Abstract
Background
Extracorporeal cardiopulmonary resuscitation (ECPR) is rapidly becoming a common treatment strategy for patients with refractory cardiac arrest. Despite its benefits, ECPR raises a variety of ethical concerns when the treatment is discontinued. There is little information about the decision to withhold/withdraw life-sustaining therapy (WLST) for out-of-hospital cardiac arrest (OHCA) patients after ECPR.
Methods
We conducted a secondary analysis of data from the SAVE-J II study, a retrospective, multicenter study of ECPR in Japan. Adult patients who underwent ECPR for OHCA with medical causes were included. The prevalence, reasons, and timing of WLST decisions were recorded. Outcomes of patients with or without WLST decisions were compared. Further, factors associated with WLST decisions were examined.
Results
We included 1660 patients in the analysis; 510 (30.7%) had WLST decisions. The number of WLST decisions was the highest on the first day and WSLT decisions were made a median of two days after ICU admission. Reasons for WLST were perceived unfavorable neurological prognosis (300/510 [58.8%]), perceived unfavorable cardiac/pulmonary prognosis (105/510 [20.5%]), inability to maintain extracorporeal cardiopulmonary support (71/510 [13.9%]), complications (10/510 [1.9%]), exacerbation of comorbidity before cardiac arrest (7/510 [1.3%]), and others. Patients with WLST had lower 30-day survival (WLST vs. no-WLST: 36/506 [7.1%] vs. 386/1140 [33.8%], p < 0.001). Primary cerebral disorders as cause of cardiac arrest and higher severity of illness at intensive care unit admission were associated with WLST decisions.
Conclusion
For approximately one-third of ECPR/OHCA patients, WLST was decided during admission, mainly because of perceived unfavorable neurological prognoses. Decisions and neurological assessments for ECPR/OHCA patients need further analysis.
Similar content being viewed by others
Background
As an advanced treatment strategy, extracorporeal cardiopulmonary resuscitation (ECPR) continues to improve the care of patients after out-of-hospital cardiac arrest (OHCA) [1,2,3]. Despite its benefits, ECPR is still associated with significant morbidity [4], including brain ischemia/injury [5] leading to prolonged neurological impairment. Survival with good neurological outcome after ECPR is still not sufficiently high [6]. The decision to initiate ECPR must be made under emergency conditions with time constraints and uncertainty of prognosis. After ECPR induction, it may become apparent that the patient’s predicted prognosis is extremely poor and aggressive treatment is no longer reasonable. As a result, it may become necessary to adjust goals for end-of-life decision-making, including establishing treatment limits or discontinuing extracorporeal membrane oxygenation (ECMO) or life-sustaining therapies.
Discontinuing ECPR or other life-sustaining therapies raises a variety of ethical concerns due to the lack of internationally accepted guidelines for termination of resuscitation [7], uncertainty of neurological prognosis testing in the acute phase [8], and the medical futility of continuing ECPR in certain situations [9]. Although treatment may sometimes be withheld or discontinued for cases with extremely poor prognoses, there is little information concerning decision criteria to withhold/withdraw life-sustaining therapy (WLST) for OHCA patients after ECPR. Past studies have been limited by sample size [10] or by including only patients who died after the decision to withdraw life-sustaining therapy [11].
The aim of this study was to describe WLST decisions for OHCA patients after ECPR. Prevalence, reasons, and timing for WLST decisions were examined. Further, the differences between ECPR/OHCA patients with or without WLST were compared.
Methods
Study design
This was a secondary analysis of a nationwide, retrospective, observational ECPR study (SAVE-J II). The Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences and the Okayama University Hospital Ethics Committee approved the study (K2209-018) and waived the requirement for written informed consent.
Data collection
Data for the analysis was obtained from the SAVE-J II study (ECPR data collected from 36 intensive care units (ICUs) in Japan from 2013 to 2018). The study design and data collection methods of the SAVE-J II study have been described previously [12]. The SAVE-J II study included consecutive patients with OHCA aged ≥ 18 years old who were resuscitated with ECPR at participating institutions during the study period.
