence for Amyloid Scanning (IDEAS) study strongly support the relevance of Aβ-PET imaging in clinical management of cognitively impaired older adults [107]. Clinical feasibility of more routine Aβ-PET scans therefore may increase significantly, especially if tied to effective Aβ lowering therapeutic agents.
Most studies of repetitive head trauma do not specifically analyze associations with cortical Aβ burden. Instead, Aβ-PET often is used to rule out or identify comorbid AD. A negative Aβ-PET scan previously was proposed as a “positive biomarker” supporting a “Probable CTE” diagnosis [16] because Aβ plaques are not a diagnostic feature of CTE and their absence strongly suggests AD is not driving symptoms [34]. Among 11 living patients with “Probable CTE,” 2 were Aβ-PET positive and also showed the most severe atrophy plus tau PET signal [43]. In brains with CTE at autopsy, Aβ deposition is a common co-pathology (> 90% of former professional American football players with advanced CTE) [5], occurs at an accelerated rate, and preferentially affects the depths of cortical sulci [108]. Aβ plaques in CTE usually are diffuse rather than neuritic, which may explain lower affinity of Aβ-PET tracers.
Acute brain injury has been linked to upregulation of amyloid precursor protein, which is cleaved to form Aβ polypeptides [109,110,111,112]. Studies evaluating Aβ-PET acutely after TBI inconsistently note presence of cortical Aβ plaques [25]. One autoradiography study reported white matter accumulation of Aβ and amyloid precursor protein, but no binding of Aβ-radiotracer (Pittsburgh Compound B; PIB), which aligned with their finding of no differences in white matter PIB binding between TBI patients and controls [113]. Across two studies of moderate-severe TBI patients compared to controls, one showed greater cortical grey matter and striatum binding (< 1 yr post-TBI) [113] and one showed greater posterior cingulate and cerebellum binding (> 1 yr post-TBI) [114]. Conversely, a recent investigation of remote head trauma exposure (both mild TBI and a subset with repetitive asymptomatic exposure) found no association with later-life cortical Aβ burden using PET in clinically normal older adults [115]. Others similarly have reported a lack of association between remote, mild head trauma exposure and cortical Aβ burden [116,117,118].
Tau-PET Neuroimaging of Repetitive Head Trauma
FDDNP
Most early tau-PET studies in repetitive head trauma patients used the FDDNP radiotracer. FDDNP binding properties severely limit its sensitivity and specificity to CTE pathology. FDDNP binds to different protein aggregates that form beta-pleated sheets (Aβ plaques, tau tangles, prion proteins, and others), has poor reproducibility, and has a low signal-to-noise ratio [119,120,121,122]. Regardless, several early studies found group-level differences between repetitive head trauma participants and controls in the spatial pattern and degree of FDDNP tracer uptake [123, 124]. Data indicated that groups of blast-exposed veterans and former professional American football players, albeit often with small numbers, showed FDDNP binding in white matter and subcortical structures [123] along with limbic and brain stem regions [123, 125]. Binding patterns seemingly differed from AD cases as well. One case study reported a former American football player diagnosed with CTE at autopsy (also with frequent neuritic Aβ plaques) who underwent FDDNP-PET imaging about 4 years before death. The report showed that FDDNP binding levels correlated with the amount of tau deposition in the brain at autopsy [126]. However, the FDDNP radiotracer is not FDA approved and there is no support for clinical utility.
Flortaucipir (FTP)
FTP was developed to detect paired helical filament tau in neurofibrillary tangles characteristic of AD (now FDA approved). Multiple investigations consistently support FTP use for differentiation of AD from controls and non-AD tauopathies [127,128,129], but there is limited comparison to CTE. There were high hopes that the science of CTE and repetitive head trauma biomarker development could ride the wave of extremely promising research demonstrating strong affinity of the FTP tracer to AD tau [127]. Excitement over potential CTE diagnosis stemmed from known similarities in phosphorylated tau isoforms between AD and CTE – mixed 3-repeat/4-repeat tau tangles with paired helical filament structures. However, an autoradiography study showed that FTP only weakly bound to brain tissue with dense CTE pathology compared to its strong binding to tissue with AD tau [130], again suggesting limited potential for sensitive or specific CTE detection. Newly identified differences in fibril folding microstructure between CTE and AD tau may explain differences in tau radiotracer binding affinity [131].
FTP exhibits “off-target” (i.e., non-tau related) binding to choroid plexus (often complicating medial temporal signal interpretation) [132, 133], caudate, putamen, pallidum, thalamus, and white matter [133,134,135], and cortically in some cases of tau-negative neurodegenerative disease [127]. An early case report speculating that FTP binding in the basal ganglia reflected a “novel variant” of CTE likely represented off-target tracer binding [133, 134, 136]. More recently, Stern et al. reported a group-level comparison of 26 predominantly Aβ-PET negative former professional American football athletes to 31 controls and found higher FTP binding in medial temporal, parietal, and superior frontal lobes [137]. Degree of FTP uptake correlated with number of years participating in American football, but there was no association with cognitive outcomes [138]. Lesman-Segev et al. compared 11 clinically impaired TES patients to clinically impaired, biomarker-confirmed AD patients and unexposed, Aβ-PET negative, clinically normal controls [43]. There was mildly elevated FTP binding in frontotemporal regions of TES patients relative to unexposed controls, and no regions with higher FTP signal than the AD group. Some patients exhibited FTP binding in a non-contiguous “dot-like” pattern, similar to data reported in a small group of veterans with history of multiple low-level blast exposures [74]. This pattern is also observed in some healthy controls [43] and may simply represent noise or imaging artifact [43, 127].
A recent case report compared antemortem FTP binding in a former professional American football player to neuropathology observed at autopsy [106]. The patient had severe CTE (stage IV) and hippocampal sclerosis without comorbid AD. FTP uptake overlapped well with CTE tau pathology in the inferior temporal lobe and juxtacortical frontal white matter, but there was weak FTP uptake on PET imaging in several areas of the brain with dense CTE tau deposition at autopsy and confirmed off-target binding subcortically.
The recent release of the FDA’s label for FTP provides essential context for application in clinical settings. FTP scans are indicated for estimating the density and distribution of aggregated tau neurofibrillary tangles in adults with cognitive impairment who are being evaluated for AD. “Positive” scans show visually apparent increased neocortical tracer uptake in the posterolateral temporal, occipital, or parietal/precuneus regions, with or without frontal uptake. FTP is not indicated for use in the evaluation of patients for CTE. This does not inherently rule out the potential clinical utility of FTP-PET scans for patients with a history of repetitive head trauma if their clinical profile raises suspicion for AD. In this scenario, a “positive” FTP scan would implicate underlying Alzheimer’s disease as contributing to cognitive impairment (especially if accompanied by elevated Aβ PET), but would not rule out comorbid CTE. A “negative” FTP scan might increase the likelihood that CTE is driving cognitive symptoms, contrary to prior research criteria proposing that positive tau PET findings fulfill the biomarker-based requirement for “Probable CTE” [16].
Other Tau PET Tracers and Considerations for Future Development
Several additional tau PET tracers exist, and others are rapidly being developed [139], but most thus far have rarely been used in repetitive head trauma research. PBB3 is a family of tau PET compounds that appears to bind tau aggregates consisting of all isoforms [140, 141]. Takahata and colleagues found that patients with TES showed higher [11C]-PBB3 binding in white matter than individuals with single-event TBI [142]. Binding to tau lesions at the depths of neocortical sulci (suggesting CTE pathology) was confirmed via in vitro assays [142]. The second-generation MK-6240 tracer is a highly selective paired helical filament tau tracer with less off-target binding in the brain, but with off-target meningeal binding [143, 144]. A recent case report of a former Australian rules football athlete described in vivo MK-6240 cortical uptake in a pattern resembling the spatial distribution of CTE (bilateral superior frontal and medial temporal regions) and distinct from a typical AD pattern [145]. However, limited autoradiographic evidence suggests MK-6240, like FTP, may have high affinity for AD tau tangles but not CTE tau [143]. Additional validation work is necessary. Other tau tracers include RO-948, PI-2620, and GTP-1. These tracers are derivatives of FTP and thus likely have similar binding characteristics, but this has not been tested empirically.
