Abstract
Background
Painful diabetic neuropathy (PDN), a debilitating and progressive chronic pain condition that significantly impacts quality of life, is one of the common complications seen with long-standing diabetes mellitus. Neither pharmacological treatments nor low-frequency spinal cord stimulation (SCS) has provided significant and long-term pain relief for patients with PDN. This study aims to document the value of 10-kHz SCS in addition to conventional medical management (CMM) compared with CMM alone in patients with refractory PDN.
Methods
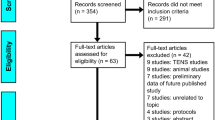
In a prospective, multicenter, randomized controlled trial (SENZA-PDN), 216 subjects with PDN will be assigned 1:1 to receive 10-kHz SCS combined with CMM or CMM alone after appropriate institutional review board approvals and followed for 24 months. Key inclusion criteria include (1) symptoms of PDN for at least 12 months, (2) average pain intensity of at least 5 cm—on a 0- to 10-cm visual analog scale (VAS)—in the lower limbs, and (3) an appropriate candidate for SCS. Key exclusion criteria include (1) large or gangrenous ulcers or (2) average pain intensity of at least 3 cm on VAS in the upper limbs or both. Along with pain VAS, neurological assessments, health-related quality of life, sleep quality, and patient satisfaction will be captured. The primary endpoint comparing responder rates (≥50% pain relief) and safety rates between the treatment groups will be assessed at 3 months. Several secondary endpoints will also be reported on.
Discussion
Enrollment commenced in 2017 and was completed in 2019. This study will help to determine whether 10-kHz SCS improves clinical outcomes and health-related quality of life and is a cost-effective treatment for PDN that is refractory to CMM.
Trial registration
ClincalTrials.gov identifier: NCT03228420 (registered 24 July 2017).
Similar content being viewed by others
Background
Globally, 422 million people have diabetes, resulting in USD $1.7 trillion in direct and indirect costs [1]. According to data from the Centers for Disease Control and Prevention, 29 million people in the US are currently living with diabetes and another 86 million with prediabetes, resulting in $245 billion in health-care costs and lost productivity [2]. About 20% of patients with diabetes will develop painful diabetic neuropathy (PDN) [3], a debilitating and progressive chronic pain condition that significantly impacts quality of life.
Peripheral neuropathy from damage to peripheral nerves may result in pain, numbness, or weakness (or a combination of these) in the affected limb. Damage may affect small (myelinated Aδ and unmyelinated C) fibers along with injury to large myelinated fibers. One of the classifications for peripheral neuropathy is based on whether the damage is to a single nerve (mononeuropathy) or multiple nerves (polyneuropathy). The causes of polyneuropathy may include metabolic (e.g., chronic renal failure), endocrine disorders (e.g., PDN), treatment-induced toxicity (e.g., radiation, chemotherapy, or alcohol-induced neuropathy), infection (Lyme disease and post-herpetic neuralgia caused by herpes zoster virus), autoimmune disorders (Guillain–Barré syndrome and Charcot–Marie–Tooth neuropathy), compression (carpal tunnel syndrome, tarsal tunnel syndrome, ulnar neuropathy, and peroneal neuropathy), and trauma (trauma-induced neuropathy). Nearly half of cases of peripheral neuropathy are diagnosed as idiopathic [4].