ECPR and ECMO care in the ICU
In Japan, acute care physicians or emergency physician intensivists generally direct the entire clinical practice of OHCA, including ECPR; they provide the continuum of care from the emergency department to post-resuscitation or ECMO care in the ICU. In addition, patient management commonly involves collaboration with cardiologists [13, 14].
Patient selection and endpoint
Patients registered in the SAVE-J II study were screened for eligibility. Patients treated with ECPR for OHCA with medical causes were included [15], and patients with missing WLST data were excluded. The primary outcome of the study was WLST decision in OHCA patients with ECPR. Prevalence, reasons, and timing for WLST decisions were described. The secondary outcome of the study was 30-day survival, 30-day neurological outcomes, and medical cost during hospitalization. Differences between ECPR/OHCA patients with or without WLST were compared.
Definitions and measurements
WLST was defined as medical interventions withheld or withdrawn, including ECMO or other life-sustaining treatments, with the understanding that the patient would most likely die from the underlying post-cardiac arrest syndrome or other causes. In this study, WLST was the combination of two categories: withholding life-sustaining treatment and withdrawal of life-sustaining treatment. Withholding life-sustaining treatment is commonly considered the establishment of treatment limits with no escalation of use of devices (including ECMO, ventilator, etc.) or drugs; withdrawal of life-sustaining treatment in Japan is commonly considered the termination of device use, pharmacological interventions, and/or other therapies. After a thorough review of each patient’s medical record, the physician in charge at each study site retrospectively determined the reason for the WLST decision and the date when the decision was made. One of the following six reasons were determined for each case: (1) inability to maintain extracorporeal cardiopulmonary support; (2) complications; (3) perceived unfavorable neurological prognosis; (4) perceived unfavorable cardiac/pulmonary prognosis; (5) exacerbation of comorbidity before cardiac arrest; (6) or others. The WLST group was defined as patients with WLST decisions (combination of withholding and withdrawal of life-sustaining treatment) during their stay in the participating hospital, and the no WLST group was defined as patients with no WLST.
The following patient data were collected from the SAVE-J II study database [12]: gender, age, cardiac arrest location, Eastern Cooperative Oncology Group performance status (PS) before admission (a lower PS score indicates a higher level of performance of daily activities: a score of 0 indicates that the patient is fully active and able to carry out all activities without restriction, while a score of 4 indicates that the patient is completely disabled and bedridden [16]), initial cardiac rhythm, presumed cardiac origin, witness of cardiac arrest, bystander cardiopulmonary resuscitation (CPR), ECPR information (time from emergency medical services scene arrival to ECMO pump on, use of intra-aortic balloon pump, ECMO-related complications), and ICU data/treatments (pH, serum lactate level, sequential organ failure assessment [SOFA] score, pupil diameter at ICU admission, and comorbidity/treatments in the ICU). In this study, SOFA score was defined without the respiratory score due to the uncertainty of effects of ECMO and mechanical ventilation on the respiratory score (i.e., the max score is 16 points). WLST data, including the time the decision was obtained and the reason for WLST, was collected and recorded. Favorable neurological outcomes, defined as Cerebral Performance Category (CPC) score of 1 or 2 at 30 days after cardiac arrest, were obtained. Survival at 30 days and medical cost incurred during the hospitalization were recorded.
Statistical analysis
Continuous variables were described using median with interquartile ranges. Categorical variables are described using percentages. Comparisons between two groups were made using the Mann–Whitney U test for continuous variables and the chi-square test for categorical variables. Kaplan–Meier survival curve was drawn for the comparison of 30-day survival of the WLST and no WLST groups with log-rank test. A multiple logistic regression model was applied to estimate adjusted odds ratios (ORs) with their 95% confidence intervals for the primary outcome. We selected confounding variables as follows: age, gender, PS before cardiac arrest, primary cerebral disorders as cause of cardiac arrest, time from scene to ECMO pump on, pupil diameter (≥ 6 mm) on ICU admission, SOFA score at ICU admission, lactate level at ICU admission, and ECMO complications. These variables were selected based on previous reports and our hypothesis was that these variables were potentially associated with WLST [10, 11]. All statistical analysis was performed using Stata version 17 (StataCorp LP, College Station, TX).