Temporal dynamics of the underlying disease process may also be particularly relevant for developing a diagnostic PET biomarker for CTE. For example, FTP binds neurofibrillary tangles and autopsy studies suggest that a “positive” scan requires advanced AD tau pathology (Braak stage V-VI). Early-stage CTE involves sparse neurofibrillary tangle deposition often located at brain/CSF interfaces where PET signal can be washed out by partial volume effects. It is therefore likely that a CTE-specific PET tracer will be sensitive only to relatively advanced pathology (i.e., CTE Stage III-IV). Further complicating matters in CTE, which is a mixed 3R/4R tauopathy, the 4R tau isoform may be much more prevalent than the 3R isoform earlier in the disease process before shifting towards deposition of 3R tau and fully formed neurofibrillary tangles [146]. Astrocytic tau inclusions are also a prominent feature of CTE despite being insufficient for formal diagnosis [34]. Recent work showed that the tau tangles within neurons are a mix of 3R and 4R isoforms while astrocytes predominantly contain 4R tau [146, 147].
Take-Home Points on FDG-PET, Aβ-PET, Tau-PET Neuroimaging
FDG-PET study findings implicate inconsistent brain regions, which is not surprising given the heterogeneous underlying diseases within clinically impaired repetitive head trauma cohorts. The main utility of Aβ-PET in repetitive head trauma research currently rests on ruling out concomitant AD pathology. Collective findings thus far unfortunately suggest limited utility of well-studied AD tau PET radiotracers for identifying CTE. A radiotracer sensitive and specific to CTE-tau must be developed and likely must account both for variations in relative presence of 3R versus 4R tau isoforms at different disease stages (e.g., mild or severe) and in different cell types (neurons versus astrocytes). Appreciation for off-target (i.e., non-tau) binding properties and nonspecific binding patterns (non-contiguous, “dot-like”) is critical to avoid potential false-positive diagnoses.
Clinico-Pathologic Examples of Clinically Suspected CTE Patients With and Without CTE Pathology at Autopsy
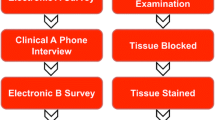
Here we present two research participants from the UCSF Memory and Aging Center’s Alzheimer’s Disease Research Center. Both patients were evaluated and discussed by multidisciplinary consensus conference after comprehensive neurological and neuropsychological evaluations. Each patient also underwent antemortem, multimodal neuroimaging obtained prior to death and autopsy. Both patients met 2014 TES criteria for “Probable CTE.” We also retroactively applied the recent 2021 TES diagnostic framework, which resulted in one patient clinically diagnosed with “Probable CTE” and one patient diagnosed with “Possible CTE.” Neuroimaging modalities included structural MRI, FDG-PET, Aβ-PET (PIB), and tau-PET (FTP). We provide summaries of neuroimaging and neuropathologic findings to demonstrate potential limitations of existing neuroimaging techniques for identifying CTE pathology. Figure 2 and the Additional file 1: supplementary figure show slices from antemortem neuroimaging.
Representative slices of antemortem structural T1 magnetic resonance imaging (T1 MRI), FDG-PET, Aβ-PET (PIB), and tau-PET (FTP) for 2 clinically impaired adults with prior repetitive head trauma meeting criteria for “Probable CTE” (see text for case descriptions). Patient #1 had a primary neuropathologic diagnosis of CTE (Stage IV) with contributing hippocampal sclerosis and left subiculum microinfarct (no AD pathology observed). Patient #2 had a primary neuropathologic diagnosis of FTLD-tau (corticobasal degeneration) with contributing hippocampal sclerosis and unclassifiable FTLD-TDP-43 inclusions (no CTE or AD pathology observed). For FDG-PET, cooler colors represent areas of decreased glucose uptake (hypometabolism). For PIB-PET, warmer colors represent increased tracer uptake. A positive Aβ-PET scan is represented by increased tracer uptake diffusely throughout the cortex. In both patients, Aβ tracer uptake is restricted to the white matter, which is considered non-specific and represents a negative Aβ-PET scan. For FTP-PET, warmer colors represent areas of increased tracer binding. A “positive” scan for AD neurofibrillary tangles requires contiguous neocortical uptake in the posterolateral temporal, occipital, or parietal/precuneus regions with or without frontal uptake. Neither patient showed a typical AD pattern of FTP tracer uptake, while both showed evidence of nonspecific, scattered frontotemporal uptake and non-specific increased signal in the basal ganglia. Slices were chosen to highlight cavum septum pellucidum (T1 MRI) or representative areas of hypometabolism (FDG-PET) and Aβ/tau tracer uptake. Additional brain slices for PET scans from each case are provided in supplemental material
Patient #1
The first patient (described in detail elsewhere [106]) was a 72-year-old former professional American football player with a 17-year participation history that began at age 14. His primary playing position was linebacker. He reported a 13-year symptom progression with initial changes in behavior and mood (irritability, anger outbursts, social withdrawal, depression), memory, and executive function. He later developed parkinsonism and seizures. Consensus clinical diagnosis was TES-mixed variant. Applying the 2021 TES diagnostic framework, Patient #1 qualifies for “Probable CTE” based on presence of ≥ 11 years of American football exposure, delayed symptom onset, emergence of motor signs, ≥ 1 psychiatric feature, and neurobehavioral dysregulation.
Antemortem structural MRI (age 68) showed cavum septum pellucidum (Grade 2; 12 mm length). There was predominantly anterior and ventral atrophy including bilateral limbic and medial temporal regions and the left middle frontal lobe. PET scans were obtained at the same visit as structural MRI. FDG-PET showed mild hypometabolism in medial temporal and frontal lobes. Aβ-PET was negative. Tau-PET showed tracer uptake in a non-AD pattern including nonspecific scattered frontotemporal binding. The patient fulfilled 3 (only 1 required) of the biomarker-based criteria from the 2014 TES criteria for Probable CTE (CSP, negative Aβ-PET, cortical atrophy) and also had some evidence suggesting abnormal tau-PET.
The primary neuropathologic diagnosis was CTE (Stage IV). Immunohistochemical analysis showed frequent clusters of tau-immunoreactive neurons and astrocytes in perivascular spaces at depths of sulci located in cortical, subcortical, and spinal cord regions. The most affected cortical regions were frontal, temporal, and limbic structures. There was also focal hippocampal sclerosis (left; CA1) and a left subiculum microinfarct. Additional findings included limbic argyrophilic grain disease, limbic-predominant age-related TDP-43 encephalopathy (LATE; stage 2), aging-related tau astrogliopathy, and mild arteriolosclerosis. There was no evidence of Aβ pathology.
Patient #2
The second patient was a 49-year-old former collegiate American football player with an 8-year participation history that began at age 12. His primary playing position was quarterback. He was also a professional motorcyclist and racecar driver wherein he suffered at least 3 additional mild TBIs after his American football career. He reported an 8-year symptom progression initially presenting with apathy, loss of empathy, social disinhibition, and compulsive behaviors. He later developed memory loss and language difficulties. Consensus clinical diagnosis was behavioral variant frontotemporal dementia. He also fulfilled criteria for TES-behavioral/mood variant. Applying the 2021 TES diagnostic framework, Patient #2 qualifies for “Possible CTE” based on ≥ 5 but < 11 years of American football exposure, delayed symptom onset, ≥ 1 psychiatric features, and neurobehavioral dysregulation.
Antemortem structural MRI (age 47) showed cavum septum pellucidum (Grade 1; 5 mm length). There was prominent left frontoparietal and subcortical atrophy including bilateral thalamus and left caudate. PET scans were obtained at the same visit as structural MRI. FDG-PET showed severe medial frontal, thalamic, and basal ganglia hypometabolism also affecting parietal and temporal lobes. Aβ-PET was negative. Tau-PET showed tracer uptake in a non-AD pattern including moderate frontotemporal white matter and basal ganglia binding with left predominance. The patient fulfilled 3 of the biomarker-based criteria from the 2014 TES criteria for Probable CTE (CSP, negative Aβ-PET, cortical atrophy) and also had evidence suggesting abnormal tau-PET.