The American Chronic Pain Association estimates that more than 15 million people in the US and Europe have some degree of neuropathic pain. More than 2 in 100 persons are estimated to have peripheral neuropathy; the incidence rises to 8 in 100 for those who are 55 or older [5]. In Europe, the prevalence of PDN ranged from 5.8% to 34.0% [6]. The incidences of PDN were reported to be 0.72 per 1000 persons per year in the Netherlands [7] and 0.64–0.69 per 1000 persons per year in the UK [8]. PDN is very taxing to the individual patient because of pain, impaired quality of life, and increased disability [9, 10] and to society as a whole because of the significant impact on the workforce and the increased cost of health care [11, 12]
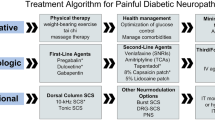
Anticonvulsant medications, including gabapentin and pregabalin, are among the most commonly prescribed medications for neuropathic pain due to PDN [13]. Pregabalin, or (S)-3-(aminomethyl)-5-methylhexanoic acid, is an analog of the inhibitory neurotransmitter gamma-aminobutyric acid (GABA). It is a compound that acts on the central nervous system, producing analgesic, anticonvulsant, and anxiolytic effects. Clinical studies have demonstrated the effectiveness of this drug in treating intractable limb pain from PDN resulting from both type 1 and 2 diabetes (Table 1) [14,15,16,17,18, 34]. A review of seven randomized controlled trials (RCTs) comparing pregabalin with placebo showed marginal benefits over placebo in decreasing average pain scores: 1.47 cm (placebo), 1.98 cm (150 mg pregabalin), 2.44 cm (300 mg pregabalin), and 2.75 cm (600 mg pregabalin) [35]. The mean follow-up was 4 to 12 weeks. Responder rates, representing the percentage of subjects with at least 50% improvement from baseline, varied from 40% to 49%, and placebo responder rates ranged from 14.5% to 23.0%. Adverse events (AEs) reported include dizziness, peripheral edema, somnolence, infection, and weight gain. Approximately 77% of patients prescribed pregabalin for PDN will discontinue the treatment within 1 year because of intolerable side effects or lack of efficacy [13]. In addition, the Neuropathic Pain Special Interest Group (NeuPSIG) of the International Association for the Study of Pain, which recently conducted a meta-analysis of 25 RCTs with pregabalin treatment of neuropathic pain, calculated that the number needed to treat (NNT) to achieve 50% pain reduction was 7.7 (range of 3.3–45.3); however, the safety profile for this medication is poor as the number needed to harm (NNH) is 13.9 [36]. Another commonly used class of medication for neuropathic pain, including PDN, consists of the serotonin-noradrenaline reuptake inhibitors (SNRIs). In an analysis of 10 RCTs for SNRIs, including seven duloxetine studies, the NeuPSIG reported a combined NNT of 6.4 (range of 4.2–30.2) and NNH of 11.8.
Low-frequency, paresthesia-based spinal cord stimulation (SCS) has also been shown to be effective in treating intractable pain associated with many peripheral neuropathies, including RCTs on PDN (Table 1) [32, 33, 37,38,39,40,41,42]. In a single-center, observational study, Pluijms et al. [39] reported that the median pain score of subjects treated with SCS decreased from 6 cm at baseline to 1.8 cm at 3 months on the visual analog scale (VAS) (range of 0–10 cm). However, at 12 months, the median pain score increased to 2.9 cm, and slightly over half the subjects (8/15 or 53%) were still responding to the therapy with at least 50% improvement in pain. In another study comparing SCS with best medical treatment, pain scores measured with the numerical rating scale (NRS) (range of 0–10) decreased from 7.3 and 6.7 (day and night, respectively) at baseline to 4 and 3.5 at 24 months [33]. Responder rates (subjects with at least 50% pain reduction) ranged from 47% (8/17, day) to 35% (6/17, night). Changes in pain scores in these studies were deemed to be both clinically and statistically significant.
Unlike traditional low-frequency, paresthesia-based SCS that seeks to induce paresthesias in the affected pain distribution, 10-kHz SCS therapy delivers paresthesia-independent, high-frequency stimulation by use of a unique waveform and uniform pulse width [43]. The therapy has demonstrated safety and superior effectiveness for the treatment of back and leg pain [44,45,46,47,48,49] and improved health-related quality of life [50]; 10-kHz SCS therapy has also been studied for the treatment of neuropathic limb pain, upper limb and neck pain, and pelvic pain ([51,52,53,54] Burgher A, Kosek P, Surrett S, Rosen S, Bromberg T, Gulve A, Kansal A, Wu P, McRoberts WP, Udeshi A, et al, 10 kHz SCS for treatment of chronic pain of the upper extremities: A post-market observational study, submitted). In a prospective multicenter study treating chronic intractable pain of the limbs from peripheral polyneuropathy using 10-kHz SCS therapy, subjects reported a decrease in mean pain score from 7.9 cm (± 0.3 standard error of the mean [SEM]) at baseline (N = 26) to 2.4 cm (± 0.5 SEM) at 6 months post-implant (N = 18), and 78% of subjects were deemed responders [55].
The current treatments for neuropathic pain secondary to PDN are suboptimal and there are substantial unmet needs [56]. In the proposed study, 10-kHz SCS therapy plus conventional medical management (CMM) will be compared with CMM alone for safety, clinical effectiveness, and cost-effectiveness in treating subjects diagnosed with chronic, neuropathic limb pain resulting from diabetic neuropathy. Subjects are allowed to cross to the alternative treatment arm after 6 months if they meet specific criteria. This protocol represents a pragmatic study designed to address current evidence gaps and meet treatment guidelines for the American Diabetes Association and the American Academy of Neurology.
