Abstract
Background
Type 2 diabetes mellitus (T2DM) and hypothyroidism are two common endocrine diseases and the phenomenon that the prevalence of diabetes-related hypothyroidism shows a significant upward trend deserves further attention, but the specific pathogenesis is not yet clear. The study aimed to explore the molecular mechanisms on DNA methylation regulating gene expression and participating in diabetes-related hypothyroidism through genome-wide DNA methylation and RNA sequencing.
Results
The prevalence of hypothyroidism in T2DM patients was significantly higher than that in patients without T2DM (P = 0.018). Meanwhile, high TSH and low T3 and T4 levels were detected in diabetic mice. Low T3 and T4 levels were detected in Nthy-ori3-1 cells incubated in high-glucose medium. Differentially expressed genes (DEGs) and differentially methylated regions (DMRs) were detected by RNA sequencing and reduced representation bisulfite sequencing in Nthy-ori3-1 cells cultured in high-glucose and normal medium. Functional enrichment analyses reveled that DMRs and DEGs were related to significant pathways including Ras, Wnt and MAPK pathways.
Conclusions
We observed the potential connection between T2DM and hypothyroidism. This study was the first one carrying out DNA methylation and gene expression profiles to explore epigenetic modification in diabetes-related hypothyroidism, which provided information for the detailed study of the molecular mechanism in diabetes-related hypothyroidism.
Similar content being viewed by others
Background
The prevalence of diabetes mellitus is increasing worldwide. There were approximately 425 million adults living with diabetes mellitus worldwide in 2017 according to data from the International Diabetes Federation and the number is expected to reach 629 million by 2045 [1]. It is worth noting that diabetes mellitus has become a major public health problem in the general population of China. Approximately 11.6% of Chinese adults was estimated to have diabetes mellitus in 2010 [2]. Long-term hyperglycemia can lead to complications such as diabetic nephropathy, diabetic retinopathy, diabetic neuropathy, atherosclerosis, and adversely affect patients' health and quality of life [3,4,5].
Hypothyroidism is a common endocrine problem caused by the reduction of thyroid hormone synthesis and secretion or insufficient tissue utilization due to various reasons. A study of thyroid diseases in 10 cities of China completed in 2011 (n = 15,008) showed that the prevalence of hypothyroidism among people over 18 years old was 17.73% [6]. Hypothyroidism has been found be associated with atherosclerosis, myocardial infarction and heart failure, requiring life-long replacement therapy with thyroid hormones [7,8,9].
T2DM and hypothyroidism are two frequently occurring disorders involving the endocrine system and the relationship between them was first reported in 1979 [10]. Since then, many studies have observed the coexistence of diabetes mellitus and hypothyroidism. A study in Mexico compared 1848 patients with T2DM and 3313 non-diabetic patients, and the results showed that the odd ratio (OR) of the prevalence of hypothyroidism in T2DM patients was 3.45 (95% CI 2.5–4.7) [11]. A systematic review and meta-analysis reported by Han et al. compared 5768 T2DM patients with 6225 non-diabetic patients. It was found that subclinical hypothyroidism was more common in T2DM patients with an OR of 1.93 (95% CI 1.66–2.24) [12]. Meanwhile, hypothyroidism can lead to high blood pressure and hyperlipidemia, affect insulin secretion, damage microvascular and macrovascular function, thereby increasing the risk of diabetic complications and exacerbating the progression of diabetes [1]. Diabetic complications in patients with subclinical hypothyroidism were more common than them in people with normal thyroid function. The overall OR for diabetic nephropathy, diabetic retinopathy, peripheral arterial disease and diabetic peripheral neuropathy was 1.74 (95% CI 1.34–2.28), 1.42 (95% CI 1.21–1.67), 1.85 (95% CI 1.35–2.54) and 1.87 (95% CI 1.06–3.28), respectively [12]. Therefore, the specific molecular mechanism of diabetes-related hypothyroidism needs to be studied urgently.