Results
Patient characteristics
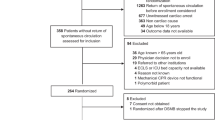
Figure 1 shows a flow chart depicting how patients were determined to be eligible for analysis. During the study period, data on 2157 patients were entered into the SAVE-J II Study registry. A total of 1759 patients met the inclusion criteria. Patients meeting the exclusion criteria (99 patients missing WLST data) were excluded. Finally, 1660 patients were included in the analysis, 510 patients (30.7%) of which had WLST decisions during admission. Of the 510 WLST patients, the decision was made to withdraw life-sustaining treatment for 327 patients and the decision was made to withhold life-sustaining treatment was made for 158 patients.
Patient characteristics are shown in Table 1. In the univariable analysis, WLST patient age was higher (WLST vs. no WLST: 62 [51–70] vs. 61 [49–69], p = 0.032). Patients with WLST were more likely to have primary cerebral disorders as the cause of cardiac arrest (32/502 [6.3%] vs. 18/1137 [1.5%], p < 0.001), higher serum lactate levels at ICU admission (8.3 [5.7–12.0] vs. 7.6 [5.0–11.3] mmol/L, p = 0.008), a higher prevalence of dilated pupils (≥ 6 mm) on ICU admission (57/420 [13.5%] vs. 75/813 [9.2%], p = 0.019), and a higher prevalence of acute renal failure (218/455 [47.9%] vs. 335/894 [37.4%], p < 0.001).
Status and reasons for WLST decisions, time to obtain WLST decisions
Table 2 shows the reasons for WLST decisions. Reasons for WLST decisions were perceived unfavorable neurological prognosis (300/510 [58.8%]), perceived unfavorable cardiac/pulmonary prognosis (105/510 [20.5%]), inability to maintain extracorporeal cardiopulmonary support (71/510 [13.9%]), complications (10/510 [1.9%]), exacerbation of comorbidity before cardiac arrest (7/510 [1.0%]), and others (4/510 [1.0%]). Proportions for each WLST reason did not differ between patients with withdrawal of life-sustaining treatment decisions and patients with withholding of life-sustaining treatment decisions. WLST was decided at a median of 2 [1–6] days. Figure 2 shows the days on which WLST decisions were made. The number of WLST decisions was the highest on the first day; the number of WLST decisions decreased with time. The trend for WLST did not differ by WLST reason (Additional file 1).
One-month survival and other patient outcomes
Table 3 shows patient outcomes. Overall, 422/1646 (25.6%) of the patients survived at 30 days. Favorable neurological outcomes were seen in 214/1646 (13.0%) of the patients. A median of $23,000 US dollars was spent to treat the patients during hospitalization. Thirty-day survival (p < 0.001, see also Fig. 3) and 30-day neurological outcomes were better in the no WLST group (p < 0.001), while medical cost during hospitalization was lower in the WLST group (p < 0.001). Thirty-day survival was better in the withholding life-sustaining treatment decision group compared to the withdrawal of life-sustaining treatment decision group (p < 0.001, Additional file 2).
Factors related to WLST decisions
Table 4 shows the results of multivariable logistic regression for WLST decisions. Primary cerebral disorders as cause of cardiac arrest (adjusted OR 6.67 [1.29–34.5], p = 0.023), SOFA score on ICU admission (adjusted OR 1.05 [1.00–1.09], p = 0.017), and lactate level on ICU admission (adjusted OR 1.04 [1.01–1.08], p = 0.007) were the factors associated with WLST decisions after adjustment.
