Abstract
Background
Cauda equina syndrome is a rare clinical condition that requires prompt diagnosis and timely surgical decompression with postoperative rehabilitation to prevent devastating complications.
Case presentation
A 55-year-old Sinhalese woman presented with a vulval abscess, with a history of involuntary leakage of urine for the last 7 years. Her sexual activity has been compromised due to coital incontinence, and she had also been treated for recurrent urinary tract infections during the last 7 years. On examination, a distended bladder was found. Neurological examination revealed a saddle sensory loss of S2–S4 dermatomes. There was no sensory loss over the lower limbs. Bladder sensation was absent, but there was some degree of anal sphincter tone. Motor functions and reflexes were normal in the limbs. Magnetic resonance imaging revealed L5–S1 spondylolisthesis. Ultrasound imaging confirmed the finding of a distended bladder, in addition to bilateral hydroureters with hydronephrosis. An incision and drainage with concomitant intravenous antibiotics were started for the vulval abscess. An indwelling catheter was placed to decompress the bladder and to reduce vulval excoriations due to urine. Bilateral ureteric stenting was performed later for persistent hydronephrosis and hydroureter despite an empty bladder.
Conclusion
This is a tragic case that illustrates the devastating long-term sequelae that ensues if cauda equina syndrome is left undiagnosed. It reiterates the importance of prompt referral and surgical decompression.
Similar content being viewed by others
Background
Cauda equina syndrome (CES) is a rare condition with an incidence of 1 in 100,000 in the population, typically presenting with severe lower back pain, sciatica, genital sensory disturbance, and bladder or bowel dysfunction [1, 2]. It requires prompt diagnosis, appropriate investigations, and timely surgical decompression with postoperative rehabilitation to achieve a satisfactory outcome [2, 3]. Unfortunately, due to its rarity, it has become difficult to achieve a satisfactory outcome in a significant proportion of cases [2].
Cauda equina syndrome (CES) comes under two classifications, incomplete cauda equina syndrome (CES-I) and complete cauda equina syndrome with true retention (CES-R)
In CES-I, patients present with motor and sensory symptoms, including saddle anesthesia, but have yet to develop retention or incontinence of either bowel or bladder. At this point, immediate surgical intervention is needed, which gives the best chance of a full recovery. In CES-R, patients have already developed painless urinary retention and overflow incontinence. Decompression of the cauda equina nerves is still likely to be required, but there is a lesser chance of recovery of lost neurological function. It is vital to diagnose the condition before it deteriorates from CES-I to CES-R as the surgical outcome for patients with CES-I is generally favorable, whereas those with CES-R have a poorer prognosis, although around 70% of patients with CES-R have a socially acceptable long-term outcome [4].
More often than not, the outcome is already decided by the time of admission owing to a delay in presentation or referral, especially in low-resource settings. We present a tragic case of cauda equina syndrome with devastating long-term complications.
Case presentation
A 55-year-old Sinhalese woman presented to the gynecology ward with a vulval abscess. She also complained of involuntary leakage of urine for the last 7 years. The incontinence was throughout both day and night. She did not have an urge to pass urine. The urinary flow was intermittent. There was no fecal incontinence. Sexual activity was also compromised due to coital incontinence.
Over the last 7 years, she had been admitted on three occasions for urinary tract infections to a gynecology ward at a tertiary hospital. The reason for pyelonephritis on the last admission was attributed to hydronephrosis. She had also been on clinic follow-up for urinary incontinence and had been treated with antimuscarinics and lifestyle modifications. She had not undergone any surgery for urinary incontinence. As there had not been any improvement, she had later defaulted follow-up.
On abdominal examination, a distended bladder was found. Neurological examination revealed a saddle sensory loss of S2–S4 dermatomes. There was no sensory loss over the lower limbs. Bladder sensation was absent, but there was some degree (reduced) of anal sphincter tone. Motor functions and reflexes were normal in the limbs.
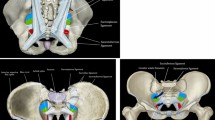
Magnetic resonance imaging (MRI) revealed L5–S1 spondylolisthesis (Fig. 1). Computerized tomography (CT) of the brain was normal. Ultrasound imaging revealed a distended bladder with bilateral hydroureter and hydronephrosis.
An incision and drainage with concomitant intravenous antibiotics were started for the vulval abscess. An indwelling catheter was placed to decompress the distended bladder and to reduce vulval excoriations due to urine. Despite bladder decompression, serum creatinine remained elevated with persistent bilateral hydronephrosis indicative of secondary bilateral vesicoureteric junctional obstruction due to a grossly thickened bladder wall. Thus, bilateral ureteric stents were placed. Subsequently the serum creatinine improved from 6.54 to 2.57 mg/dL, and upper tract dilation reduced significantly.