The primary neuropathologic diagnosis was FTLD-tau (corticobasal degeneration). Immunohistochemical analysis showed frequent neuronal cytoplasmic inclusions, tau-positive ballooned neurons, coiled bodies, and variably dense astrocytic plaques, as well as severe subcortical white matter tauopathy. There was also widespread TDP-43 pathology with diverse inclusion types usually, but not always, in a pattern resembling the tauopathy (particularly prominent in medial temporal limbic structures and accompanied by severe hippocampal sclerosis affecting all sectors of Ammon’s horn). There was no evidence of CTE or AD pathology.
Clinically Suspected CTE Patient Summary
Both patients exhibited clinical decline several years after repetitive head trauma exposure and had multiple biomarkers suggesting underlying CTE pathology per prior research criteria [16]. Atrophic areas on structural MRI and regional hypometabolism on FDG-PET were largely consistent with the presenting clinical syndromes. Of note, tau PET in each participant showed abnormal, low-level tracer uptake in a clearly non-AD pattern. In the absence of tau PET, which is not widely available clinically, presence of CSP and negative Aβ-PET alone would likely have made both patients strong candidates for harboring significant CTE pathology. It remains unknown if or how Patient #2’s head trauma exposure contributed to the onset, progression, or symptom manifestation of non-CTE neuropathologic processes. Beyond the limitations of available neuroimaging modalities for reliably identifying CTE, these cases highlight the diversity of prospectively documented symptom presentations and underlying neurodegenerative diseases among clinically impaired patients with repetitive head trauma exposure.
Future Considerations for Neuroimaging Research in Repetitive Head Trauma
Structural Neuroimaging
Structural MRI remains an important and relatively accessible component of clinical evaluations for patients with suspected neurodegenerative disease, but usually images are reviewed qualitatively. Incorporating quantitative MRI methods and/or advanced sequences like DTI into clinical practice may improve sensitivity to head trauma-related brain changes. Systematically collecting different types of lifetime head trauma exposure, from repetitive asymptomatic impacts to severe TBI, will facilitate our understanding of brain changes on structural MRI attributable to head trauma. While elite level collision sport athletes represent an important study group, extending these efforts to the broader aging population will enhance generalizability and improve risk estimation along a wider spectrum of head trauma exposure.
Other PET Radiotracers
While there is an understandable focus on in vivo CTE tau identification, measuring the degree and spatial distribution of neuroinflammation [100, 148,149,150] and synaptic dysfunction are other potentially interesting PET applications for repetitive head trauma [151,152,153]. The translocator protein (TSPO) is a mitochondrial membrane protein that is upregulated in activated microglia, astroglia, and macrophages. Several TSPO-PET ligands have been developed as in vivo markers of neuroinflammation. One study of TSPO-PET using the [11C]DPA-713 tracer found higher signal in former American professional football players than controls in bilateral medial and superior temporal regions [15]. New molecular targets for imaging activated microglia and astrocytes are currently under development [150]. To our knowledge, PET imaging of synaptic loss (e.g., synaptic vesicle glycoprotein 2A; SV2A-PET) [154, 155] has not been performed in repetitive head trauma cohorts. It is unclear if these approaches will be clinically meaningful in isolation for specific disease identification (e.g., differentiating CTE from AD or other neurodegenerative diseases), but they may prove valuable for unlocking pathophysiologic mechanisms linking repetitive head trauma to increased neurodegenerative disease risk in general.
Sex-Specific differences in Neuroimaging of Repetitive Head Trauma
Sex differences in neuroimaging findings among repetitive head trauma cohorts are unknown. Existing studies almost exclusively focus on male-predominant groups of collision sport athletes (e.g., American football) and military veterans. Reported sex differences in head impact biomechanics [156,157,158], brain injury outcomes [159,160,161], and risk for neurodegenerative disease [162, 163] underscore the critical importance of studying the role of sex in repetitive head trauma outcomes. Large-scale, longitudinal cohorts like the Professional Fighters Brain Health Study [164], CARE Consortium [52], Chronic Effects of Neurotrauma Consortium [165], and longitudinal follow-up of the Transforming Research and Clinical Knowledge in TBI cohort [166] (i.e., TRACK-TBI LONG) offer strong potential for studying sex-specific outcomes in the association of repetitive head trauma with brain volume changes or molecular/metabolic alterations on PET imaging. Former participants in presumably high-risk female collision sports like soccer/futbol, ice hockey, rugby, mixed martial arts, etc. may be especially important study cohorts. Additionally, intimate partner violence survivors, who are usually female, are an often overlooked but critically important group to study [167]. Comprehensive evaluation of both repetitive, asymptomatic exposure and symptomatic brain injuries will be essential to these efforts.
Concluding Remarks
Repetitive head trauma may increase risk for multiple neurodegenerative outcomes, with much recent focus on CTE. Structural MRI studies in repetitive head trauma cohorts do not clearly suggest a specific pattern of volume loss, though subcortical structures like the thalamus and corpus callosum and medial temporal limbic region appear susceptible to repetitive traumatic forces. Cavum septum pellucidum is much more common in clinically impaired repetitive head trauma populations than both clinically normal and impaired cohorts without head trauma exposure. Presence of cavum septum in clinically impaired adults with repetitive head trauma should increase suspicion that head trauma exposure contributed to the underlying disease. White matter abnormalities occasionally are observable on conventional clinical MRI and may be spatially distinct in repetitive head trauma populations, but more work characterizing these abnormalities is needed. FDG-PET studies have not identified a characteristic repetitive head trauma pattern, which likely reflects the diversity of underlying neuropathologies and associated clinical syndromes. Tau-PET remains a promising research avenue but will require development of CTE-tau specific radiotracers given the lack of support for current tracers with strong affinity for AD tau. PET imaging of Aβ plaques and AD tau tangles may still be clinically useful in ruling AD in or out. CTE is highly associated with prior repetitive head trauma. However, we caution against tenuous assumptions that CTE is present, or the sole or primary source of symptoms, in clinically impaired repetitive head trauma cohorts without other compelling clinical or biomarker data. Improving diagnostic precision for neurodegenerative disease within repetitive head trauma cohorts requires antemortem imaging-to-autopsy studies and development of other in vivo biomarkers sensitive to the effects of repetitive trauma on brain health.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- AD:
-
Alzheimer’s disease
- Aβ:
-
Beta-amyloid
- CARE:
-
Concussion Assessment, Research, and Education Consortium
- CSF:
-
Cerebrospinal fluid
- CSP:
-
Cavum septum pellucidum
- CT:
-
Computed tomography
- CTE:
-
Chronic traumatic encephalopathy
- DAI:
-
Diffuse axonal injury
- DETECT:
-
Diagnosing and Evaluating Traumatic Encephalopathy using Clinical Tests
- DIAGNOSE-CTE:
-
Diagnostics, Imaging, and Genetics Network for the Objective Study and Evaluation of Chronic Traumatic Encephalopathy
- DTI:
-
Diffusion tensor imaging
- FDA:
-
Food & Drug Administration
- FDDNP:
-
2-(1-{6-[(2-Fluoroethyl(methyl)amino]-2-naphthyl}ethylidene)malononitrile
- FDG:
-
Fluorodeoxyglucose
- FLAIR:
-
Fluid attenuated inversion recovery
- FTP:
-
Flortaucipir
- IDEAS:
-
Imaging Dementia – Evidence for Amyloid Scanning
- LOC:
-
Loss of consciousness
- MRI:
-
Magnetic resonance imaging
- mTBI:
-
Mild traumatic brain injury
- NFT:
-
Neurofibrillary tangle
- PET:
-
Positron emission tomography
- PIB:
-
Pittsburgh Compound B
- PTA:
-
Posttraumatic amnesia
- SV2A:
-
Synaptic vesicle glycoprotein 2A
- SWI:
-
Susceptibility weighted imaging
- TBI:
-
Traumatic brain injury
- TES:
-
Traumatic encephalopathy syndrome
- TRACK-TBI:
-
Transforming Research and Clinical Knowledge in TBI
- TSPO:
-
Translocator protein
- WMH:
-
White matter hyperintensity
References
Perry DC, Sturm VE, Peterson MJ, Pieper CF, Bullock T, Boeve BF et al (2016) Association of traumatic brain injury with subsequent neurological and psychiatric disease: a meta-analysis. J Neurosurg 124(2):511–526
Mackay DF, Russell ER, Stewart K, MacLean JA, Pell JP, Stewart W (2019) Neurodegenerative disease mortality among former professional soccer players. N Engl J Med 381:1801–1808
Gardner RC, Yaffe K (2015) Epidemiology of mild traumatic brain injury and neurodegenerative disease. Mol Cell Neurosci 66:75–80
Nordström A, Nordström P (2018) Traumatic brain injury and the risk of dementia diagnosis: a nationwide cohort study. PLoS Med 15(1):e1002496
Mez J, Daneshvar DH, Kiernan PT, Abdolmohammadi B, Alvarez VE, Huber BR et al (2017) Clinicopathological evaluation of chronic traumatic encephalopathy in players of American football. JAMA 318(4):360–370
Gardner RC, Byers AL, Barnes DE, Li Y, Boscardin J, Yaffe K (2018) Mild TBI and risk of parkinson disease: a chronic effects of neurotrauma consortium study. Neurology 90(20):e1771–e1779
Lehman EJ, Hein MJ, Baron SL, Gersic CM (2012) Neurodegenerative causes of death among retired national football league players. Neurology 79(19):1970–1974
Crane PK, Gibbons LE, Dams-O’Connor K, Trittschuh E, Leverenz JB, Keene CD et al (2016) Association of traumatic brain injury with late-life neurodegenerative conditions and neuropathologic findings. JAMA Neurol 73(9):1062–1069
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH et al (2011) The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dementia 7(3):263–269
Crutch SJ, Schott JM, Rabinovici GD, Murray M, Snowden JS, van der Flier WM et al (2017) Consensus classification of posterior cortical atrophy. Alzheimer’s Dementia 13(8):870–884
Ossenkoppele R, Pijnenburg YA, Perry DC, Cohn-Sheehy BI, Scheltens NM, Vogel JW et al (2015) The behavioural/dysexecutive variant of Alzheimer’s disease: clinical, neuroimaging and pathological features. Brain 138(Pt 9):2732–2749
Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF et al (2011) Classification of primary progressive aphasia and its variants. Neurology 76(11):1006–1014
Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J et al (2011) Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain 134(Pt 9):2456–2477
Weinberger DR, Radulescu E (2021) Structural Magnetic Resonance Imaging All Over Again. JAMA Psychiat 78(1):11–12
Coughlin JM, Wang Y, Minn I, Bienko N, Ambinder EB, Xu X et al (2017) Imaging of glial cell activation and white matter integrity in brains of active and recently retired national football league players. JAMA Neurol 74(1):67–74
Montenigro PH, Baugh CM, Daneshvar DH, Mez J, Budson AE, Au R et al (2014) Clinical subtypes of chronic traumatic encephalopathy: literature review and proposed research diagnostic criteria for traumatic encephalopathy syndrome. Alzheimer’s Res Therapy 6(5):68
Katz DI, Bernick C, Dodick DW, Mez J, Mariani ML, Adler CH, et al (2021) National Institute of neurological disorders and stroke consensus diagnostic criteria for traumatic encephalopathy syndrome, Neurology (Epub Ahead of Print; PMID:33722990)
Iverson GL, Gardner AJ (2020) Risk for misdiagnosing chronic traumatic encephalopathy in men with anger control problems. Front Neurol 11:739
Iverson GL, Gardner AJ (2020) Risk of misdiagnosing chronic traumatic encephalopathy in men with depression. J Neuropsychiatry Clin Neurosci 32(2):139–146
Koerte IK, Lin AP, Willems A, Muehlmann M, Hufschmidt J, Coleman MJ et al (2015) A review of neuroimaging findings in repetitive brain trauma. Brain Pathol 25(3):318–349
Ng TS, Lin AP, Koerte IK, Pasternak O, Liao H, Merugumala S et al (2014) Neuroimaging in repetitive brain trauma. Alzheimers Res Ther 6(1):10
Sundman MH, Hall EE, Chen NK (2014) Examining the relationship between head trauma and neurodegenerative disease: a review of epidemiology, pathology and neuroimaging techniques. J Alzheimer's Dis Parkin 4:137
Shetty T, Raince A, Manning E, Tsiouris AJ (2016) Imaging in chronic traumatic encephalopathy and traumatic brain injury. Sports Health 8(1):26–36
Lee BG, Leavitt MJ, Bernick CB, Leger GC, Rabinovici G, Banks SJ (2018) A Systematic review of positron emission tomography of tau, amyloid beta, and neuroinflammation in chronic traumatic encephalopathy: the evidence to date. J Neurotrauma 35(17):2015–2024
Ayubcha C, Revheim ME, Newberg A, Moghbel M, Rojulpote C, Werner TJ et al (2021) A critical review of radiotracers in the positron emission tomography imaging of traumatic brain injury: FDG, tau, and amyloid imaging in mild traumatic brain injury and chronic traumatic encephalopathy. Eur J Nucl Med Mol Imaging 48(2):623–641
Asken BM, DeKosky ST, Clugston JR, Jaffee MS, Bauer RM (2018) Diffusion tensor imaging (DTI) findings in adult civilian, military, and sport-related mild traumatic brain injury (mTBI): a systematic critical review. Brain Imaging Behav 12(2):585–612
Sparks P, Lawrence T, Hinze S (2020) Neuroimaging in the diagnosis of chronic traumatic encephalopathy: a systematic review. Clin J Sport Med 30(Suppl 1):S1-s10
Dallmeier JD, Meysami S, Merrill DA, Raji CA (2019) Emerging advances of in vivo detection of chronic traumatic encephalopathy and traumatic brain injury. Br J Radiol 92(1101):20180925
Lin A, Charney M, Shenton ME, Koerte IK (2018) Chronic traumatic encephalopathy: neuroimaging biomarkers. Handb Clin Neurol 158:309–322
Asken BM, Sullan MJ, DeKosky ST, Jaffee MS, Bauer RM (2017) Research gaps and controversies in chronic traumatic encephalopathy: a review. JAMA Neurol 74(10):1255–1262
Bieniek KF, Ross OA, Cormier KA, Walton RL, Soto-Ortolaza A, Johnston AE et al (2015) Chronic traumatic encephalopathy pathology in a neurodegenerative disorders brain bank. Acta Neuropathol 130(6):877–889
Alosco ML, Stein TD, Tripodis Y, Chua AS, Kowall NW, Huber BR et al (2019) Association of white matter rarefaction, arteriolosclerosis, and tau with dementia in chronic traumatic encephalopathy. JAMA Neurol 76(11):1298–1308
Bieniek KF, Cairns NJ, Crary JF, Dickson DW, Folkerth RD, Keene CD et al (2021) The second NINDS/NIBIB consensus meeting to define neuropathological criteria for the diagnosis of chronic traumatic encephalopathy. J Neuropathol Exp Neurol 80(3):210–219