Discussion
In this study, we described the prevalence and reasons for WLST decisions in patients who underwent ECPR in a Japanese nationwide registry. WLST decisions were made most frequently on the first day and the median time until WLST decisions were made was two days in our ECPR population. Surprisingly, the majority of attending physicians disclosed that the reason for WLST was perceived unfavorable neurological prognosis, although we could not examine whether they could actually estimate the patient’s prognosis at this early time. Patients experiencing WLST had higher mortalities and incurred lower medical costs compared to those without WLST.
Approximately one third (30.7%) of our ECPR population had WLST decisions during their hospital stay. A previous report demonstrated that in a general population of OHCA patients with conventional CPR, WLST at any time/for any reason occurred in 43% of the patients [17]. Similarly, in the other conventional CPR population study, withdrawal of life-sustaining therapy for perceived poor neurologic prognosis occurred in 25% of hospitalized patients [18]. Although our ECPR cohort had a high proportion (13.0%) of favorable neurological outcomes, the prevalence of WLST was comparable with that of the general conventional CPR OHCA population.
Although guidelines recommend avoiding early WLST in patients after cardiac arrest [19, 20], the timing for WLST decisions was surprisingly early in our ECPR cohort, with a mode of one day and a median of two days after ICU admission, which is different from the conventional CPR population, in which 17% of hospitalized OHCA patients had WLST within three calendar days [17]. Past literature on WLST in ECPR patients is limited; however, similar to our study, the prevalence of early WLST in ECPR patients in these previous studies seems to be high. Our results were consistent with those from a past report that used data from The Extracorporeal Life Support Organization (ELSO) registry. Carlson et al. reported that decisions to withdraw life-sustaining therapy most commonly occurred on day one [11]. Additionally, Haas et al. reported that more than one third of non-survivors’ ECPR was discontinued within 24 h of ECPR initiation, although the number of WLST decisions was not described [21]. Early WLST may eliminate the chance of survival during a time when prognostic estimation is not possible; this may lead to excess mortality. Elmer et al. reported that WLST decisions due to presumed poor neurological prognosis were made within 72 h in one-third of OHCA patients that died in-hospital. If life-sustaining therapy was not withdrawn before 72 h, two prognostic models derived from a large database in North America predicted that 26% of those who died due to early withdrawal of life-sustaining therapy decision might have survived and 16% of those who died might have had functionally favorable survival [22].
In our study, some of the patient’s baseline demographics were associated with WLST. When adjusted in the multivariable regression model, primary cerebral disorders as cause of cardiac arrest, SOFA score on ICU admission, and lactate level on ICU admission were factors associated with WLST. This finding is consistent with that from a previous study showing that severity of illness was associated with WLST within 72 h in ECPR patients [10]. We additionally found that primary cerebral disorders, commonly associated with poor favorable outcomes, were strongly associated with WLST.
Carlson et al. described clinical outcomes of WLST in ECMO patients in a single center; all 73 patients (100%) with WLST decisions died [10]. In our analysis, 7.1% of the WLST group survived until 30 days, but none survived with 30-day good neurological outcomes. We found a significant difference in survival between the WLST group and the no WLST group; further, there were significant differences in survival between patients with withdrawal of life-sustaining therapy and patients with withholding of life-sustaining therapy. These findings raise concerns for early WLST based on presumed unfavorable neurological outcome. Inappropriately predicting a poor neurological outcome may result in a self-fulfilling prophecy. Using such a prognostication to guide early WLST may have a critical impact on survival.
There still are numerous barriers to ECPR implementation; some of the issues with ECPR are medical cost and clinical effectiveness for OHCA patients [23]. Japan's universal coverage charges patients a very low cost, covering most hospitalization costs under national health care expenditures [24]. Still, in this study, medical cost in the WLST group was lower due to early death with WLST. However, our data are insufficient to quantify the social or economic costs for death associated with WLST.