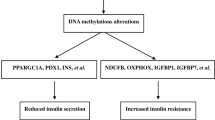
DNA methylation an epigenetic modification pattern in which methyl groups are added to the cytosine residues at the context of CpG dinucleotides, thereby changing the transcription activity of DNA fragments without changing the DNA sequence [13]. Environmental factors could regulate gene expression and function through epigenetic factors [14]. Epigenetic modification has opened up a new research field in the study of diabetes mellitus and thyroid diseases, but we still know little about how DNA methylation participates in the pathogenesis of diabetes-related hypothyroidism through regulating gene expression. Therefore, genome‑wide profiles of DNA methylation and gene expression were detected in the current study and we attempted to clarify the underlying mechanism of diabetes-related hypothyroidism with regard to epigenetics.
Results
Prevalence of thyroid dysfunction in patients with T2DM
A total of 1551 patients with T2DM and 374 healthy controls were included in the study. The prevalence of overt hypothyroidism, subclinical hypothyroidism, overt hyperthyroidism and subclinical hyperthyroidism were 1.74%, 3.93%, 0.19% and 1.93%, respectively (Table 1). The results showed that the prevalence of hypothyroidism in T2DM patients was significantly higher than that in patients without T2DM (P = 0.018). In contrast, the prevalence of hyperthyroidism in T2DM patients was lower than that in healthy controls (P < 0.001).
Thyroid dysfunction in diabetic mice
Blood was collected from high-fat-diet (HFD) -fed mice and ob/ob mice after anesthesia was administered. Serum T3, T4 and TSH concentrations were detected by ELISA. Serum TSH level was significantly higher in HFD-fed mice (Fig. 1a, P = 0.001) and ob/ob mice (Fig. 1d, P < 0.001). At the same time, concentration of T3 was markedly lower in HFD-fed mice (Fig. 1b, P < 0.001) and ob/ob mice (Fig. 1e, P < 0.001). Serum T4 level was lower in HFD-fed mice (Fig. 1c, P < 0.001) and ob/ob mice (Fig. 1f, P < 0.001), either.
Thyroid function in diabetic mice. High TSH (a), low T3 (b) and T4 (c) levels were detected in the serum of HFD-fed diabetic mice (n = 5 per group). High TSH (d), low T3 (e) and T4 (f) levels were detected in the serum of ob/ob mice (n = 5 per group). Data are presented as mean ± SD. **P < 0.01, ***P < 0.001
Thyroid hormone secretion in Nthy-ori3-1 cells incubated in high-glucose medium
Nthy-ori3-1 cells were incubated in high-glucose medium and normal medium for 48 h. ELISA kits were used for detecting concentrations of T3 and T4 after the culture supernatant of Nthy-ori3-1 cells were collected. T3 (Fig. 2a, P < 0.001 when glucose concentration was 20 mM and 30 mM) and T4 (Fig. 2b, P = 0.004 when glucose concentration was 20 mM and P = 0.001 when glucose concentration was 30 mM) levels was lower in high-glucose groups compared to the control group.
Differentially expressed genes (DEGs) in high-glucose-incubated Nthy-ori3-1 cells
Changes in gene expression profile were found by next-generation sequencing between Nthy-ori3-1 cells incubated in high-glucose medium and normal medium. According to the coding ability of transcripts, they were divided into mRNAs and lncRNAs. The most dysregulated genes were shown in Table 2. Volcano plots of mRNA and lncRNA were drawn, respectively. A total of 183 mRNAs and 216 lncRNAs were significantly upregulated, and 645 mRNAs and 338 lncRNAs were significantly downregulated (Fig. 3a, b).
