Abstract
Purpose
For women with locoregionally advanced cervical cancer, the standard of care treatment is the curatively intended chemoradiation therapy (CRT). A relationship between bone marrow (BM) dose–volume histograms (DVHs) and acute hematological toxicity (HT) has been debated recently. Aim of this study was the evaluation of BM dose constraints and HT in a contemporary patient cohort.
Methods
Radiation treatment plans of 31 patients with cervical cancer (FIGO stage IIB–IVB) treated with intensity-modulated radiotherapy and simultaneous chemotherapy were explored retrospective. Pelvic bones (PB) and femoral heads (FH) were contoured and DVHs were correlated with white blood cells (WBC), hemoglobin levels and platelets.
Results
Comparing the absolute blood levels with the dose volumes of both FH and PB the data showed a significant correlation between WBC and the median dose of the FH and the median dose, V30Gy, V40Gy and V50Gy of the PB. A correlation between the toxicity grade of anemia and mean dose, maximum dose and V5Gy of the PB was found. Counting the highest grade of HT of all three blood levels of each patient, significant correlations were found for the mean and median dose, V30Gy, V40Gy and V50Gy of the PB.
Conclusion
The results show that blood levels may correlate with distinct dosimetric subvolumes of critical bone marrow compartments with a potential impact on therapeutic outcome and treatment-related toxicity. The data presented are in line with the previous findings on the relevance of dosimetric exposure of pelvic bony subvolumes.
Similar content being viewed by others
Introduction
For women with loco-regionally advanced cervical cancer FIGO stage IIA–IVA the current standard of care treatment is pelvic external beam radiotherapy and concurrent cisplatin-based chemotherapy [1,2,3]. Acute and late toxicity remain a challenge and are still common in multimodal therapy protocols. Furthermore, incidental dose deposition in the adjacent pelvic and vertebral bone structures may contribute to chemotherapy-related bone marrow (BM) suppression [4]. Both, radiotherapy (RT) and chemotherapy (CT) are responsible for BM damage and may cause leukopenia, which may represent a severe dose-limiting side effect [5,6,7]. With the implementation of intensity-modulated RT (IMRT) and volumetric-modulated arc therapy (VMAT) the applied dose to pelvic organs at risk can be reduced and subsequently lead to fewer side effects in the irradiation of pelvic tumors [5, 8,9,10].
The purpose of this study was to examine a correlation between hematotoxicity (HT) and dose–volume parameters of irradiated BM in cervical cancer patients who underwent curatively intended chemoradiation (CRT).
Patients and methods
Patients and treatment
The cohort in this study included 31 consecutive cervical cancer patients treated between 2010 and 2016 with definitive CRT at the Department of Radiation Oncology at the Klinikum rechts der Isar, Munich. A total of 24 patients without paraaortic RT was included in the presented dosimetric analysis. Details of the whole cohort are listed in Table 1.
Some patients had relevant comorbidities. Seven patients suffered from concomitant nephrological diseases (renal insufficiency: n = 3, a nonfunctioning kidney: n = 1, partial kidney resection due to a cyst: n = 1, nephrolithiasis: n = 1, history of acute renal failure: n = 1) and 3 patients suffered from concomitant cardiological diseases (atrial fibrillation: n = 1, history of after PTCA: n = 1, undefined heart disease: n = 1).
Simultaneously with percutaneous radiotherapy, 29 patients received chemotherapy. Twenty-two patients received cisplatin 40 mg/m2 (2 cycles (n = 1), 3 cycles (n = 6), 4 cycles (n = 5), 5 cycles (n = 4) and 6 cycles (n = 6)]; one patient was switched to carboplatin AUC2 after 4 cycles due to a low glomerular filtration rate (GFR). One patient each received only carboplatin AUC2 (4 cycles), vinorelbine 40 mg/m2 (7 cycles) and vinorelbine 70 mg/m2 (4 cycles). Four patients received vinorelbine 15 mg/m2 (5 cycles (n = 2) and 6 cycles (n = 2) due to low renal function. Two patients refused chemotherapy.
Technical details
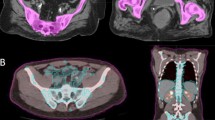
All patients underwent planning computed tomography in supine position with intravenous contrast medium and 5 mm slices. The clinical target volume (CTV) was based on common target volume delineation guidelines (RTOG) and consisted of the uterus, cervix, parametria, upper half of the vagina if involved and regional lymph nodes. The paraaortic nodes were included if radiographically involved and a planning target volume (PTV) was defined using an isotropic margin around the CTV of 10 mm adopted to anatomical structures. Six patients were treated in IMRT technique with helical tomotherapy, 23 patients had a VMAT and two patients had a step-and-shoot IMRT plan.