Methods/design
This is a multicenter, prospective, randomized controlled clinical study to document the comparative safety, clinical effectiveness, and cost-effectiveness of the addition of 10-kHz SCS therapy to CMM compared with CMM alone in subjects with chronic, intractable, neuropathic lower limb pain due to diabetic neuropathy. Enrollment of subjects will occur at multiple clinical sites only after institutional review board (IRB) approval and written informed consent from subjects have been obtained. Central ethical approval was provided by Western IRB (approval #1176998 received July 20, 2017), and local IRB approvals were obtained prior to recruiting at the corresponding sites. Subjects will be selected to participate in the study on the basis of the protocol’s inclusion (Table 2) and exclusion (Table 3) criteria. A panel of physician medical monitors independent of both the study sponsor and clinical investigator teams will review each consented subject to provide oversight of appropriate patient selection prior to randomization. Investigators will conduct the study in accordance with Good Clinical Practices as outlined in the US Code of Federal Regulations, the Declaration of Helsinki (version 2013), and other applicable regulatory requirements.
Randomization
Subjects meeting the requirements for inclusion and exclusion criteria will be randomly assigned 1:1 to 10-kHz SCS therapy delivered by a Senza SCS System (Nevro Corp., Redwood City, CA, USA) plus CMM or to CMM alone. The randomization for each site will be performed by a block randomization method developed by an independent statistician. Randomization will be stratified by average baseline pain VAS score and the baseline hemoglobin A1c (HbA1c) level. Thus, there will be four strata per site. Concealed allocation will be achieved via computer assignment of the treatment arm, and investigational site staff and study sponsor personnel will be unaware of the block size and randomization list. Owing to the nature of the treatments, specifically an implanted medical device compared with CMM, blinding subjects or investigator teams to the treatment assignment is not feasible. Subjects randomly assigned to either treatment group will have the potential to cross over to the alternative treatment arm at the 6-month visit if they meet all of the following criteria: (1) less than 50% lower limb pain relief from baseline, (2) documented subject dissatisfaction with the treatment (“dissatisfied” or “very dissatisfied” on subject satisfaction measure), and (3) investigator agreement with crossover.
Sample size
Up to 432 subjects will be screened at multiple clinical sites in the US to obtain a total of 216 randomly assigned subjects, resulting in approximately 108 subjects assigned to each treatment group. Subjects will continue with their respective treatments through the 3-month primary endpoint with an expected 10% attrition rate, resulting in approximately 97 subjects in each group at the primary endpoint. This is the sample size required on the basis of the following assumptions: a 60% responder rate for the 10-kHz SCS therapy group (80% trial success rate and 75% responders at 3 months among permanent implant subjects), a 36% responder rate for the CMM-only group, 90% power, and two-sided type I error of 0.05. Interim analysis will be performed to reassess sample size assumptions when 25% of the subjects reach the 3-month primary endpoint.
Outcomes assessed
Outcome data will be collected at baseline, trial and implant (10-kHz SCS therapy group), and defined follow-up intervals (Fig. 1, Table 4). Data collection will include measures of pain, health-related quality of life, function, subject satisfaction, health-care utilization, and medication usage, including treatments for pain relief and diabetic management (Table 5). Data will be collected by using electronic case report forms (eCRFs) via an Electronic Data Capture (EDC) system (M-Core, Medrio Inc., San Francisco, CA, USA). Data will be collected by the site research staff and entered directly into eCRFs in the EDC system at the investigational sites. The clinical site will record data on outcome variables as well as AEs should they occur. Subject confidentiality will be maintained, and each subject will be identified by his or her subject number.
Statistical analysis
The primary endpoint of this study is a composite of safety and effectiveness at 3 months, specifically the percentage of subjects who respond to treatment without a clinically meaningful neurological deficit compared with baseline. A responder is defined as a subject with at least 50% reduction in lower limb pain from baseline. For each subject and all analyses, the right and left lower limb VAS scores collected during a single visit will be averaged together to generate a lower limb pain score. In addition to the primary endpoint, several secondary and tertiary endpoints will be evaluated (Tables 6 and 7).
Descriptive statistics will be used to summarize all subject baseline and outcome data collected during the study. Continuous variables will be summarized by using means, standard deviations, medians, and ranges. Categorical variables will be summarized in frequency distributions. Statistical tests appropriate to the endpoint being examined will be used and identified. Parametric tests (e.g., Student’s t tests) will be used if the distributional properties of the data are suitable. If parametric tests are not indicated, the associated non-parametric tests (e.g., Mann–Whitney tests and Fisher’s exact tests) will be used. A two-sided P value of 0.05 or less for the primary endpoint will be considered evidence of statistical significance. Reported P values for all other tests will be considered nominal and unadjusted for multiple testing but without conclusions regarding statistical significance levels.