Functional enrichment of DEGs. Differentially expressed mRNAs and lncRNAs were shown by volcano plots (a and b). The red and green dots represented statistically upregulated and downregulated genes. Functional enrichment of mRNAs (c and d) and lncRNAs (e and f) were conducted using GO and KEGG pathway analyses, respectively
Functional enrichment of DEGs
In order to better explore the function and molecular pathway of DEGs, functional enrichment was conducted using Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) analyses. Go analysis was carried out from three aspects: molecular function, biological process and cellular component. The significant GO clusters such as cell cycle, RNA binding, DNA replication origin binding for mRNAs (Fig. 3c) and cellular metabolic process, cellular protein metabolic process, protein binding for lncRNA-targeting genes (Fig. 3e) were found. Significant KEGG pathways related to ubiquitin-mediated proteolysis, jak-STAT signaling pathway and Ras signaling pathway were enriched for differentially expressed mRNAs (Fig. 3d). Enrichment pathways included RNA transport and cell cycle for lncRNA-targeting genes were also found (Fig. 3f).
Differentially methylated regions (DMRs) in high-glucose-incubated Nthy-ori3-1 cells
A total of 2662 DMRs were identified, including 1272 hypermethylated and 1390 hypomethylated DMRs. The significance and distribution of DMRs on the chromosome were shown in Fig. 4a. Hyper- and hypomethylated DMRs were colored in red and blue, respectively. Distribution of DMRs was shown in Fig. 4b.
DMRs in high-glucose-incubated Nthy-ori3-1 cells. The significance and distribution of DMRs on the chromosome were displayed in a circular plot (a). The distribution of DMRs based on gene regions were shown in histogram (b). Hyper- and hypomethylated regions were colored in red and blue, respectively
Functional enrichment of DMRs -related genes
GO analysis for DMRs-related genes was conducted to explore biological processes and problems. The significant GO clusters such as cell development, cell differentiation and transcription process were enriched (Fig. 5a). Genes coordinated with each other to perform their biological functions. Through significant enrichment of pathways, the most important biochemical pathways and signal transduction pathways involved in DMR-related genes could be determined. Significant KEGG pathways related to Wnt, Ras and MAPK signaling pathways were enriched (Fig. 5b).
Overlap analysis between DMRs and DEGs
To explore the relationship between DMRs and DEGs, an overlap analysis was conducted. We imported the list of DEGs into the protein–protein interaction database (STRING) in order to find out the relationship between these DEGs. And then we imported the result of the interaction of DEGs into Cytoscape software to realize the visualization of the interaction network. DEGs with DMRs were colored in orange, blue and yellow for hypermethylation, hypomethylation and both, respectively (Fig. 6). Data used for the interaction network was shown in Additional file 1: Table S1.
Quantitative real-time PCR (qRT-PCR) validation for DEGs
The most upregulated and downregulated mRNAs and lncRNAs were chosen for qRT-PCR validation. ENSG00000227359 and ENSG00000249141 were upregulated in Nthy-ori3-1 cells incubated in high-glucose medium (Fig. 7a and c, P < 0.001 and P = 0.005). ENSG00000240790 and ENSG00000284776 were downregulated in Nthy-ori3-1 cells incubated in high-glucose medium (Fig. 7b, d, P = 0.023 and P = 0.040).
Discussion
The coexistence of T2DM and hypothyroidism is not accidental. Zhu et al.'s cross-sectional study on the prevalence of abnormal thyroid function in elderly T2DM patients in China suggested that hypothyroidism was the most common type of thyroid dysfunction in T2DM patients, accounting for 14.19%. The prevalence of overt and subclinical hypothyroidism was 9.3% and 4.89%, respectively [15]. Diabetes-related hypothyroidism from three perspectives were observed: patients, experimental mice, and cells. We analyzed the clinical data of 1551 T2DM patients and found that hypothyroidism was also the most common type of thyroid dysfunction, accounting for 5.67% of T2DM patients, of which overt and subclinical hypothyroidism were 3.93% and 1.74%, respectively. In addition, high TSH and low T3 and T4 levels were detected in diabetic mice. Low T3 and T4 levels were detected in Nthy-ori3-1 cells incubated in high-glucose medium.