Twenty-seven patients underwent curative definitive therapy, two patients received a palliative concept, one patient switched from palliative to curative treatment and one patient from a curative to a palliative concept. The dose to the tumor region was 50.4 á 1.8 Gy (n = 22) or 45 á 1.8 (n = 8). One patient received once a single fraction of 2 Gy and then 1.8 Gy to a total dose of 50.6 Gy. In 8 patients the paraoartical lymph nodes were included in the treatment plan. Thirteen patients received a boost to pathological lymph nodes. The mean value of the total radiation dose was 54.5 Gy, for the lymphatic drainage 51.5 Gy and for the pathologic lymph nodes 55.5 Gy.
Brachytherapy (BT) was performed in 24 patients (mean value 23.7 Gy) after external beam RT based on MRI planning encompassing the residual tumor at the time of BT planning with single doses of 5 (n = 5) or 7 Gy (n = 18). One patient received twice BT in PDR-AL technic with 0.4 Gy/h with a total dose of 16 Gy/session. Dose prescription and dose constraints were followed according to GEC-ESTRO criteria [11].
Definition of bone marrow-relevant substructures
The pelvic bone included the os sacrum, os ilium, os ischii and os pubis. The femoral head included the upper femur, the bone cortex was also included. The lumbar spine was not included. The dosimetric parameters were defined as the volumes of a definite radiation dose, such as Vx means the total volume of the bone that received the radiation dose of X Gy. In addition, the analyzed parameters included the V5, V10, V20, V30, V40, V50, and the minimal, maximal and mean doses. Patients with paraaortic RT were excluded from dosimetric analyses of BM subvolumes.
Toxicity assessment
The hematological data, including WBC, hemoglobin concentration and platelet count were recorded from laboratory studies performed under CRT. All available information about the relevant acute therapy side effects according CTCAE and RTOG criteria (nausea, leucopenia, anemia, thrombopenia, loss of weight, diarrhea, skin reaction, fatigue, vaginal mucositis, urological side effects) were assembled out of the patient files. For the correlation of the blood levels the nadir of WBCs, hemoglobin levels and thrombopenia during CRT were analyzed.
Statistics
The overall survival (OS) and progression-free survival (PFS) were estimated according to Kaplan–Meier. Pearson correlation coefficient (PCC) was calculated for the correlation of absolute blood levels and PB and FH constraints. Spearman correlation coefficient as well as logistic regression and scatter plots were used for the correlation of blood levels according to CTCAE.
Results
Overall survival and progression-free survival
The mean OS was 30 months (range 3–82 months) with 11 deaths reported. PFS was defined as absence of loco-regional or distant metastatic failure. The PFS was 17.4 months (range 0–63 months). Referring to RECIST criteria 11 patients had a complete response after CRT. Nine patients were in partial remission; two patients had a stable disease and seven patients had a progressive disease with distant metastases.
Hematologic toxicity
Regarding information about the relevant acute and late therapy side effects three patients had a grade 4 acute toxicity according to CTCAE criteria for leukopenia (n = 2) and diarrhea (n = 1). Grade-3 acute toxicity existed for leukopenia (n = 17), anemia (n = 5), thrombopenia (n = 3), diarrhea (n = 2), nausea (n = 6), vaginal bleeding (n = 1) and dysuria (n = 2). Except for one patient suffering from grade-3 loss of weight (according to late toxicity RTOG criteria) only grade 1 and 2 late toxicities occurred.
Correlation of blood levels and PB and FH constraints
Comparing the absolute blood levels with the dose volumes of both FH and PB the data showed a significant correlation between WBC and the median dose of the FH and the median dose, V30Gy, V40Gy and V50Gy of the PB (Table 2). A correlation between the toxicity grade of anemia and mean dose, maximum dose and V5Gy of the PB was found. Counting the highest grade of HT of all three blood levels of each patient, significant correlations were found for the mean and median dose, V30Gy, V40Gy and V50Gy of the PB. Further dosimetric details of BM subsites are presented in Table 3.