Analysis populations defined for the study include intention-to-treat (ITT) and per protocol (PP). The ITT population includes all subjects randomly assigned to the CMM and CMM plus 10-kHz SCS study groups. This is considered the safety population for purposes of reporting on any reported AEs. The PP population includes all ITT subjects who complete the 3-month primary assessment. The primary analysis population for the primary study endpoint is the ITT population. Secondary analyses will be performed in the PP population. The responder rates will be compared between groups with a Fisher’s exact test. Hierarchical testing will be carried out on the secondary endpoints listed in Table 6. Additional analyses will be performed for subjects who cross over to 10-kHz SCS treatment by using their data collected during the initial 6 months of CMM treatment as a control. Health economic outcomes will be assessed from health-care utilization, medication, work status, and health-related quality of life data.
Safety
A clinical events committee (CEC) will be convened to provide oversight during the study. This expert panel will serve in an advisory role to review safety data at interim points during the study, including the review of AEs and adjudication of the relatedness and seriousness of serious AEs. If needed, the CEC will also review unanticipated serious adverse device events on an urgent basis. The CEC will consist of clinicians with expertise in pain management, neurology, and endocrinology. Data review meetings will be held at regular intervals with the option for an ad hoc meeting at any time if an imminent subject safety issue arises. The CEC will have one physician member representing the study sponsor and the other physician members will be independent of the study sponsor and clinical investigators.
Discussion
In the treatment of neuropathic pain secondary to PDN, 10-kHz SCS has the potential to deliver safe and effective pain relief that is non-pharmacologic and paresthesia-independent. This would be an important development in the field because currently available treatment options for this condition, including pharmacologic agents and conventional SCS, are not adequate for all patients [56].
Pharmacologic options for treating neuropathic pain include anticonvulsants such as pregabalin, which has shown clinical efficacy in treating neuropathic pain due to PDN in high-quality studies [14,15,16,17,18, 34]. These trials were placebo-controlled and had large sample sizes but only short-term follow-up (lasting from 4 to 13 weeks). A study that pooled data from seven pregabalin trials to improve statistical power found that pain reductions were modest, the average NRS reduction was 2.75 for pregabalin (600 mg/day), and a majority of patients (53%) did not respond to the drug, defined as pain relief of at least 50% [35]. Duloxetine has also demonstrated pain relief for PDN in several well-designed RCTs. With follow-up lasting 8 to 16 weeks, reported responder rates ranged from 28% to 59% [19, 21, 23,24,25,26,27,28].
Conventional, low-frequency SCS has also been tested for treating neuropathic pain in patients with PDN. Median patient-reported NRS scores were reduced by an average of 3.1 after 12 months in a small study of 15 patients [39] and 3.3 after 24 months of stimulation in a study of 22 patients [33]. Although the long-term durability of these results is promising, the magnitude of pain relief was modest, similar to that offered by medication, and about half of the subjects did not respond to SCS treatment in each study. These results, combined with the technical difficulties presented by targeting paresthesia-dependent stimulation to the feet, support the development of additional options for treating this patient population.
The study described here will help determine the efficacy of 10-kHz SCS in patients with neuropathic pain due to PDN, a currently underserved patient population. About 100 patients will be randomly assigned to each treatment arm recruited at multiple sites throughout the US, which will result in a greater power to detect statistically and clinically meaningful results compared with prior SCS studies. Follow-up will continue for 24 months to demonstrate long-term outcomes compared with prior pharmacological data. Study sites include both large academic centers and independent pain clinics in geographically diverse areas that will provide a representative patient population. A limitation of the study is the contribution of employees of the sponsor to protocol design and data analysis as this has the potential to introduce bias. Multiple measures have been taken to minimize bias: the participation of outside medical experts in the design of the study; recruitment of independent physician investigators who are responsible for patient selection, data collection, and oversight of study conduct at their sites; concealed allocation of treatment; and the involvement of the CEC to monitor study safety. The primary endpoint results will be reported for the ITT population, and secondary and tertiary outcomes will be reported for the PP population.
Another potential limitation is the cost of the proposed treatment in this study versus CMM. SCS is typically an outpatient procedure during which percutaneous leads and battery are fully implanted. The device in this study is rechargeable, and the expected battery life is in excess of 10 years when used at typical therapeutic settings. This study will collect data on health-care utilization, health-related quality of life, and medication usage to address whether the upfront cost for an implanted medical device can be justified by benefit over the life of the product, similar to what has been reported previously for SCS [67,68,69] (Additional file 1).
Conclusions
The SENZA-PDN study will be the largest RCT conducted to date using SCS in subjects with PDN. This prospective multicenter study will determine whether 10-kHz SCS improves clinical outcomes and health-related quality of life and is a cost-effective treatment for PDN. The current treatments for neuropathic pain secondary to PDN are suboptimal and have limited effectiveness and intolerable side effects. Primary endpoint data are expected in 2020, and 24-month data in 2022.