McKee AC, Cairns NJ, Dickson DW, Folkerth RD, Keene CD, Litvan I et al (2016) The first NINDS/NIBIB consensus meeting to define neuropathological criteria for the diagnosis of chronic traumatic encephalopathy. Acta Neuropathol 131(1):75–86
Smith DH, Johnson VE, Trojanowski JQ, Stewart W (2019) Chronic traumatic encephalopathy—confusion and controversies. Nature Rev Neurol 15(3):179–183
Iverson GL, Gardner AJ, Shultz SR, Solomon GS, McCrory P, Zafonte R et al (2019) Chronic traumatic encephalopathy neuropathology might not be inexorably progressive or unique to repetitive neurotrauma. Brain 142(12):3672–3693
Iverson GL, Luoto TM, Karhunen PJ, Castellani RJ (2019) Mild chronic traumatic encephalopathy neuropathology in people with no known participation in contact sports or history of repetitive neurotrauma. J Neuropathol Exp Neurol 78(7):615–625
Gardner RC, Rivera E, O’Grady M, Doherty C, Yaffe K, Corrigan J et al (2020) Screening for lifetime history of traumatic brain injury among older American and Irish adults at risk for dementia: development and validation of a web-based survey. J Alzheimer's Dis 74(2):699–711
Su E, Bell M (2016) Diffuse axonal injury. In: Laskowitz D, Grant G (eds) Translational research in traumatic brain injury. CRC Press/Taylor and Francis Group © (2016) by Taylor & Francis Group. LLC, Boca Raton, FL, pp 41–84
Klein AP, Tetzlaff JE, Bonis JM, Nelson LD, Mayer A, Huber DL et al (2019) Prevalence of potentially clinically significant MRI findings in athletes with and without sport-related concussion. J Neurotrauma 36(11):1776–1785
Champagne AA, Peponoulas E, Terem I, Ross A, Tayebi M, Chen Y et al (2019) Novel strain analysis informs about injury susceptibility of the corpus callosum to repeated impacts. Brain Commun 1(1):fcz021
Lepage C, Muehlmann M, Tripodis Y, Hufschmidt J, Stamm J, Green K et al (2019) Limbic system structure volumes and associated neurocognitive functioning in former NFL players. Brain Imaging Behav 13(3):725–734
Lesman-Segev OH, La Joie R, Stephens ML, Sonni I, Tsai R, Bourakova V et al (2019) Tau PET and multimodal brain imaging in patients at risk for chronic traumatic encephalopathy. NeuroImage: Clin 24:102025
Strain JF, Womack KB, Didehbani N, Spence JS, Conover H, Hart J et al (2015) Imaging correlates of memory and concussion history in retired National Football League athletes. JAMA Neurol 72(7):773–780
Goswami R, Dufort P, Tartaglia MC, Green RE, Crawley A, Tator CH et al (2016) Frontotemporal correlates of impulsivity and machine learning in retired professional athletes with a history of multiple concussions. Brain Struct Funct 221(4):1911–1925
Wojtowicz M, Gardner AJ, Stanwell P, Zafonte R, Dickerson BC, Iverson GL (2018) Cortical thickness and subcortical brain volumes in professional rugby league players. NeuroImage Clin 18:377–381
Misquitta K, Dadar M, Tarazi A, Hussain MW, Alatwi MK, Ebraheem A et al (2018) The relationship between brain atrophy and cognitive-behavioural symptoms in retired Canadian football players with multiple concussions. NeuroImage Clin 19:551–558
Schultz V, Stern RA, Tripodis Y, Stamm J, Wrobel P, Lepage C et al (2018) Age at first exposure to repetitive head impacts is associated with smaller thalamic volumes in former professional american football players. J Neurotrauma 35(2):278–285
Lee JK, Wu J, Bullen J, Banks S, Bernick C, Modic MT et al (2020) Association of cavum septum pellucidum and cavum vergae with cognition mood, and brain volumes in professional fighters. JAMA Neurol 77(1):35–42
Zivadinov R, Polak P, Schweser F, Bergsland N, Hagemeier J, Dwyer MG et al (2018) Multimodal imaging of retired professional contact sport athletes does not provide evidence of structural and functional brain damage. J Head Trauma Rehabil 33(5):E24-e32
Koerte IK, Mayinger M, Muehlmann M, Kaufmann D, Lin AP, Steffinger D et al (2016) Cortical thinning in former professional soccer players. Brain Imaging Behav 10(3):792–798
Broglio SP, McCrea M, McAllister T, Harezlak J, Katz B, Hack D et al (2017) A national study on the effects of concussion in collegiate athletes and US military service academy members: the NCAA-DoD concussion assessment, research and education (CARE) consortium structure and methods. Sports Med 47(7):1437–1451
Wu YC, Harezlak J, Elsaid NMH, Lin Z, Wen Q, Mustafi SM et al (2020) Longitudinal white-matter abnormalities in sports-related concussion: A diffusion MRI study. Neurology 95(7):e781–e792
Mustafi SM, Harezlak J, Koch KM, Nencka AS, Meier TB, West JD et al (2018) Acute white-matter abnormalities in sports-related concussion: a diffusion tensor imaging study from the NCAA-DoD CARE consortium. J Neurotrauma 35(22):2653–2664
Klein AP, Tetzlaff JE, Bonis JM, Nelson LD, Mayer AR, Huber DL et al (2019) Prevalence of potentially clinically significant magnetic resonance imaging findings in athletes with and without sport-related concussion. J Neurotrauma 36(11):1776–1785
Brett BL, Bobholz SA, España LY, Huber DL, Mayer AR, Harezlak J et al (2020) Cumulative effects of prior concussion and primary sport participation on brain morphometry in collegiate athletes: a study from the NCAA-DoD CARE Consortium. Front Neurol 11:673
Meier TB, Bellgowan PS, Bergamino M, Ling JM, Mayer AR (2016) Thinner cortex in collegiate football players with, but not without, a self-reported history of concussion. J Neurotrauma 33(4):330–338
Mills BD, Goubran M, Parivash SN, Dennis EL, Rezaii P, Akers C et al (2020) Longitudinal alteration of cortical thickness and volume in high-impact sports. Neuroimage 217:116864
Wierenga LM, Langen M, Oranje B, Durston S (2014) Unique developmental trajectories of cortical thickness and surface area. Neuroimage 87:120–126
Janssen PH, Mandrekar J, Mielke MM, Ahlskog JE, Boeve BF, Josephs K et al (2017) High school football and late-life risk of neurodegenerative syndromes, 1956–1970. Mayo Clin Proc 92(1):66–71
Savica R, Parisi JE, Wold LE, Josephs KA, Ahlskog JE (2012) High school football and risk of neurodegeneration: a community-based study. Mayo Clin Proc 87(4):335–340
Deshpande SK, Hasegawa RB, Rabinowitz AR, Whyte J, Roan CL, Tabatabaei A et al (2017) Association of playing high school football with cognition and mental health later in life. JAMA Neurol 74(8):909–918
Terry DP, Miller LS (2018) Repeated mild traumatic brain injuries is not associated with volumetric differences in former high school football players. Brain Imaging Behav 12(3):631–639
Slobounov SM, Walter A, Breiter HC, Zhu DC, Bai X, Bream T et al (2017) The effect of repetitive subconcussive collisions on brain integrity in collegiate football players over a single football season: a multi-modal neuroimaging study. NeuroImage Clin 14:708–718
Mayinger MC, Merchant-Borna K, Hufschmidt J, Muehlmann M, Weir IR, Rauchmann BS et al (2018) White matter alterations in college football players: a longitudinal diffusion tensor imaging study. Brain Imaging Behav 12(1):44–53
Gong NJ, Kuzminski S, Clark M, Fraser M, Sundman M, Guskiewicz K et al (2018) Microstructural alterations of cortical and deep gray matter over a season of high school football revealed by diffusion kurtosis imaging. Neurobiol Dis 119:79–87
Murugesan G, Saghafi B, Davenport E, Wagner B, Urban J, Kelley M et al (2018) Single season changes in resting state network power and the connectivity between regions: distinguish head impact exposure level in high school and youth football players. Proc SPIE Int Soc Opt Eng 10575:105750F