Discussion
This case illustrates the failure to recognize the presence of acute CES, which was likely due to an atypical presentation, low index of suspicion, and improper follow-up. This delay in appropriate therapy led to the catastrophic sequelae.
Unfortunately, only one-fifth of the patients present with the classical triad of bilateral sciatica with lower limb weakness, saddle anesthesia, and sphincter disturbance [5]. In this patient, the atypical presentation of the loss of sensation in the perineum in the absence of sciatica and lower limb weakness probably accounted for the initial delay in presentation. During this admission, the vulval abscess prompted the detection of the saddle sensory loss that had not been picked up even by the patient. Thereafter, piecing together of the evidence of the clinical evaluation, that is, vulval abscess, saddle sensory loss, overflow incontinence, hydronephrosis, renal compromise, and MRI evidence, gave the complete picture (Fig. 2). The timeline of the development of complications is shown in Fig. 3.
Unfortunately, if the bladder dysfunction was properly evaluated during previous admissions, an overflow incontinence due to a neurogenic bladder would have been elicited by clinical evaluation alone. This would have, in turn, prompted a neurological examination that would have revealed a CES. A painless urine retention in CES leads to permanent bladder damage from irreversible stretching of the bladder wall resulting in a palpable bladder. Therefore, it is essential in a case of neurogenic bladder dysfunction to screen for CES, even if they do not present with classic symptoms [6]. Although this is basic undergraduate knowledge, it is common practice to look for urogynecological causes for incontinence rather than rare neurological causes. This compartmentalization of clinical features and the lack of a holistic approach to patient management is a result of involvement of multiple specialists in patient care. If catastrophes of this nature are to be prevented, actual discussion among clinicians and not mere referrals are needed, especially in the current concept of multidisciplinary care.
Diagnostic imaging with computerized tomography (CT) scan or magnetic resonance imaging (MRI) is mandatory in these cases. Surgical decompression, usually via laminectomy, is recommended if there is a disc herniation. It is generally accepted that CES is a surgical emergency as early decompression prevents irreversible neurological disability [2, 4, 5]. However, the lack of accurate imaging and prompt surgical decompression may be difficult to achieve in low-resource settings.
In summary, the triad of delayed presentation by the patient; physician-related factors such as not suspecting CES or referral to inappropriate speciality; and problems of low-resource settings such as delay or unavailability of magnetic resonance imaging (MRI) and inability to perform surgery due to a lack of beds or theater time in a tertiary care center will contribute to make an already bad situation worse [2]. It is probable that all of these factors contributed to this patient’s outcome.
Conclusion
This is a case that demonstrates the tragic long-term sequelae of undiagnosed CES. It illustrates the importance of clinical suspicion and prompt referral to a neurosurgical unit to take timely action.
Availability of data and materials
Not applicable.
References
Anthony S. Cauda equina syndrome. Med Protect Soc UK Casebook. 2000;20:9–13.
Gardner A, Gardner E, Morley T. Cauda equina syndrome: a review of the current clinical and medico-legal position. Eur Spine J. 2011;20:690–7.
Ahn UM, Ahn NU, Buchowski JM, et al. Cauda equina syndrome secondary to lumbar disc herniation. A meta-analysis of surgical outcomes. Spine. 2000;25:1515–22.
Gleave JRW, Macfarlane R. Cauda equina syndrome: what is the relationship between timing of surgery and outcome? Br J Neurosurg. 2002;16(4):325–8.
Jalloh I, Minhas P. Delays in the treatment of cauda equina syndrome due to its variable clinical features in patients presenting to the emergency department. Emerg Med J. 2007;24(1):33–4. https://doi.org/10.1136/emj.2006.038182.
Malloch JD. Acute retention due to intervertebral disc prolapse. Br J Urol. 1965;37:578.
Acknowledgements
We would like to express our sincere gratitude to the staff of the obstetrics and gynecology ward, University hospital—Kotelawala Defence University, Werahera, Sri Lanka.
Funding
The authors declare that they have no funding source.
Author information
Authors and Affiliations
Contributions
CE and DW were the gynecologists, RW was the urologist, SP was the neurosurgeon, and DG was the physician involved in the management. DD was the junior doctor involved. CE and DD wrote the manuscript. CE, DW, RW, SP, and DG were involved in the editing of the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed written consent was obtained from the patient for publication of case details and accompanying images.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ekanayake, C.D., Weerasekera, D., Dissanayake, D. et al. Late presentation of a cauda equina lesion with a vulval abscess: a case report. J Med Case Reports 15, 455 (2021). https://doi.org/10.1186/s13256-021-03012-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-021-03012-z