Trial status
Protocol CA2016–5 US SENZA-PDN-1, revision D (March 19, 2019). The first subject was randomly assigned in October 2017 and the last in August 2019.
Availability of data and materials
Not applicable.
Abbreviations
- AE:
-
Adverse event
- CEC:
-
Clinical events committee
- CMM:
-
Conventional medical management
- eCRF:
-
Electronic case report forms
- EDC:
-
Electronic Data Capture
- IRB:
-
Institutional review board
- ITT:
-
Intention-to-treat
- NeuPSIG :
-
Neuropathic Pain Special Interest Group
- NNH:
-
Number needed to harm
- NNT:
-
Numbers needed to treat
- NRS:
-
Numerical rating scale
- PDN:
-
Painful diabetic neuropathy
- PP:
-
Per protocol
- RCT:
-
Randomized controlled trial
- SEM:
-
Standard error of the mean
- SNRI:
-
Serotonin-noradrenaline reuptake inhibitor
- VAS:
-
Visual analog scale
References
World Health Organization. Global report on diabetes. 2016.
Centers for Disease Control and Prevention. National diabetes statistics report. 2014.
Schmader KE. Epidemiology and impact on quality of life of postherpetic neuralgia and painful diabetic neuropathy. Clin J Pain. 2002;18:350–4.
Hsieh ST. Pathology and functional diagnosis of small-fiber painful neuropathy. Acta Neurol Taiwanica. 2010;19:82–9.
Azhary H, Farooq MU, Bhanushali M, Majid A, Kassab MY. Peripheral neuropathy: differential diagnosis and management. Am Fam Physician. 2010;81:887–92.
Alleman CJ, Westerhout KY, Hensen M, Chambers C, Stoker M, Long S, et al. Humanistic and economic burden of painful diabetic peripheral neuropathy in Europe: a review of the literature. Diabetes Res Clin Pract. 2015;109:215–25.
Dieleman JP, Kerklaan J, Huygen FJ, Bouma PA, Sturkenboom MC. Incidence rates and treatment of neuropathic pain conditions in the general population. Pain. 2008;137:681–8.
Hall GC, Carroll D, McQuay HJ. Primary care incidence and treatment of four neuropathic pain conditions: a descriptive study, 2002-2005. BMC Fam Pract. 2008;9:26.
Dulipsingh L, Zailskas S, Goldsby T, McInnis T, Marotta A. Assessment of pain and treatment satisfaction in patients with painful diabetic peripheral neuropathy. Conn Med. 2013;77:523–7.
Deli G, Bosnyak E, Pusch G, Komoly S, Feher G. Diabetic neuropathies: diagnosis and management. Neuroendocrinology. 2013;98:267–80.
Cole BE. Diabetic peripheral neuropathic pain: recognition and management. Pain Med. 2007;8(Suppl 2):S27–32.
DiBonaventura M, Cappelleri JC, Joshi AV. A longitudinal assessment of painful diabetic peripheral neuropathy on health status, productivity, and health care utilization and cost. Pain Med. 2011;12:118–26.
Yang M, Qian C, Liu Y. Suboptimal treatment of diabetic peripheral neuropathic pain in the United States. Pain Med. 2015;16:2075–83.
Rosenstock J, Tuchman M, LaMoreaux L, Sharma U. Pregabalin for the treatment of painful diabetic peripheral neuropathy: a double-blind, placebo-controlled trial. Pain. 2004;110:628–38.
Lesser H, Sharma U, LaMoreaux L, Poole RM. Pregabalin relieves symptoms of painful diabetic neuropathy: a randomized controlled trial. Neurology. 2004;63:2104–10.
Richter RW, Portenoy R, Sharma U, Lamoreaux L, Bockbrader H, Knapp LE. Relief of painful diabetic peripheral neuropathy with pregabalin: a randomized, placebo-controlled trial. J Pain. 2005;6:253–60.
Arezzo JC, Rosenstock J, Lamoreaux L, Pauer L. Efficacy and safety of pregabalin 600 mg/d for treating painful diabetic peripheral neuropathy: a double-blind placebo-controlled trial. BMC Neurol. 2008;8:33.
Tolle T, Freynhagen R, Versavel M, Trostmann U, Young JP Jr. Pregabalin for relief of neuropathic pain associated with diabetic neuropathy: a randomized, double-blind study. Eur J Pain. 2008;12:203–13.
Tanenberg RJ, Irving GA, Risser RC, Ahl J, Robinson MJ, Skljarevski V, et al. Duloxetine, pregabalin, and duloxetine plus gabapentin for diabetic peripheral neuropathic pain management in patients with inadequate pain response to gabapentin: an open-label, randomized, noninferiority comparison. Mayo Clin Proc. 2011;86:615–26.