The decision for WLST depends on a variety of factors. Besides the patient's medical condition or medical cost, patient/family cultural and religious beliefs, values, and preferences may affect the decisions [25]. Despite Japanese guidelines regarding end-of-life-care that provide a basis for WLST decisions and decision-making using a multidisciplinary approach, physicians in Japan often prefer to not withhold or withdraw life-sustaining therapy in the ICU [26]. However, this would not apply to specific situations in which neurological damage is so catastrophic that functional recovery is extremely unlikely. Remarkably, a recent study from Japan demonstrated that almost all WLST decisions were made through discussions between patients’ family members and attending emergency physician intensivists/neurosurgeons within 24 h after admission for severe traumatic brain injury [27]. Early WLST decision in our study may be in part attributed to the physician’s perception of futility that the patient would have a poor neurological prognosis or a “bridge to nowhere.” It is also speculated that attending physicians/families decided WLST with the self-fulfilling prophecy that the patient would have an unfavorable outcome. Physicians should be aware that the self-fulfilling prophecy that may result from inappropriate pessimistic neurological prognostication has a detrimental impact on patient outcomes. Withdrawal of life-sustaining therapy is a critical factor for estimated excessive mortality in cardiac arrest with conventional CPR [17, 22] or intracerebral hemorrhage [28]. Future research should aim to coherently clarify the decision-making process for why ECMO care, which is expensive and time-consuming, was withdrawn or withheld as early as 1–2 days in ECPR patients.
Limitations
The study has several limitations. First, this study was conducted as a post-hoc analysis of data from a Japanese nationwide registry [12]; decisions and treatments of ECPR patients were left to the discretion of attending physicians and family members. We did not have any specific protocol for WLST decisions. We were unable to investigate specific findings that may have underpinned physicians’ perceptions of unfavorable neurological or cardiac/pulmonary prognoses. We did not have data on the WLST decision-making process, so we did not know whether a multidisciplinary team approach was used or whether a family member initiated the decision, or the roles of family members, physicians (emergency physician intensivists, cardiologists, etc.), and other healthcare professionals, including social workers or ethical consultants. Second, the most appropriate reason for WLST was chosen by the researchers of the participating facility based on medical records. Retrospectively choosing one of six possible reasons for WLST is not likely to reflect the complexity of such decisions that also include multiple other factors, including family/attending physician discretion, late found advance directives, or economic factors. Our study did not set specific guidelines for choosing WLST reasons. Finally, this study is based on data from a single nation; culture, ethics, and economic setting may affect WLST decisions, which may limit the generalizability of our findings. However, our data is consistent with previous international registry data [11].
Despite these limitations, our study provides valuable data on the prevalence, reasons, and timing for WLST decisions in OHCA patients with ECPR using a large nationwide cohort. Further research is needed to investigate more accurate neurologic prognostication in the early phase in OHCA/ECPR patients to allow more in-depth WLST decision pathways, which could guide clinicians in making medically and ethically appropriate decisions.
Conclusions
WLST decisions were made for about one-third of ECPR/OHCA patients in a Japanese nationwide cohort. The main reason for WLST decisions was perceived unfavorable neurological prognosis. Decisions were made early, at a median of two days after ICU admission during a time when neurological prognostication is not recommended. Decisions and neurological assessments for ECPR/OHCA patients need further analysis.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the authors upon reasonable request.
Abbreviations
- CPC:
-
Cerebral Performance Category
- ECMO:
-
Extracorporeal membrane oxygenation
- ECPR:
-
Extracorporeal cardiopulmonary resuscitation
- ICU:
-
Intensive care unit
- OHCA:
-
Out-of-hospital cardiac arrest
- OR:
-
Odds ratio
- PS:
-
Performance status
- ROSC:
-
Return of spontaneous circulation
- SOFA:
-
Sequential organ failure assessment
- WLST:
-
Withdrawal/withholding of life-sustaining therapy
References
Lunz D, Calabrò L, Belliato M, Contri E, Broman LM, Scandroglio AM, et al. Extracorporeal membrane oxygenation for refractory cardiac arrest: a retrospective multicenter study. Intensive Care Med. 2020;46:973–82.