Discussion
In our analysis of cervical cancer patients undergoing CRT with IG-VMAT, we were able to identify a defined subset of BM dose–volume parameters that seem to correlate with different forms of HT. Notably, intermediate and higher doses (subvolumes receiving 30–50 Gy) of the PB had a negative impact on WBC and mean dose as well as lower doses (V5Gy) lead to higher HT in terms of anemia. Correlations of the dose–volume parameters with HT according to CTCAE by logistic regression failed to show any correlation. Scatter plots though showed an apparent correlation with a tendency to higher toxicity grades with higher radiated dose volumes so that probably a larger patient cohort is necessary to show a significance.
Previous studies have already evaluated associations between dose–volume metrics on BM and the development of HT, although most of them were retrospective analyses [6, 12,13,14,15,16]. Table 4 gives an updated overview of recent studies that examined the influence of BM dose–volume parameters and HT in cervical cancer patients undergoing (IG-)IMRT/VMAT-based CRT.
Zhang and colleagues retrospectively examined outcomes of 117 patients undergoing CRT with IMRT/VMAT. The V5Gy, V10Gy, V20Gy, and V30Gy of BM correlated significantly with lymphocytic toxicity. A strong limitation was the uncommon use of induction chemotherapy and a concomitant chemotherapy with Paclitaxel and Cisplatin, which makes comparison with other work considerably more difficult. The group of Chen et al. performed a retrospective analysis of 69 patients undergoing CRT with IMRT/VMAT. They subdivided the BM into ilium (IL), lower pelvis (LP) and lumbosacral spine (LS) and evaluated dosimetric predictors of BM toxicity. The authors only found a difference in patients who had more chemotherapy cycles (5–6 vs. 3–4), so one can assume that BM toxicity was possibly masked by the amount of BM-suppressing cytostatic therapy. In the group with less CT cycles the relative IL-V15, relative IL-V50 and absolute LP-V50 correlated with the neutrophil nadir.
Although most of this work has defined the bony structures as BM equivalent, some authors proceed methodologically differently. These take positron emission tomography (PET) as the basis of the BM definition to define active BM [13, 17]. The FDG uptake in PET/CT scans can define active BM regions and correlates with the number of hematopoietic marrow cells [7, 18]. The uptake within the radiation field decreases after treatment and is variable across irradiated bone sites, which indicates myelosuppression [18]. In conjunction with the use of modern radiation techniques such as IMRT and VMAT, this methodology offers greater accuracy when trying to spare relevant BM subvolumes in order to reduce toxicity.
The group of Mell and colleagues initiated a remarkable prospective multicenter phase II trial, which examined for the first time the dosimetric impact and relevance of PET-based BMS-IG-IMRT [13]. The BM constraints used were V10Gy and V20Gy < 90% and < 75%, respectively. The results showed that V10Gy/V20Gy/V30Gy/V40Gy were considerably lower with IG-IMRT and led to significantly less grade-3 neutropenia. The same group was able to set up the international phase-II/-III trial (INTERTECC) that accrued 101 patients, which is also the most relevant study in this field today[19]. The question of the study was whether PET-based bone marrow sparing IG-IMRT reduces toxicity compared to standard IG-IMRT. The results showed a significant lower incidence of acute grade ≥ 3 neutropenia in the PET-BMS-IMRT group as compared to IMRT (19% versus 54%), but no difference in post-treatment ALC by treatment group. Furthermore, according to the authors there was no evidence that PET-BMS-IMRT affected chemotherapy delivery or long-term outcomes. However, only 29 out of 101 patients were finally enrolled in the phase-III part and a possible bias cannot be excluded.
Although the studies by Zhang, Chen and Mell showed an effect on neutropenia or lymphopenia even at low doses (V10Gy, V20Gy, IL-V15), we were only able to detect a correlation in our cohort at higher doses (V30-50). The fact that a correlation between Hb value and V5Gy, mean and maximum dose was found in the PB in our study was not seen in any of the other studies, so that we must assume that this is most likely an artifact.
Several studies have now been able to show that the BM dose can safely be reduced by IG-VMAT or, at best, the targeted use of BM-protective constraints leads to lower toxicities. Nevertheless, the clinical relevance of these efforts has not yet been proven beyond doubt. A recent meta-analysis on this topic was also able to confirm that protecting the pelvic bones can lead to a reduction in the bone marrow dose and HT [20]. At the same time, however, the authors admitted that a clinical benefit of these measures in the broad is still pending. Despite the lack of clear evidence of superiority, sparing of the relevant BM structures can generally be achieved through modern radiation planning and without compromising target volume coverage or increasing other toxicities (gastrointestinal, genitourinary). Based on our own data and the literature discussed, we prepared a tabular summary in which useful BM constraints from previous studies are suggested (Table 5) [12, 14, 19, 21, 22].