Rauck R, Makumi CW, Schwartz S, Graff O, Meno-Tetang G, Bell CF, et al. A randomized, controlled trial of gabapentin enacarbil in subjects with neuropathic pain associated with diabetic peripheral neuropathy. Pain Pract. 2013;13:485–96.
Tesfaye S, Wilhelm S, Lledo A, Schacht A, Tolle T, Bouhassira D, et al. Duloxetine and pregabalin: high-dose monotherapy or their combination? The “COMBO-DN study”--a multinational, randomized, double-blind, parallel-group study in patients with diabetic peripheral neuropathic pain. Pain. 2013;154:2616–25.
Mimenza Alvarado A, Aguilar Navarro S. Clinical trial assessing the efficacy of Gabapentin Plus B Complex (B1/B12) versus Pregabalin for treating painful diabetic neuropathy. J Diabetes Res. 2016;2016:4078695.
Goldstein DJ, Lu Y, Detke MJ, Lee TC, Iyengar S. Duloxetine vs. placebo in patients with painful diabetic neuropathy. Pain. 2005;116:109–18.
Raskin J, Pritchett YL, Wang F, D’Souza DN, Waninger AL, Iyengar S, et al. A double-blind, randomized multicenter trial comparing duloxetine with placebo in the management of diabetic peripheral neuropathic pain. Pain Med. 2005;6:346–56.
Wernicke JF, Pritchett YL, D’Souza DN, Waninger A, Tran P, Iyengar S, et al. A randomized controlled trial of duloxetine in diabetic peripheral neuropathic pain. Neurology. 2006;67:1411–20.
Gao Y, Ning G, Jia W, Zhou Z, Xu Z, Liu Z, et al. Duloxetine versus placebo in the treatment of patients with diabetic neuropathic pain in China. Chin Med J. 2010;123:3184–92.
Kaur H, Hota D, Bhansali A, Dutta P, Bansal D, Chakrabarti A. A comparative evaluation of amitriptyline and duloxetine in painful diabetic neuropathy: a randomized, double-blind, cross-over clinical trial. Diabetes Care. 2011;34:818–22.
Rowbotham MC, Arslanian A, Nothaft W, Duan WR, Best AE, Pritchett Y, et al. Efficacy and safety of the alpha4beta2 neuronal nicotinic receptor agonist ABT-894 in patients with diabetic peripheral neuropathic pain. Pain. 2012;153:862–8.
Schwartz S, Etropolski M, Shapiro DY, Okamoto A, Lange R, Haeussler J, et al. Safety and efficacy of tapentadol ER in patients with painful diabetic peripheral neuropathy: results of a randomized-withdrawal, placebo-controlled trial. Curr Med Res Opin. 2011;27:151–62.
Niesters M, Proto PL, Aarts L, Sarton EY, Drewes AM, Dahan A. Tapentadol potentiates descending pain inhibition in chronic pain patients with diabetic polyneuropathy. Br J Anaesth. 2014;113:148–56.
Vinik AI, Shapiro DY, Rauschkolb C, Lange B, Karcher K, Pennett D, et al. A randomized withdrawal placebo-controlled study evaluating the efficacy and tolerability of tapentadol extended release in patients with chronic painful diabetic peripheral neuropathy. Diabetes Care. 2014;37:2302–9.
de Vos CC, Meier K, Zaalberg PB, Nijhuis HJ, Duyvendak W, Vesper J, et al. Spinal cord stimulation in patients with painful diabetic neuropathy: a multicentre randomized clinical trial. Pain. 2014;155:2426–31.
van Beek M, Slangen R, Schaper NC, Faber CG, Joosten EA, Dirksen CD, et al. Sustained treatment effect of spinal cord stimulation in painful diabetic peripheral neuropathy: 24-month follow-up of a prospective two-center randomized controlled trial. Diabetes Care. 2015;38:e132–4.
Boyle J, Eriksson ME, Gribble L, Gouni R, Johnsen S, Coppini DV, et al. Randomized, placebo-controlled comparison of amitriptyline, duloxetine, and pregabalin in patients with chronic diabetic peripheral neuropathic pain: impact on pain, polysomnographic sleep, daytime functioning, and quality of life. Diabetes Care. 2012;35:2451–8.
Freeman R, Durso-Decruz E, Emir B. Efficacy, safety, and tolerability of pregabalin treatment for painful diabetic peripheral neuropathy: findings from seven randomized, controlled trials across a range of doses. Diabetes Care. 2008;31:1448–54.
Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14:162–73.
Kumar K, Toth C, Nath RK. Spinal cord stimulation for chronic pain in peripheral neuropathy. Surg Neurol. 1996;46:363–9.