Abbas K, Shenk TE, Poole VN, Breedlove EL, Leverenz LJ, Nauman EA et al (2015) Alteration of default mode network in high school football athletes due to repetitive subconcussive mild traumatic brain injury: a resting-state functional magnetic resonance imaging study. Brain Connect 5(2):91–101
Hirad AA, Bazarian JJ, Merchant-Borna K, Garcea FE, Heilbronner S, Paul D et al (2019) A common neural signature of brain injury in concussion and subconcussion. Sci Adv 5(8):eaau3460
Davenport ND, Gullickson JT, Grey SF, Hirsch S, Sponheim SR (2018) Longitudinal evaluation of ventricular volume changes associated with mild traumatic brain injury in military service members. Brain Inj 32(10):1245–1255
Bigler ED, Abildskov TJ, Eggleston B, Taylor BA, Tate DF, Petrie JA et al (2019) Structural neuroimaging in mild traumatic brain injury: a chronic effects of neurotrauma consortium study. Int J Methods Psychiat Res 28(3):1781
Martindale SL, Rostami R, Shura RD, Taber KH, Rowland JA (2020) Brain volume in veterans: relationship to posttraumatic stress disorder and mild traumatic brain injury. J Head Trauma Rehabil 35(4):E330-e341
Stone JR, Avants BB, Tustison NJ, Wassermann EM, Gill J, Polejaeva E et al (2020) Functional and structural neuroimaging correlates of repetitive low-level blast exposure in career breachers. J Neurotrauma 37(23):2468–2481
Dickstein DL, De Gasperi R, Gama Sosa MA, Perez-Garcia G, Short JA, Sosa H, et al (2020) Brain and blood biomarkers of tauopathy and neuronal injury in humans and rats with neurobehavioral syndromes following blast exposure. Mol Psychiatry (Online ahead of print; PMCID: PMC7484380)
Spillane JD (1962) Five boxers. BMJ 2(5314):1205–1210
Mawdsley C, Ferguson FR (1963) Neurological disease in boxers. Lancet (London, England) 2(7312):795–801
Gardner RC, Hess CP, Brus-Ramer M, Possin KL, Cohn-Sheehy BI, Kramer JH et al (2016) Cavum septum pellucidum in retired american pro-football players. J Neurotrauma 33(1):157–161
Koerte IK, Hufschmidt J, Muehlmann M, Tripodis Y, Stamm JM, Pasternak O et al (2016) Cavum septi pellucidi in symptomatic former professional football players. J Neurotrauma 33(4):346–353
Lee JK, Wu J, Banks S, Bernick C, Massand MG, Modic MT et al (2017) Prevalence of traumatic findings on routine MRI in a large cohort of professional fighters. AJNR Am J Neuroradiol 38(7):1303–1310
McKee AC, Stein TD, Nowinski CJ, Stern RA, Daneshvar DH, Alvarez VE et al (2013) The spectrum of disease in chronic traumatic encephalopathy. Brain 136(1):43–64
Smith DH, Johnson VE, Stewart W (2013) Chronic neuropathologies of single and repetitive TBI: substrates of dementia? Nat Rev Neurol 9(4):211–221
Wang LX, Li P, He H, Guo F, Tian P, Li C et al (2020) The prevalence of cavum septum pellucidum in mental disorders revealed by MRI: a meta-analysis. J Neuropsychiatry Clin Neurosci 32(2):175–184
Trzesniak C, Oliveira IR, Kempton MJ, Galvão-de Almeida A, Chagas MH, Ferrari MC et al (2011) Are cavum septum pellucidum abnormalities more common in schizophrenia spectrum disorders? A systematic review and meta-analysis. Schizophrenia Res 125(1):1–12
Hwang J, Kim JE, Kaufman MJ, Renshaw PF, Yoon S, Yurgelun-Todd DA, et al (2013) Enlarged cavum septum pellucidum as a neurodevelopmental marker in adolescent-onset opiate dependence. PLoS One 8(10):e78590.
Chon MW, Choi JS, Kang DH, Jung MH, Kwon JS (2010) MRI study of the cavum septum pellucidum in obsessive-compulsive disorder. Eur Arch Psychiatry Clin Neurosci 260(4):337–343
Kim KJ, Peterson BS (2003) Cavum septi pellucidi in Tourette syndrome. Biol Psychiat 54(1):76–85
Jordan BD, Jahre C, Hauser WA, Zimmerman RD, Zarrelli M, Lipsitz EC et al (1992) CT of 338 active professional boxers. Radiology 185(2):509–512
Zimmerman RD, Jordan BD (1992) Neuroradiology of boxing injuries. In: Jordan BD (ed) Medical aspects of boxing. CRC Press, Inc., Boca Raton, FL, pp 188–195
Greer N, Sayer NA, Spoont M, Taylor BC, Ackland PE, MacDonald R et al (2020) Prevalence and severity of psychiatric disorders and suicidal behavior in service members and veterans with and without traumatic brain injury: systematic review. J Head Trauma Rehabil 35(1):1–13
Phipps H, Mondello S, Wilson A, Dittmer T, Rohde NN, Schroeder PJ et al (2020) Characteristics and impact of U.S. military blast-related mild traumatic brain injury: a systematic review. Front Neurol 11:559318
Molloy C, Conroy RM, Cotter DR, Cannon M (2011) Is traumatic brain injury a risk factor for schizophrenia? A meta-analysis of case-controlled population-based studies. Schizophrenia Bull 37(6):1104–1110
Jarrett M, Tam R, Hernández-Torres E, Martin N, Perera W, Zhao Y et al (2016) A prospective pilot investigation of brain volume, white matter hyperintensities, and hemorrhagic lesions after mild traumatic brain injury. , Front Neurol 7:11
Alosco ML, Koerte IK, Tripodis Y, Mariani M, Chua AS, Jarnagin J et al (2018) White matter signal abnormalities in former National Football League players. Alzheimer’s Dementia 10:56–65
Amen DG, Willeumier K, Omalu B, Newberg A, Raghavendra C, Raji CA (2016) Perfusion neuroimaging abnormalities alone distinguish national football league players from a healthy population. J Alzheimer’s Diseas 53(1):237–241
Roby PR, Duquette P, Kerr ZY, Register-Mihalik J, Stoner L, Mihalik JP (2021) Repetitive head impact exposure and cerebrovascular function in adolescent athletes. J Neurotrauma 38(7):837–847
Hart J, Kraut MA, Womack KB, Strain J, Didehbani N, Bartz E et al (2013) Neuroimaging of cognitive dysfunction and depression in aging retired National Football League players: a cross-sectional study. JAMA Neurol 70(3):326–335
Bailey DM, Jones DW, Sinnott A, Brugniaux JV, New KJ, Hodson D et al (1979) (2013), Impaired cerebral haemodynamic function associated with chronic traumatic brain injury in professional boxers, Clinical science (London. England 124(3):177–189
Veksler R, Vazana U, Serlin Y, Prager O, Ofer J, Shemen N et al (2020) Slow blood-to-brain transport underlies enduring barrier dysfunction in American football players. Brain 143(6):1826–1842
Doherty CP, O’Keefe E, Wallace E, Loftus T, Keaney J, Kealy J et al (2016) Blood-brain barrier dysfunction as a hallmark pathology in chronic traumatic encephalopathy. J Neuropathol Exp Neurol 75(7):656–662
Cherry JD, Tripodis Y, Alvarez VE, Huber B, Kiernan PT, Daneshvar DH et al (2016) Microglial neuroinflammation contributes to tau accumulation in chronic traumatic encephalopathy. Acta Neuropathol Commun 4(1):112
Hsu ET, Gangolli M, Su S, Holleran L, Stein TD, Alvarez VE et al (2018) Astrocytic degeneration in chronic traumatic encephalopathy. Acta Neuropathol 136(6):955–972
Holleran L, Kim JH, Gangolli M, Stein T, Alvarez V, McKee A et al (2017) Axonal disruption in white matter underlying cortical sulcus tau pathology in chronic traumatic encephalopathy. Acta Neuropathol 133(3):367–380
Provenzano FA, Jordan B, Tikofsky RS, Saxena C, Van Heertum RL, Ichise M (2010) F-18 FDG PET imaging of chronic traumatic brain injury in boxers: a statistical parametric analysis. Nucl Med Commun 31(11):952–957
Bang SA, Song YS, Moon BS, Lee BC, Lee HY, Kim JM et al (2016) Neuropsychological, metabolic, and GABAA receptor studies in subjects with repetitive traumatic brain injury. J Neurotrauma 33(11):1005–1014
Meabon JS, Huber BR, Cross DJ, Richards TL, Minoshima S, Pagulayan KF et al (2016) Repetitive blast exposure in mice and combat veterans causes persistent cerebellar dysfunction. Sci Transl Med 8(321):321ra6