Miraglia D, Miguel LA, Alonso W. Extracorporeal cardiopulmonary resuscitation for in- and out-of-hospital cardiac arrest: systematic review and meta-analysis of propensity score-matched cohort studies. J Am Coll Emerg Phys Open. 2020;1:342–61.
Bougouin W, Dumas F, Lamhaut L, Marijon E, Carli P, Combes A, et al. Extracorporeal cardiopulmonary resuscitation in out-of-hospital cardiac arrest: a registry study. Eur Heart J. 2020;41:1961–71.
Klee TE, Kern KB. A review of ECMO for cardiac arrest. Resusc Plus. 2021;5:100083.
Shoskes A, Migdady I, Rice C, Hassett C, Deshpande A, Price C, et al. Brain injury is more common in venoarterial extracorporeal membrane oxygenation than venovenous extracorporeal membrane oxygenation: a systematic review and meta-analysis. Crit Care Med. 2020;48:1799–808.
Fagnoul D, Combes A, De Backer D. Extracorporeal cardiopulmonary resuscitation. Curr Opin Crit Care. 2014;20:259–65.
Dalle Ave AL, Shaw DM, Gardiner D. Extracorporeal membrane oxygenation (ECMO) assisted cardiopulmonary resuscitation or uncontrolled donation after the circulatory determination of death following out-of-hospital refractory cardiac arrest—an ethical analysis of an unresolved clinical dilemma. Resuscitation. 2016;108:87–94.
Nolan JP, Sandroni C, Böttiger BW, Cariou A, Cronberg T, Friberg H, et al. European Resuscitation Council and European Society of Intensive Care Medicine guidelines 2021: post-resuscitation care. Intensive Care Med. 2021;47:369–421.
Belohlavek J, Smalcova J, Rob D, Franek O, Smid O, Pokorna M, et al. Effect of intra-arrest transport, extracorporeal cardiopulmonary resuscitation, and immediate invasive assessment and treatment on functional neurologic outcome in refractory out-of-hospital cardiac arrest. JAMA. 2022;327:737–47.
Carlson JM, Etchill EW, Enriquez CAG, Peeler A, Whitman GJ, Choi CW, et al. Population characteristics and markers for withdrawal of life-sustaining therapy in patients on extracorporeal membrane oxygenation. J Cardiothorac Vasc Anesth. 2022;36:833–9.
Carlson JM, Etchill E, Whitman G, Kim BS, Choi CW, Tonna JE, et al. Early withdrawal of life sustaining therapy in extracorporeal cardiopulmonary resuscitation (ECPR): results from the extracorporeal life support organization registry. Resuscitation. 2022;179:71–7.
Inoue A, Hifumi T, Sakamoto T, Okamoto H, Kunikata J, Yokoi H, et al. Extracorporeal cardiopulmonary resuscitation in adult patients with out-of-hospital cardiac arrest: a retrospective large cohort multicenter study in Japan. Crit Care. 2022;26:129.
Kitamura T, Iwami T, Atsumi T, Endo T, Kanna T, Kuroda Y, et al. The profile of Japanese Association for Acute Medicine—out-of-hospital cardiac arrest registry in 2014–2015. Acute Med Surg. 2018;5:249–58.
Hifumi T, Inoue A, Takiguchi T, Watanabe K, Ogura T, Okazaki T, et al. Variability of extracorporeal cardiopulmonary resuscitation practice in patients with out-of-hospital cardiac arrest from the emergency department to intensive care unit in Japan. Acute Med Surg. 2021;8:e647.
Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out-of-hospital cardiac arrest: a statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American Heart Association, European resuscitation council, Australian and New Zealand council on resuscitation, heart and stroke foundation of Canada, interamerican heart foundation, resuscitation council of southern Africa, resuscitation council of Asia); and the American Heart Association emergency cardiovascular care Committee and the council on cardiopulmonary, critical care, perioperative and resuscitation. Circulation. 2015;132:1286–300.