Finally, our study had several limitations due to the small patient group and the retrospectively gained data and needs a prospective cohort to affirm these findings. Owing to the low patient number, a logistic regression model to correlate the different CTCAE toxicity grades with the dose volumes was not robust enough.
However, the results of this and previous studies show that HT correlates with distinct subvolumes in FH and PB.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- HT:
-
Hematotoxicity
- ABM:
-
Active bone marrow
- BM:
-
Bone marrow
- BMS:
-
Bone marrow sparing
- cc:
-
Cubic centimeter
- CRT:
-
Chemoradiation
- CTCAE:
-
Common toxicity criteria
- DVH:
-
Dose–volume histogram
- IMRT:
-
Intensity-modulated radiation therapy
- IG:
-
Image-guided
- HT:
-
Hematotoxicity
- ALC:
-
Absolute lymphocyte count
- PB:
-
Pelvic bone
- PET:
-
Positron emission tomography
- VMAT:
-
Volumetric-modulated radiation therapy
References
Koh WJ, Abu-Rustum NR, Bean S, Bradley K, Campos SM, Cho KR, et al. Cervical cancer, version 3 2019 NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2019;17(1):64–84.
Eifel PJ, Winter K, Morris M, Levenback C, Grigsby PW, Cooper J, et al. Pelvic irradiation with concurrent chemotherapy versus pelvic and para-aortic irradiation for high-risk cervical cancer: an update of radiation therapy oncology group trial (RTOG) 90–01. J Clin Oncol. 2004;22(5):872–80.
Rose PG, Bundy BN, Watkins EB, Thigpen JT, Deppe G, Maiman MA, et al. Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med. 1999;340(15):1144–53.
Torres MA, Jhingran A, Thames HD Jr, Levenback CF, Bodurka DC, Ramondetta LM, et al. Comparison of treatment tolerance and outcomes in patients with cervical cancer treated with concurrent chemoradiotherapy in a prospective randomized trial or with standard treatment. Int J Radiat Oncol Biol Phys. 2008;70(1):118–25.
Brixey CJ, Roeske JC, Lujan AE, Yamada SD, Rotmensch J, Mundt AJ. Impact of intensity-modulated radiotherapy on acute hematologic toxicity in women with gynecologic malignancies. Int J Radiat Oncol Biol Phys. 2002;54(5):1388–96.
Rose BS, Aydogan B, Liang Y, Yeginer M, Hasselle MD, Dandekar V, et al. Normal tissue complication probability modeling of acute hematologic toxicity in cervical cancer patients treated with chemoradiotherapy. Int J Radiat Oncol Biol Phys. 2011;79(3):800–7.
Rose BS, Liang Y, Lau SK, Jensen LG, Yashar CM, Hoh CK, et al. Correlation between radiation dose to (1)(8)F-FDG-PET defined active bone marrow subregions and acute hematologic toxicity in cervical cancer patients treated with chemoradiotherapy. Int J Radiat Oncol Biol Phys. 2012;83(4):1185–91.
Regnier A, Ulbrich J, Munch S, Oechsner M, Wilhelm D, Combs SE, et al. Comparative analysis of efficacy, toxicity, and patient-reported outcomes in rectal cancer patients undergoing preoperative 3D conformal radiotherapy or VMAT. Front Oncol. 2017;7:225.
Gandhi AK, Sharma DN, Rath GK, Julka PK, Subramani V, Sharma S, et al. Early clinical outcomes and toxicity of intensity modulated versus conventional pelvic radiation therapy for locally advanced cervix carcinoma: a prospective randomized study. Int J Radiat Oncol Biol Phys. 2013;87(3):542–8.
Mazzola R, Ricchetti F, Fiorentino A, Levra NG, Fersino S, Di Paola G, et al. Weekly cisplatin and volumetric-modulated Arc therapy with simultaneous integrated boost for radical treatment of advanced cervical cancer in elderly patients: feasibility and clinical preliminary results. Technol Cancer Res Treat. 2017;16(3):310–5.
Kirisits C, Potter R, Lang S, Dimopoulos J, Wachter-Gerstner N, Georg D. Dose and volume parameters for MRI-based treatment planning in intracavitary brachytherapy for cervical cancer. Int J Radiat Oncol Biol Phys. 2005;62(3):901–11.
Kumar T, Schernberg A, Busato F, Laurans M, Fumagalli I, Dumas I, et al. Correlation between pelvic bone marrow radiation dose and acute hematological toxicity in cervical cancer patients treated with concurrent chemoradiation. Cancer Manag Res. 2019;11:6285–97.