T2DM and hypothyroidism have similar clinical symptoms, such as fatigue, edema, paleness, and weight gain [1, 16,17,18]. Therefore, the symptoms of T2DM can mask the occurrence of hypothyroidism. At the same time, some anti-diabetic drugs such as sulfonylureas and thiazolidinediones may also affect thyroid function [1]. Thus, T2DM patients are likely to ignore their signs and symptoms about hypothyroidism. Hypothyroidism without proper intervention and treatment may increase the risk of diabetic complications and aggravate the course of T2DM [19, 20]. It is of great significance to explore the specific mechanism of diabetic-related hypothyroidism for deepening our understanding of the disease and optimizing the treatment plan.
DNA methylation is one of the most widely studied epigenetic mechanisms regulating gene expression and mediated by DNA methyltransferases (DNMTs), among which DNMT1 mediates hemi-methylation and DNMT3A and DNMT3B were responsible for de novo methylation [21]. DNA methylation in CpG-rich promoter regions is linked to gene repression and DNA methylation within gene bodies is associated with gene activation [22]. In a study of diabetic peripheral neuropathy (DPN), the authors found that DNA methylation and gene expression profile of sural nerves in DPN patients with high HbA1c had significant changes, suggesting that the interaction between DNA methylation and gene expression participated in the pathological mechanism in DPN [23]. In this study, RNA sequencing and reduced representation bisulfite sequencing (RRBS) were performed in Nthy-ori3-1 cells cultured in high-glucose medium and normal medium, respectively. Sequencing results revealed changes in genome-wide DNA methylation and gene expression profiles. The qRT-PCR validation of specific genes confirmed the accuracy and reliability of the sequencing results.
Researchers believed that diabetes mellitus could affect thyroid function by altering TRH and TSH levels [1, 24]. Hyperglycemia led to a decrease in the activity of thyroxine 5′ deiodinase and affected the conversion of T4 to T3, which was also one of the reasons for altering thyroid function [25, 26]. Molnar et al. reported that some inflammatory cytokines including TNF-α, IFN-γ and IL-6 were related with low level of T3, which showed that high levels of inflammatory cytokines in diabetic patients might accelerate hypothyroidism [27]. Wnt signaling pathway was found under control of DNA methylation in our study and was reported to be linked to inflammation, which suggested that DNA methylation of specific genes of Wnt signaling pathway might participated in diabetes-related hypothyroidism [28, 29]. Chen et al. confirmed that high concentration of glucose inhibited proliferation of Nthy-ori3-1 cells and arrested more thyroid cells in G0/G phase [30]. This finding suggested that the reduction of thyroid cells might be partly responsible for low thyroid hormone levels. Ras-Raf-MEK-MAPK signaling pathway was reported to be involved in numerous cellular and physiological processes essential to life including cell proliferation and cell growth [31]. The KEGG analysis of DMRs revealed that Ras and MAPK signaling pathways were dysregulated in high-glucose-cultured Nthy-ori3-1 cells. DNA methylation of these signaling pathways related to cell proliferation might be a new mechanism connecting diabetes mellitus and hypothyroidism.
Conclusions
We observed the potential connection between diabetes mellitus and hypothyroidism. This study was the first one carrying out DNA methylation and gene expression profiles to explore epigenetic modification in diabetes-related hypothyroidism, which provided information for the detailed study of the regulation of DNA methylation in diabetes-related hypothyroidism.
Methods
Patients
A total of 1551 T2DM patients hospitalized in our medical center were enrolled from 1 January 2018 to 31 December 2019. 374 age-matched patents without suffering from T2DM were included in the control group. All participants were older than 18 years old and complete clinical data were available. Pregnant women and participants with a history of malignant tumor or thyroid surgery were excluded in the study. The diagnostic criteria for T2DM referred to Guidelines for the prevention and control of type 2 diabetes in China (2020 Edition) [32]. The reference intervals were 0.35–5.5 IU/mL for TSH, 2.3–4.2 pg/mL for FT3 and 0.89–1.76 ng/dL for FT4 according to the commercial kit used in our medical center. The diagnostic criteria for thyroid dysfunction were as follows: overt hypothyroidism, TSH > 5.5 IU/mL, FT3 < 2.3 pg/mL and FT4 < 0.89 ng/dL; subclinical hypothyroidism, TSH > 5.5 IU/mL with normal FT3 and FT4 values; overt hyperthyroidism, TSH < 0.35 IU/mL, FT3 > 4.2 pg/mL and FT4 > 1.76 ng/dL; overt hyperthyroidism, TSH < 0.35 IU/mL with normal FT3 and FT4 values. The study was approved by the ethics committee of Beijing Hospital (No. 2021BJYYEC-013-01).