National Cancer Institute, DCTD division of cancer treatment & diagnosis. Performance status scales/scores. In: Common toxicity criteria (CTC) v2.0. 1999. https://ctep.cancer.gov/protocoldevelopment/electronic_applications/ctc.htm. Accessed 20 May 2023.
May TL, Ruthazer R, Riker RR, Friberg H, Patel N, Soreide E, et al. Early withdrawal of life support after resuscitation from cardiac arrest is common and may result in additional deaths. Resuscitation. 2019;139:308–13.
Steinberg A, Abella BS, Gilmore EJ, Hwang DY, Kennedy N, Lau W, et al. Frequency of withdrawal of life-sustaining therapy for perceived poor neurologic prognosis. Crit Care Explor. 2021;3:e0487.
Soar J, Berg KM, Andersen LW, Böttiger BW, Cacciola S, Callaway CW, et al. Adult advanced life support: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2020;156:A80-119.
Wijdicks EF, Hijdra A, Young GB, Bassetti CL, Wiebe S. Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2006;67:203–10.
Haas NL, Coute RA, Hsu CH, Cranford JA, Neumar RW. Descriptive analysis of extracorporeal cardiopulmonary resuscitation following out-of-hospital cardiac arrest-An ELSO registry study. Resuscitation. 2017;119:56–62.
Elmer J, Torres C, Aufderheide TP, Austin MA, Callaway CW, Golan E, et al. Association of early withdrawal of life-sustaining therapy for perceived neurological prognosis with mortality after cardiac arrest. Resuscitation. 2016;102:127–35.
Matsuoka Y, Goto R, Atsumi T, Morimura N, Nagao K, Tahara Y, et al. Cost-effectiveness of extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest: a multi-centre prospective cohort study. Resuscitation. 2020;157:32–8.
Shibuya K, Hashimoto H, Ikegami N, Nishi A, Tanimoto T, Miyata H, et al. Future of Japan’s system of good health at low cost with equity: beyond universal coverage. Lancet. 2011;378:1265–73.
Phua J, Joynt GM, Nishimura M, Deng Y, Myatra SN, Chan YH, et al. Withholding and withdrawal of life-sustaining treatments in intensive care units in Asia. JAMA Intern Med. 2015;175:363–71.
Makino J, Fujitani S, Twohig B, Krasnica S, Oropello J. End-of-life considerations in the ICU in Japan: ethical and legal perspectives. J Intensive Care. 2014;2:9.
Tanizaki S, Toma Y, Miyashita K, Maeda S. The characteristics of withdrawal or withholding of life-sustaining treatment in severe traumatic brain injury: a single Japanese institutional study. World Neurosurg X. 2022;17:100144.
Zahuranec DB, Brown DL, Lisabeth LD, Gonzales NR, Longwell PJ, Smith MA, et al. Early care limitations independently predict mortality after intracerebral hemorrhage. Neurology. 2007;68:1651–7.