Mell LK, Sirak I, Wei L, Tarnawski R, Mahantshetty U, Yashar CM, et al. Bone marrow-sparing intensity modulated radiation therapy with concurrent cisplatin for stage IB-IVA cervical cancer: an international multicenter phase II clinical trial (INTERTECC-2). Int J Radiat Oncol Biol Phys. 2017;97(3):536–45.
Zhou YM, Freese C, Meier T, Go D, Khullar K, Sudhoff M, et al. The absolute volume of PET-defined, active bone marrow spared predicts for high grade hematologic toxicity in cervical cancer patients undergoing chemoradiation. Clin Transl Oncol. 2018;20(6):713–8.
Chen M, Wang D, Bao Z, Yi Z, Mei Z, Sun S, et al. The impact of bone marrow irradiation dose on acute haematologic toxicity in cervical cancer patients treated with concurrent chemoradiotherapy. Radiat Oncol. 2023;18(1):66.
Zhang BZ, Li Y, Xu LM, Chai YL, Qu C, Cao YJ, et al. The relationship between the radiation dose of pelvic-bone marrow and lymphocytic toxicity in concurrent chemoradiotherapy for cervical cancer. Radiat Oncol. 2023;18(1):12.
McGuire SM, Menda Y, Ponto LL, Gross B, Juweid M, Bayouth JE. A methodology for incorporating functional bone marrow sparing in IMRT planning for pelvic radiation therapy. Radiother Oncol. 2011;99(1):49–54.
Yagi M, Froelich J, Arentsen L, Shanley R, Ghebre R, Yee D, et al. Longitudinal FDG-PET revealed regional functional heterogeneity of bone marrow, site-dependent response to treatment and correlation with hematological parameters. J Cancer. 2015;6(6):531–7.
Williamson CW, Sirak I, Xu R, Portelance L, Wei L, Tarnawski R, et al. Positron emission tomography-guided bone marrow-sparing radiation therapy for locoregionally advanced cervix cancer: final results from the INTERTECC phase II/III trial. Int J Radiat Oncol Biol Phys. 2022;112(1):169–78.
Zhou P, Zhang Y, Luo S, Zhang S. Pelvic bone marrow sparing radiotherapy for cervical cancer: a systematic review and meta-analysis. Radiother Oncol. 2021;165:103–18.
Albuquerque K, Giangreco D, Morrison C, Siddiqui M, Sinacore J, Potkul R, et al. Radiation-related predictors of hematologic toxicity after concurrent chemoradiation for cervical cancer and implications for bone marrow-sparing pelvic IMRT. Int J Radiat Oncol Biol Phys. 2011;79(4):1043–7.
Mell LK, Kochanski JD, Roeske JC, Haslam JJ, Mehta N, Yamada SD, et al. Dosimetric predictors of acute hematologic toxicity in cervical cancer patients treated with concurrent cisplatin and intensity-modulated pelvic radiotherapy. Int J Radiat Oncol Biol Phys. 2006;66(5):1356–65.
Funding
Open Access funding enabled and organized by Projekt DEAL. Not applicable.
Author information
Authors and Affiliations
Contributions
DH, SP and SEC treated the patients and provided the data and study infrastructure. DH and DBH developed the study design. CK collected the data and performed the statistical analysis. DBH and DH reviewed the data. DBH and DH drafted the manuscript. DH made substantial contributions to conception of the study, interpreted the data and revised the manuscript. MK, SEC, SP and CK contributed significantly to the discussion and interpretation of the results. All co-authors read and approved the final manuscript. On behalf of all authors, the corresponding author states that there is no conflict of interest.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study has been approved by the ethics committee of the Klinikum rechts der Isar, School of Medicine, Technical University of Munich (TUM), Munich, Germany. File number: 141/17 S. According to the bavarian hospital code, article 27, there was no necessity of consent to participate as the data were used anonymously. There was no manipulation of independent variables regarding the treatment.
Consent for publication
According to the Bavarian hospital law, article 27, there was no necessity of consent for publication as the data were used anonymously.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hallqvist, D., Kormann, C., Pigorsch, S. et al. Bone marrow toxicity in patients with locally advanced cervical cancer undergoing multimodal treatment with VMAT/IMRT: are there dosimetric predictors for toxicity?. Eur J Med Res 29, 445 (2024). https://doi.org/10.1186/s40001-024-02041-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-024-02041-w