Animals
Eight-week-old male ob/ob mice on the C57BL/6J background were purchased form the Institute of Laboratory Animals Science, CAMS & PUMC. Five-week-old male C57BL/6J mice were obtained from the Institute of Laboratory Animals Science, CAMS & PUMC and were randomly divided into two groups. One group of C57BL/6J mice were fed with a high-fat diet for 8 weeks (D12494, 60% energy from fat). The control group of C57BL/6J mice were fed with a normal diet for 8 weeks (D12450J, 10% energy from fat). Blood was collected via the orbital vein and serum was separated after coagulation for 1 h and centrifugation. All experimental procedures were approved by the experimental animal management committee of Beijing Hospital (No. P2017108).
Cell culture
The Nthy-ori3-1 cell line were purchased from the Stem Cell Bank/Stem Cell Core Facility and were grown in RPMI-1640 medium (Hyclone, USA) with 10% fetal bovine serum (Biological Industries, Israel) at 37 °C and 5% CO2. High-glucose microenvironment were induced via incubating Nthy-ori3-1 cells with 20 or 30 mM high-glucose medium.
Enzyme-linked immunosorbent assay (ELISA)
Concentrations of T3, T4 and TSH in the culture supernatant of Nthy-ori3-1 cells and mice serum were detected using ELISA kits (Cloud-Clone Corp, China). In brief, 50 μL samples were added to each well and then 50 μL prepared detection reagent A was added immediately. After incubating for 1 h at 37 °C, the plate was discarded and washed for 3 times. 100 μL prepared detection reagent B was added and the plate was incubated for 30 min at 37 °C. After washing for total 5 times, the substrate solution was added and the samples were incubated at 37 °C until color change was observed. The stop solution was added to each well and the OD values at 450 nm were measured using a microplate reader (Synergy H1, USA).
RNA sequencing and genome-wide methylation profiling
Total RNA and DNA were extracted from Nthy-ori3-1 cells grown in high-glucose medium (glucose: 30 mM) and normal medium (glucose: 5 mM). The purity of RNA and DNA were evaluated by the NanoPhotometer® spectrophotometer (IMPLEN, USA). RNA and DNA concentrations were measured using Qubit® DNA Assay Kit in Qubit® 2.0 Flurometer (Life Technologies, USA). The quality of RNA and DNA was assessed on the Agilent Bioanalyzer 2100 system (Agilent Technologies, USA). RNA sequencing was performed on an Illumina Hiseq 2500 platform and 125 bp paired-end reads were generated. For RRBS, the library was constructed and pair-end sequencing of sample was performed on the Illumina platform.
Quality control and data mapping
Raw data of fastq format was firstly filtered to obtain the clean data with high quality for the following analyses. For RNA sequencing data, reference genome and gene model annotation files were downloaded from genome website directly. Index of the reference genome was built and paired-end clean reads were aligned to the reference genome using HISAT2 v2.0.4. For RRBS data, bisulfite-treated reads were aligned to a reference genome using Bismark software [33]. Clean reads and reference genome were transformed into bisulfite-converted version (C-to-T and G-to-A converted). Then, the sequence reads were compared to the normal genomic sequence and the methylation state of all cytosine positions was inferred.
Differential expression and methylation analyses
Differential expression analysis was performed using edgeR software and genes with a P adjust < 0.05 were assigned as differentially expressed [34]. DMRs were identified using the DSS software [35]. According to the distribution of DMRs through the genome, we defined the genes related to DMRs as genes whose gene body regions (from transcription starting site to transcription ending site) or promoter regions (2 kb upstream from the transcription starting site) have an overlap with the DMRs.