Mantyh WG, Spina S, Lee A, Iaccarino L, Soleimani-Meigooni D, Tsoy E et al (2020) Tau positron emission tomographic findings in a former US football player with pathologically confirmed chronic traumatic encephalopathy. JAMA Neurol 77(4):517–521
Rabinovici GD, Gatsonis C, Apgar C, Chaudhary K, Gareen I, Hanna L et al (2019) Association of amyloid positron emission tomography with subsequent change in clinical management among medicare beneficiaries with mild cognitive impairment or dementia. JAMA 321(13):1286–1294
Stein TD, Montenigro PH, Alvarez VE, Xia W, Crary JF, Tripodis Y et al (2015) Beta-amyloid deposition in chronic traumatic encephalopathy. Acta Neuropathol 130(1):21–34
Johnson VE, Stewart W, Smith DH (2012) Widespread tau and amyloid-beta pathology many years after a single traumatic brain injury in humans. Brain Pathol 22(2):142–149
Johnson VE, Stewart W, Smith DH (2010) Traumatic brain injury and amyloid-β pathology: a link to Alzheimer’s disease? Nat Rev Neurosci 11(5):361
Ikonomovic MD, Uryu K, Abrahamson EE, Ciallella JR, Trojanowski JQ, Lee VM et al (2004) Alzheimer’s pathology in human temporal cortex surgically excised after severe brain injury. Exp Neurol 190(1):192–203
Chen XH, Johnson VE, Uryu K, Trojanowski JQ, Smith DH (2009) A lack of amyloid beta plaques despite persistent accumulation of amyloid beta in axons of long-term survivors of traumatic brain injury. Brain Pathol 19(2):214–223
Hong YT, Veenith T, Dewar D, Outtrim JG, Mani V, Williams C et al (2014) Amyloid imaging with carbon 11–labeled Pittsburgh compound B for traumatic brain injury. JAMA Neurol 71(1):23–31
Scott G, Ramlackhansingh AF, Edison P, Hellyer P, Cole J, Veronese M et al (2016) Amyloid pathology and axonal injury after brain trauma. Neurology 86(9):821–828
Asken BM, Mantyh WG, La Joie R, Strom A, Casaletto KB, Staffaroni AM, et al (2021) Association of remote mild traumatic brain injury with cortical amyloid burden in clinically normal older adults. Brain Imaging Behav (Online ahead of print; PMID:33432536)
Weiner MW, Harvey D, Hayes J, Landau SM, Aisen PS, Petersen RC et al (2017) Effects of traumatic brain injury and posttraumatic stress disorder on development of Alzheimer’s disease in Vietnam veterans using the Alzheimer’s Disease Neuroimaging Initiative: preliminary report. Alzheimer’s Dementia 3(2):177–188
Sugarman MA, McKee AC, Stein TD, Tripodis Y, Besser LM, Martin B et al (2019) Failure to detect an association between self-reported traumatic brain injury and Alzheimer’s disease neuropathology and dementia. Alzheimer’s Dementia 15(5):686–698
Wang ML, Wei XE, Yu MM, Li PY, Li WB (2017) Self-reported traumatic brain injury and in vivo measure of AD-vulnerable cortical thickness and AD-related biomarkers in the ADNI cohort. Neurosci Lett 655:115–120
Thompson PW, Ye L, Morgenstern JL, Sue L, Beach TG, Judd DJ et al (2009) Interaction of the amyloid imaging tracer FDDNP with hallmark Alzheimer’s disease pathologies. J Neurochem 109(2):623–630
Leung K (2004) 2-(4-(2-[(18)F]Fluoroethyl)piperidin-1-yl)benzo[4,5]imidazo[1,2-a]pyrimidine, Molecular Imaging and Contrast Agent Database (MICAD), National Center for Biotechnology Information (US), Bethesda (MD)
Agdeppa ED, Kepe V, Liu J, Flores-Torres S, Satyamurthy N, Petric A et al (2001) Binding characteristics of radiofluorinated 6-dialkylamino-2-naphthylethylidene derivatives as positron emission tomography imaging probes for beta-amyloid plaques in Alzheimer's disease. J Neurosci 21(24):Rc189
Harada R, Okamura N, Furumoto S, Tago T, Yanai K, Arai H et al (2016) Characteristics of tau and its ligands in PET Imaging. Biomolecules 6(1):7
Barrio JR, Small GW, Wong KP, Huang SC, Liu J, Merrill DA et al (2015) In vivo characterization of chronic traumatic encephalopathy using [F-18]FDDNP PET brain imaging. Proc Natl Acad Sci USA 112(16):E2039–E2047
Omalu B, Small GW, Bailes J, Ercoli LM, Merrill DA, Wong KP et al (2018) Postmortem autopsy-confirmation of antemortem [F-18]FDDNP-PET scans in a football player with chronic traumatic encephalopathy. Neurosurgery 82(2):237–246
Chen ST, Siddarth P, Merrill DA, Martinez J, Emerson ND, Liu J et al (2018) FDDNP-PET tau brain protein binding patterns in military personnel with suspected chronic traumatic encephalopathy1. J Alzheimer’s Disease 65(1):79–88
Omalu B, Small G, Bailes J, Ercoli L, Merrill D, Wong K et al (2018) Postmortem autopsy-confirmation of antemortem [F-18] FDDNP-PET scans in a football player with chronic traumatic encephalopathy. Neurosurgery 82:237–246
Soleimani-Meigooni DN, Iaccarino L, La Joie R, Baker S, Bourakova V, Boxer AL et al (2020) 18F-flortaucipir PET to autopsy comparisons in Alzheimer's disease and other neurodegenerative diseases. Brain 143(11):3477–3494
Ossenkoppele R, Rabinovici GD, Smith R, Cho H, Schöll M, Strandberg O et al (2018) Discriminative accuracy of [18F] flortaucipir positron emission tomography for Alzheimer disease vs other neurodegenerative disorders. JAMA 320(11):1151–1162
Lowe VJ, Lundt ES, Albertson SM, Min HK, Fang P, Przybelski SA et al (2020) Tau-positron emission tomography correlates with neuropathology findings. Alzheimer’s Dementia 16(3):561–571
Marquié M, Agüero C, Amaral AC, Villarejo-Galende A, Ramanan P, Chong MST et al (2019) [18 F]-AV-1451 binding profile in chronic traumatic encephalopathy: a postmortem case series. Acta Neuropathol Commun 7(1):164
Falcon B, Zivanov J, Zhang W, Murzin AG, Garringer HJ, Vidal R et al (2019) Novel tau filament fold in chronic traumatic encephalopathy encloses hydrophobic molecules. Nature 568(7752):420
Lee CM, Jacobs HIL, Marquié M, Becker JA, Andrea NV, Jin DS et al (2018) 18F-Flortaucipir binding in choroid plexus: related to race and hippocampus signal. J Alzheimer’s Dis 62(4):1691–1702
Baker SL, Harrison TM, Maass A, La Joie R, Jagust WJ (2019) Effect of off-target binding on (18)F-flortaucipir variability in healthy controls across the life span. J Nucl Med 60(10):1444–1451
Baker SL, Lockhart SN, Price JC, He M, Huesman RH, Schonhaut D et al (2017) Reference Tissue-Based Kinetic Evaluation of 18F-AV-1451 for Tau Imaging, Journal of nuclear medicine : official publication, Society of. Nuclear Medicine 58(2):332–338
Johnson KA, Schultz A, Betensky RA, Becker JA, Sepulcre J, Rentz D et al (2016) Tau positron emission tomographic imaging in aging and early Alzheimer disease. Ann Neurol 79(1):110–119
Mitsis EM, Riggio S, Kostakoglu L, Dickstein DL, Machac J, Delman B et al (2014) Tauopathy PET and amyloid PET in the diagnosis of chronic traumatic encephalopathies: studies of a retired NFL player and of a man with FTD and a severe head injury. Transl Psychiatry 4(9):e441
Stern RA, Adler CH, Chen K, Navitsky M, Luo J, Dodick DW et al (2019) Tau positron-emission tomography in former national football league players. N Engl J Med 380(18):1716–1725
Tanner JA, Rabinovici GD (2021) Relationship between tau and cognition in the evolution of Alzheimer's disease: new insights from tau PET. J Nucl Med 62(5):612–613
Wang YT, Edison P (2019) Tau imaging in neurodegenerative diseases using positron emission tomography. Curr Neurol Neurosci Rep 19(7):45
Endo H, Shimada H, Sahara N, Ono M, Koga S, Kitamura S et al (2019) In vivo binding of a tau imaging probe, [(11) C]PBB3, in patients with progressive supranuclear palsy. Mov Disord 34(5):744–754