Kumar K, Toth C, Nath RK, Laing P. Epidural spinal cord stimulation for treatment of chronic pain--some predictors of success. A 15-year experience. Surg Neurol. 1998;50:110–20 discussion 120–1.
Pluijms WA, Slangen R, Bakkers M, Faber CG, Merkies IS, Kessels AG, et al. Pain relief and quality-of-life improvement after spinal cord stimulation in painful diabetic polyneuropathy: a pilot study. Br J Anaesth. 2012;109:623–9.
Slangen R, Pluijms WA, Faber CG, Dirksen CD, Kessels AG, van Kleef M. Sustained effect of spinal cord stimulation on pain and quality of life in painful diabetic peripheral neuropathy. Br J Anaesth. 2013;111:1030–1.
Tesfaye S, Watt J, Benbow SJ, Pang KA, Miles J, MacFarlane IA. Electrical spinal-cord stimulation for painful diabetic peripheral neuropathy. Lancet. 1996;348:1698–701.
van Beek M, Geurts JW, Slangen R, Schaper NC, Faber CG, Joosten EA, et al. Severity of neuropathy is associated with long-term spinal cord stimulation outcome in painful diabetic peripheral neuropathy: five-year follow-up of a prospective two-center clinical trial. Diabetes Care. 2018;41:32–8.
De Carolis G, Paroli M, Tollapi L, Doust MW, Burgher AH, Yu C, et al. Paresthesia-independence: an assessment of technical factors related to 10 kHz paresthesia-free spinal cord stimulation. Pain Physician. 2017;20:331–41.
Kapural L, Yu C, Doust MW, Gliner BE, Vallejo R, Sitzman BT, et al. Novel 10-kHz high-frequency therapy (HF10 therapy) is superior to traditional low-frequency spinal cord stimulation for the treatment of chronic back and leg pain the SENZA-RCT randomized controlled trial. Anesthesiology. 2015;123:851–60.
Kapural L, Yu C, Doust MW, Gliner BE, Vallejo R, Sitzman BT, et al. Comparison of 10-kHz high-frequency and traditional low-frequency spinal cord stimulation for the treatment of chronic back and leg pain: 24-month results from a multicenter, randomized, controlled pivotal trial. Neurosurgery. 2016;79:667–77.
Al-Kaisy A, Van Buyten J-P, Smet I, Palmisani S, Pang D, Smith T. Sustained effectiveness of 10 kHz high-frequency spinal cord stimulation for patients with chronic, low back pain: 24-month results of a prospective multicenter study. Pain Med (Malden, Mass). 2014;15:347–54.
Stauss T, El Majdoub F, Sayed D, Surges G, Rosenberg WS, Kapural L, et al. A multicenter real-world review of 10 kHz SCS outcomes for treatment of chronic trunk and/or limb pain. Ann Clin Transl Neurol. 2019;6:496–507.
Al-Kaisy A, Van Buyten JP, Amirdelfan K, Gliner B, Caraway D, Subbaroyan J, et al. Opioid sparing effects of 10 kHz spinal cord stimulation: A review of clinical evidence. Ann N Y Acad Sci. 2019. https://doi.org/10.1111/nyas.14236 [Epub ahead of print].
Al-Kaisy A, Van Buyten JP, Carganillo R, Caraway D, Gliner B, Subbaroyan J, et al. 10 kHz SCS therapy for chronic pain, effects on opioid usage: Post hoc analysis of data from two prospective studies. Sci Rep. 2019;9:11441.
Amirdelfan K, Yu C, Doust MW, Gliner BE, Morgan DM, Kapural L, et al. Long-term quality of life improvement for chronic intractable back and leg pain patients using spinal cord stimulation: 12-month results from the SENZA-RCT. Qual Life Res. 2018;27:2035–44.
Al-Kaisy A, Palmisani S, Smith T, Harris S, Pang D. The use of 10-kilohertz spinal cord stimulation in a cohort of patients with chronic neuropathic limb pain refractory to medical management. Neuromodulation. 2015;18:18–23.
Simopoulos T, Yong RJ, Gill JS. Treatment of chronic refractory neuropathic pelvic pain with high-frequency 10-kilohertz spinal cord stimulation. Pain Pract. 2018;18:805–9.
Gill JS, Asgerally A, Simopoulos TT. High frequency spinal cord stimulation at 10 kHz for the treatment of complex regional pain syndrome: a case series of patients with or without previous spinal cord stimulator implantation. Pain Pract. 2019;19:289–94.
Amirdelfan K, Vallejo R, Benyamin R, Yu C, Yang T, Bundschu R, et al. High-frequency Spinal Cord Stimulation at 10 kHz for the treatment of combined neck and arm pain. Results from prospective multicenter study. Neurosurgery. 2019. [Epub ahead of print].