GO and KEGG enrichment analyses
GO enrichment analyses of differentially expressed genes, lncRNA target genes and genes related to DMRs were implemented by the GOseq R package, in which gene length bias was corrected [36]. GO terms with corrected P value less than 0.05 were considered as significant enrichment. KOBAS software was used to test the statistical enrichment of differentially expressed genes, lncRNA target genes and genes related to DMRs in KEGG pathways [37].
Quantitative real-time PCR
cDNA of extracted total RNA was synthesized by reverse transcription using PrimeScript™ RT Master Mix kit (Takara, Japan). Then, TB Green® Premix Ex Taq™ II kit (Takara, Japan) was used for cDNA amplification on the Bio-Rad iQ5 real-time PCR system (Bio-Rad, USA). Specific primers used were listed as follows: ENSG00000227359, 5′-TCTTCTCAGGGCCGTAAACC-3′ (forward) and 5′-GCACACTGCCAGGAATAAAGC-3′ (reverse); ENSG00000240790, 5′-AGGAAAGGACACGTCAGCATC-3′ (forward) and 5′-GAAGGACGTCATGGGCGAG-3′ (reverse); ENSG00000249141, 5′-GGCAGAAGCCTGGAACTCTAC-3′ (forward) and 5′-CTTCTGCAGTGTCTTCTGTGG-3′ (reverse); ENSG00000284776, 5′-ATCGAAATGAGTTCACGGCCT-3′ (forward) and 5′-TGTTCCAGTTCCTTCTGCGT-3′ (reverse); GAPDH, 5′-GCACCGTCAAGGCTGAGAAC-3′ (forward) and 5′-TGGTGAAGACGCCAGTGGA-3′ (reverse). Each sample was tested in triplicate. GAPDH served as the reference gene and the relative expression of target genes were calculated using the 2−ΔΔCT method.
Statistical analysis
SPSS 25.0 software was used for statistical analyses. Kolmogorov–Smirnov test was used for verifying normal distribution. Non-normally distributed variables were compared using non-parametric Mann–Whitney test. Student’s t test was conducted for comparison between normally distributed variables. All experiments were performed three times and P < 0.05 was considered to be statistically significant.
Availability of data and materials
The datasets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
- T2DM:
-
type 2 diabetes mellitus
- OR:
-
odd ratio
- HFD:
-
high fat diet
- DEG:
-
differentially expressed gene
- DMR:
-
differentially methylated region
- qRT-PCR:
-
quantitative real-time PCR
- DNMT:
-
DNA methyltransferase
- RRBS:
-
reduced representation bisulfite sequencing;
- ELISA:
-
enzyme-linked immunosorbent assay
References
Kalra S, Aggarwal S, Khandelwal D. Thyroid dysfunction and type 2 diabetes mellitus: screening strategies and implications for management. Diabetes Ther Res Treat Educ Diabetes Relat Disord. 2019;10(6):2035–44.
Xu Y, Wang L, He J, Bi Y, Li M, Wang T, et al. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310(9):948–59.
Wang Y, He W. Improving the dysregulation of FoxO1 activity is a potential therapy for alleviating diabetic kidney disease. Front Pharmacol. 2021;12:630617.
Silva M, Peng T, Zhao X, Li S, Farhan M, Zheng W. Recent trends in drug-delivery systems for the treatment of diabetic retinopathy and associated fibrosis. Adv Drug Deliv Rev. 2021;173:439–60.
Natarajan R. Epigenetic mechanisms in diabetic vascular complications and metabolic memory: the 2020 Edwin Bierman award lecture. Diabetes. 2021;70(2):328–37.
Shan Z, Chen L, Lian X, Liu C, Shi B, Shi L, et al. Iodine status and prevalence of thyroid disorders after introduction of mandatory universal salt iodization for 16 years in China: a cross-sectional study in 10 cities. Thyroid Off J Am Thyroid Assoc. 2016;26(8):1125–30.