Tagai K, Ono M, Kubota M, Kitamura S, Takahata K, Seki C et al (2021) High-contrast in vivo imaging of tau pathologies in Alzheimer's and non-Alzheimer's disease tauopathies. Neuron 109(1):42–58
Takahata K, Kimura Y, Sahara N, Koga S, Shimada H, Ichise M et al (2019) PET-detectable tau pathology correlates with long-term neuropsychiatric outcomes in patients with traumatic brain injury. Brain 142(10):3265–3279
Aguero C, Dhaynaut M, Normandin MD, Amaral AC, Guehl NJ, Neelamegam R et al (2019) Autoradiography validation of novel tau PET tracer [F-18]-MK-6240 on human postmortem brain tissue. Acta Neuropathol Commun 7(1):37
Betthauser TJ, Cody KA, Zammit MD, Murali D, Converse AK, Barnhart TE et al (2019) In vivo characterization and quantification of neurofibrillary tau PET radioligand 18F-MK-6240 in humans from Alzheimer disease dementia to young controls. J Nucl Med 60(1):93–99
Krishnadas N, Doré V, Lamb F, Groot C, McCrory P, Guzman R et al (2020) Case Report: (18)F-MK6240 tau positron emission tomography pattern resembling chronic traumatic encephalopathy in a retired australian rules football player. Front Neurol 11:
Cherry JD, Kim SH, Stein TD, Pothast MJ, Nicks R, Meng G et al (2020) Evolution of neuronal and glial tau isoforms in chronic traumatic encephalopathy. Brain pathology (Zurich, Switzerland) 30(5):913–925
Arena JD, Smith DH, Lee EB, Gibbons GS, Irwin DJ, Robinson JL et al (2020) Tau immunophenotypes in chronic traumatic encephalopathy recapitulate those of ageing and Alzheimer’s disease. Brain 143(5):1572–1587
Palleis C, Sauerbeck J, Beyer L, Harris S, Schmitt J, Morenas-Rodriguez E et al (2020) In vivo assessment of neuroinflammation in 4-repeat tauopathies. Mov Disord 36(4):883–894
Needham EJ, Helmy A, Zanier ER, Jones JL, Coles AJ, Menon DK (2019) The immunological response to traumatic brain injury. J Neuroimmunol 332:112–125
Kreisl WC, Kim MJ, Coughlin JM, Henter ID, Owen DR, Innis RB (2020) PET imaging of neuroinflammation in neurological disorders. The Lancet Neurology 19(11):940–950
Wilson H, Politis M, Rabiner EA, Middleton LT (2020) Novel PET biomarkers to disentangle molecular pathways across age-related neurodegenerative diseases. Cells 9(12):2581
Holland N, Jones PS, Savulich G, Wiggins JK, Hong YT, Fryer TD et al (2020) Synaptic loss in primary tauopathies revealed by [(11) C]UCB-j positron emission tomography. Mov Disord 35(10):1834–1842
Mansur A, Rabiner EA, Comley RA, Lewis Y, Middleton LT, Huiban M et al (2020) Characterization of 3 PET tracers for quantification of mitochondrial and synaptic function in healthy human brain: (18)F-BCPP-EF, (11)C-SA-4503, and (11)C-UCB-J. J Nucl Med 61(1):96–103
Heurling K, Ashton NJ, Leuzy A, Zimmer ER, Blennow K, Zetterberg H et al (2019) Synaptic vesicle protein 2A as a potential biomarker in synaptopathies. Mol Cell Neurosci 97:34–42
Mecca AP, Chen MK, O’Dell RS, Naganawa M, Toyonaga T, Godek TA et al (2020) In vivo measurement of widespread synaptic loss in Alzheimer’s disease with SV2A PET. Alzheimer’s Dementia 16(7):974–982
Mihalik JP, Amalfe SA, Roby PR, Ford CB, Lynall RC, Riegler KE et al (2020) Sex and sport differences in college lacrosse and soccer head impact biomechanics. Med Sci Sports Exerc 52(11):2349–2356
Reyes J, Mitra B, McIntosh A, Clifton P, Makdissi M, Nguyen JVK et al (2020) An investigation of factors associated with head impact exposure in professional male and female australian football players. Am J Sports Med 48(6):1485–1495
Alsalaheen B, Johns K, Bean R, Almeida A, Eckner J, Lorincz M (2019) Women and men use different strategies to stabilize the head in response to impulsive loads: implications for concussion injury risk. J Orthop Sports Phys Ther 49(11):779–786
Gallagher V, Kramer N, Abbott K, Alexander J, Breiter H, Herrold A et al (2018) The effects of sex differences and hormonal contraception on outcomes after collegiate sports-related concussion. J Neurotrauma 35(11):1242–1247
Dougan BK, Horswill MS, Geffen GM (2014) Athletes’ age, sex, and years of education moderate the acute neuropsychological impact of sports-related concussion: a meta-analysis. J Int Neuropsychol Soc 20(1):64–80
Iverson GL, Gardner AJ, Terry DP, Ponsford JL, Sills AK, Broshek DK et al (2017) Predictors of clinical recovery from concussion: a systematic review. Br J Sports Med 51(12):941–948
Dubal DB (2020) Sex difference in Alzheimer’s disease: An updated, balanced and emerging perspective on differing vulnerabilities. Handb Clin Neurol 175:261–273
Ullah MF, Ahmad A, Bhat SH, Abu-Duhier FM, Barreto GE, Ashraf GM (2019) Impact of sex differences and gender specificity on behavioral characteristics and pathophysiology of neurodegenerative disorders. Neurosci Biobehav Rev 102:95–105
Bernick C, Banks S, Phillips M, Lowe M, Shin W, Obuchowski N et al (2013) Professional fighters brain health study: rationale and methods. Am J Epidemiol 178(2):280–286
Walker WC, Carne W, Franke LM, Nolen T, Dikmen SD, Cifu DX et al (2016) The chronic effects of neurotrauma consortium (CENC) multi-centre observational study: description of study and characteristics of early participants. Brain Inj 30(12):1469–1480
Yue JK, Vassar MJ, Lingsma HF, Cooper SR, Okonkwo DO, Valadka AB et al (2013) Transforming research and clinical knowledge in traumatic brain injury pilot: multicenter implementation of the common data elements for traumatic brain injury. J Neurotrauma 30(22):1831–1844
Valera EM, Cao A, Pasternak O, Shenton ME, Kubicki M, Makris N et al (2019) White matter correlates of mild traumatic brain injuries in women subjected to intimate-partner violence: a preliminary study. J Neurotrauma 36(5):661–668
Acknowledgements
We thank Corrina Fonseca, Renaud La Joie, Amelia Strom, and Nidhi Mundada for their assistance with preparation of structural MRI and PET images, with an additional thank you to Dr. La Joie for lending interpretations of the PET scans. We are especially thankful for the research participants who generously committed their time and effort to research projects at UCSF during life, and for their brain donation to the UCSF Neurodegenerative Disease Brain Bank. Neuropathologic findings for the two patient examples were derived from autopsy reports prepared by Drs. William Seeley or Salvatore Spina from the UCSF Memory and Aging Center Neurodegenerative Disease Brain Bank.
Funding
We thank the UCSF Alzheimer’s Disease Research Center (NIA P50AG023501 and P30AG062422; PI: Bruce Miller) and Rainwater Charitable Foundation (PI: Gil Rabinovici) for their funding support. Funding agencies did not play a role in design or interpretation of data in this manuscript.
Author information
Authors and Affiliations
Contributions
BMA drafted the manuscript. GDR revised and was a major contributor in writing the manuscript. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The two patients described from the UCSF Alzheimer’s Disease Research Center consented to participate in all IRB-approved study protocols. Identifiable information was redacted from reported data.
Competing interests
BMA and GDR declare that they have no competing interests relevant this review.
Consent for publication
Individual consent was obtained from each participant at the time of study enrollment.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Asken, B.M., Rabinovici, G.D. Identifying degenerative effects of repetitive head trauma with neuroimaging: a clinically-oriented review. acta neuropathol commun 9, 96 (2021). https://doi.org/10.1186/s40478-021-01197-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40478-021-01197-4