Galan V, Chang P, Scowcroft J, Li S, Staats P, Subbaroyan J. A prospective clinical trial to assess high frequency spinal cord stimulation (HF-SCS) at 10 kHz in the treatment of chronic intractable pain from peripheral polyneuropathy. In: The 22nd annnual meeting of the North American neuromodulation society; Las Vegas, NV, vol. 2019; 2019.
Pop-Busui R, Boulton AJ, Feldman EL, Bril V, Freeman R, Malik RA, et al. Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care. 2017;40:136–54.
Olsen MF, Bjerre E, Hansen MD, Tendal B, Hilden J, Hrobjartsson A. Minimum clinically important differences in chronic pain vary considerably by baseline pain and methodological factors: systematic review of empirical studies. J Clin Epidemiol. 2018;101:87–106.e102.
Amirdelfan K, Gliner BE, Kapural L, Sitzman BT, Vallejo R, Yu C, et al. A proposed definition of remission from chronic pain, based on retrospective evaluation of 24-month outcomes with spinal cord stimulation. Postgrad Med. 2019;131:278–86.
Bouhassira D, Attal N, Alchaar H, Boureau F, Brochet B, Bruxelle J, et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain. 2005;114:29–36.
Young MJ, Boulton AJ, MacLeod AF, Williams DR, Sonksen PH. A multicentre study of the prevalence of diabetic peripheral neuropathy in the United Kingdom hospital clinic population. Diabetologia. 1993;36:150–4.
Zelman DC, Gore M, Dukes E, Tai KS, Brandenburg N. Validation of a modified version of the brief pain inventory for painful diabetic peripheral neuropathy. J Pain Symptom Manag. 2005;29:401–10.
Dworkin RH, Turk DC, Revicki DA, Harding G, Coyne KS, Peirce-Sandner S, et al. Development and initial validation of an expanded and revised version of the Short-form McGill Pain Questionnaire (SF-MPQ-2). Pain. 2009;144:35–42.
Diabetes Control and Complications Trial. Reliability and validity of a diabetes quality-of-life measure for the Diabetes Control and Complications Trial (DCCT). Diabetes Care. 1988;11:725–32.
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20:1727–36.
Ayearst LE, Harsanyi Z, Michalko KJ. The Pain and Sleep Questionnaire three-item index (PSQ-3): a reliable and valid measure of the impact of pain on sleep in chronic nonmalignant pain of various etiologies. Pain Res Manag. 2012;17:281–90.
American Thoracic Society. American thoracic society statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–7.
Annemans L, Van Buyten J-P, Smith T, Al-Kaisy A. Cost effectiveness of a novel 10 kHz high-frequency spinal cord stimulation system in patients with failed back surgery syndrome (FBSS). J Long Term Eff Med Implants. 2014;24:173–83.
Taylor RS, Taylor RJ, Van Buyten JP, Buchser E, North R, Bayliss S. The cost effectiveness of spinal cord stimulation in the treatment of pain: a systematic review of the literature. J Pain Symptom Manag. 2004;27:370–8.
Taylor RJ, Taylor RS. Spinal cord stimulation for failed back surgery syndrome: a decision-analytic model and cost-effectiveness analysis. Int J Technol Assess Health Care. 2005;21:351–8.
Acknowledgments
The authors thank Peter J. Neumann, ScD, from the Center for the Evaluation of Value and Risk in Health at Tufts Medical Center, for his thoughtful input.
Funding
This study is funded by Nevro. Employees of Nevro collaborated with an expert steering committee to design the study. Independent investigators are responsible for the conduct of the study and data collection. Data analysis will be performed by an independent statistician. Both Nevro employees and the investigators will interpret the data and write subsequent manuscripts.
Author information
Authors and Affiliations
Contributions
All of the authors collaborated on the design of the study and have read and approved this manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
IRB approval was obtained for the study prior to subject recruitment, and all participating subjects provided written informed consent. The study was approved by Western IRB on July 20, 2017.
Consent for publication
Not applicable.
Competing interests
NAM served as independent medical monitor for the Senza PDN study. CEA, RST, and CN have received consulting fees from Nevro. DLC, BEG, JS, and ESB are employees of Nevro.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
SPIRIT (Standard Protocol Items: Recommendations for Interventional Trials) 2013 Checklist.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Mekhail, N.A., Argoff, C.E., Taylor, R.S. et al. High-frequency spinal cord stimulation at 10 kHz for the treatment of painful diabetic neuropathy: design of a multicenter, randomized controlled trial (SENZA-PDN). Trials 21, 87 (2020). https://doi.org/10.1186/s13063-019-4007-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-019-4007-y