Özcan EE, Dural M, Görenek B. Tips for management of arrhythmias in endocrine disorders from an European Heart Rhythm Association position paper. Anatol J Cardiol. 2018;20(4):241–5.
Abdel-Moneim A, Gaber AM, Gouda S, Osama A, Othman SI, Allam G. Relationship of thyroid dysfunction with cardiovascular diseases: updated review on heart failure progression. Hormones (Athens). 2020;19(3):301–9.
Hak AE, Pols HA, Visser TJ, Drexhage HA, Hofman A, Witteman JC. Subclinical hypothyroidism is an independent risk factor for atherosclerosis and myocardial infarction in elderly women: the Rotterdam Study. Ann Intern Med. 2000;132(4):270–8.
Feely J, Isles TE. Screening for thyroid dysfunction in diabetics. Br Med J. 1979;1(6179):1678.
Tamez-Pérez HE, Martínez E, Quintanilla-Flores DL, Tamez-Peña AL, Gutiérrez-Hermosillo H, Díaz de León-González E. The rate of primary hypothyroidism in diabetic patients is greater than in the non-diabetic population. An observational study. Med Clin. 2012;138(11):475–7.
Han C, He X, Xia X, Li Y, Shi X, Shan Z, et al. Subclinical hypothyroidism and type 2 diabetes: a systematic review and meta-analysis. PLoS ONE. 2015;10(8):e0135233.
Wang WR, Chen NT, Hsu NY, Kuo IY, Chang HW, Wang JY, et al. Associations among phthalate exposure, DNA methylation of TSLP, and childhood allergy. Clin Epigenet. 2021;13(1):76.
Guo Q, Wu D, Fan C, Peng S, Guan H, Shan Z, et al. Iodine excess did not affect the global DNA methylation status and DNA methyltransferase expression in T and B lymphocytes from NOD.H-2(h4) and Kunming mice. Int Immunopharmacol. 2018;55:151–7.
Zhu Y, Xu F, Shen J, Liu Y, Bi C, Liu J, et al. Prevalence of thyroid dysfunction in older Chinese patients with type 2 diabetes-a multicenter cross-sectional observational study across China. PLoS ONE. 2019;14(5):e0216151.
Stuber MJ, Moutzouri E, Feller M, Del Giovane C, Bauer DC, Blum MR, et al. Effect of thyroid hormone therapy on fatigability in older adults with subclinical hypothyroidism: a nested study within a randomized placebo-controlled trial. J Gerontol Ser A Biol Sci Med Sci. 2020;75(9):e89–94.
Talebi S, Karimifar M, Heidari Z, Mohammadi H, Asbaghi O, Hadi A, et al. The effect of synbiotic supplementation on anthropometric indices, appetite, and constipation in people with hypothyroidism: a randomized, double-blind, placebo-controlled trial. Phytother Res PTR. 2020;34(10):2712–20.
Berk KA, Buijks HIM, Verhoeven AJM, Mulder MT, Özcan B, van’t Spijker A, et al. Group cognitive behavioural therapy and weight regain after diet in type 2 diabetes: results from the randomised controlled POWER trial. Diabetologia. 2018;61(4):790–9.
Wang J, Li H, Tan M, Gao G, Zhang Y, Ding B, et al. Association between thyroid function and diabetic nephropathy in euthyroid subjects with type 2 diabetes mellitus: a cross-sectional study in China. Oncotarget. 2019;10(2):88–97.
Wu J, Yue S, Geng J, Liu L, Teng W, Liu L, et al. Relationship between diabetic retinopathy and subclinical hypothyroidism: a meta-analysis. Sci Rep. 2015;5:12212.
Czarny P, Białek K, Ziółkowska S, Strycharz J, Barszczewska G, Sliwinski T. The importance of epigenetics in diagnostics and treatment of major depressive disorder. J Personal Med. 2021;11(3):167.
Arechederra M, Recalde M, Gárate-Rascón M, Fernández-Barrena MG, Ávila MA, Berasain C. Epigenetic biomarkers for the diagnosis and treatment of liver disease. Cancers. 2021;13(6):1265.
Guo K, Eid SA, Elzinga SE, Pacut C, Feldman EL, Hur J. Genome-wide profiling of DNA methylation and gene expression identifies candidate genes for human diabetic neuropathy. Clin Epigenet. 2020;12(1):123.
Rondeel JM, de Greef WJ, Heide R, Visser TJ. Hypothalamo-hypophysial-thyroid axis in streptozotocin-induced diabetes. Endocrinology. 1992;130(1):216–20.
Ogbonna SU, Ezeani IU. Risk factors of thyroid dysfunction in patients with type 2 diabetes mellitus. Front Endocrinol. 2019;10:440.
Huang X, Zhang X, Zhou X, Han X, Fu Z, Li Y, et al. Prevalence of thyroid dysfunction in a chinese population with different glucose intolerance status: a community-based cross-sectional study. Diabetes Metab Syndr Obes Targets Ther. 2020;13:4361–8.
Molnár I, Balázs C, Szegedi G, Sipka S. Inhibition of type 2,5’-deiodinase by tumor necrosis factor alpha, interleukin-6 and interferon gamma in human thyroid tissue. Immunol Lett. 2002;80(1):3–7.
Jridi I, Canté-Barrett K, Pike-Overzet K, Staal FJT. Inflammation and Wnt signaling: target for immunomodulatory therapy? Front Cell Dev Biol. 2020;8:615131.
Weinstock A, Rahman K, Yaacov O, Nishi H, Menon P, Nikain CA, et al. Wnt signaling enhances macrophage responses to IL-4 and promotes resolution of atherosclerosis. Elife. 2021;10:e67932.
Chen XJ, Gong XH, Jie JP, Yu WH, Chen X, Du X, et al. Receptor for advanced glycation end products reveals a mechanism regulating thyroid hormone secretion through the SIRT1/Nrf2 pathway. J Cell Biochem. 2019;120(3):4582–98.
Jiang T, Xia Y, Lv J, Li B, Li Y, Wang S, et al. A novel protein encoded by circMAPK1 inhibits progression of gastric cancer by suppressing activation of MAPK signaling. Mol Cancer. 2021;20(1):66.
Chinese Diabetes Society. Guidelines for the prevention and treatment of type 2 diabetes in China (2020 Edition). Chin J Endocrinol Metab. 2021;37(4):311–98.
Krueger F, Andrews SR. Bismark: a flexible aligner and methylation caller for bisulfite-seq applications. Bioinformatics (Oxford, England). 2011;27(11):1571–2.
Robinson MD, McCarthy DJ, Smyth GK. edgeR: a Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics (Oxford, England). 2010;26(1):139–40.
Feng H, Conneely KN, Wu H. A Bayesian hierarchical model to detect differentially methylated loci from single nucleotide resolution sequencing data. Nucl Acids Res. 2014;42(8):e69.
Young MD, Wakefield MJ, Smyth GK, Oshlack A. Gene ontology analysis for RNA-seq: accounting for selection bias. Genome Biol. 2010;11(2):R14.
Kanehisa M, Araki M, Goto S, Hattori M, Hirakawa M, Itoh M, et al. KEGG for linking genomes to life and the environment. Nucl Acids Res. 2008;36(Database issue):D480–4.
Acknowledgements
We are grateful to all authors for their careful work and good cooperation.
Funding
The study was funded by Natural Science Foundation of China (Grant Nos. 81670763 and 81471050).
Author information
Authors and Affiliations
Contributions
LG, LY and JL conceived and designed the research. JL was responsible for performing the experiments. JL and XW were responsible for data analyses and writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethics committee of Beijing Hospital.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Overlap network between DEGs and DMRs.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Luo, J., Wang, X., Yuan, L. et al. Genome‑wide profiling of DNA methylation and gene expression unravel the epigenetic landscape in diabetes-related hypothyroidism. Clin Epigenet 13, 123 (2021). https://doi.org/10.1186/s13148-021-01109-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13148-021-01109-2