Acknowledgements
We thank Christine Burr for English language editing. We also thank all the members of the SAVE-J II study group who participated in this study: Hirotaka Sawano, M.D., Ph.D. (Osaka Saiseikai Senri Hospital), Yuko Egawa, M.D., Shunichi Kato, M.D. (Saitama Red Cross Hospital), Naofumi Bunya, M.D., Takehiko Kasai, M.D. (Sapporo Medical University), Shinichi Ijuin, M.D., Shinichi Nakayama, M.D., Ph.D. (Hyogo Emergency Medical Center), Jun Kanda, M.D., Ph.D., Seiya Kanou, M.D. (Teikyo University Hospital), Toru Takiguchi, M.D., Shoji Yokobori, M.D., Ph.D. (Nippon Medical School), Kazushige Inoue, M.D. (National Hospital Organization Disaster Medical Center), Ichiro Takeuchi, M.D., Ph.D., Hiroshi Honzawa, M.D. (Yokohama City University Medical Center), Makoto Kobayashi, M.D., Ph.D., Tomohiro Hamagami, M.D. (Toyooka Public Hospital), Wataru Takayama, M.D., Yasuhiro Otomo, M.D., Ph.D. (Tokyo Medical and Dental University Hospital of Medicine), Kunihiko Maekawa, M.D. (Hokkaido University Hospital), Takafumi Shimizu, M.D., Satoshi Nara, M.D. (Teine Keijinkai Hospital), Michitaka Nasu, M.D., Kuniko Takahashi, M.D. (Urasoe General Hospital), Yoshihiro Hagiwara, M.D., M.P.H. (Imperial Foundation Saiseikai, Utsunomiya Hospital), Shigeki Kushimoto, M.D., Ph.D. (Tohoku University Graduate School of Medicine), Reo Fukuda, M.D. (Nippon Medical School Tama Nagayama Hospital), Takayuki Ogura, M.D., Ph.D. (Japan Red Cross Maebashi Hospital), Shin-ichiro Shiraishi, M.D. (Aizu Central Hospital), Ryosuke Zushi, M.D. (Osaka Mishima Emergency Critical Care Center), Norio Otani, M.D. (St. Luke’s International Hospital), Migaku Kikuchi, M.D., Ph.D. (Dokkyo Medical University), Kazuhiro Watanabe, M.D. (Nihon University Hospital), Takuo Nakagami, M.D. (Omihachiman Community Medical Center), Tomohisa Shoko, M.D., Ph.D. (Tokyo Women’s Medical University Medical Center East), Nobuya Kitamura, M.D., Ph.D. (Kimitsu Chuo Hospital), Takayuki Otani, M.D. (Hiroshima City Hiroshima Citizens Hospital), Yoshinori Matsuoka, M.D., Ph.D. (Kobe City Medical Center General Hospital), Makoto Aoki, M.D., Ph.D. (Gunma University Graduate School of Medicine), Hideki Arimoto, M.D. (Osaka City General Hospital), Koichiro Homma, M.D., Ph.D. (Keio University School of Medicine), Shunichiro Nakao, M.D., Ph.D. (Osaka University Graduate School of Medicine), Tomoya Okazaki, M.D., Ph.D. (Kagawa University Hospital), Yoshio Tahara, M.D., Ph.D. (National Cerebral and Cardiovascular Center), Hiroshi Okamoto, M.D, M.P.H. (St. Luke’s International Hospital), Jun Kunikata, M.D., Ph.D., and Hideto Yokoi, M.D., Ph.D. (Kagawa University Hospital).
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Consortia
Contributions
HN had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. HN and MS wrote the first and subsequent drafts of the manuscript. HN, MS, AI, TH, TS, YK, and AN conceived and designed the study. HN, MS, TH, HT, TY, TY, TH, AI, TS, YK, and AN acquired and interpreted the data. HN, MS, TH, and TY analyzed the data. All authors reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
This study conforms to the principles outlined in the Declaration of Helsinki and was approved by the Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences and the Okayama University Hospital Ethics Committee (ID: K K2209-018). Patient consent was waived.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
The days of WLST decisions are shown with each WLST decision reason. The trend for WLST did not differ by WLST reason. WLST: withholding/withdrawal of life-sustaining therapy
Additional file 2.
Kaplan–Meier survival curve was drawn for the comparison of 30-day survival of withholding of life-sustaining therapy patients and withdrawal of life-sustaining therapy patients with log-rank test. Thirty-day survival was better in the withholding of life-sustaining therapy patients (p < 0.001)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Naito, H., Sakuraya, M., Hongo, T. et al. Prevalence, reasons, and timing of decisions to withhold/withdraw life-sustaining therapy for out-of-hospital cardiac arrest patients with extracorporeal cardiopulmonary resuscitation. Crit Care 27, 252 (2023). https://doi.org/10.1186/s13054-023-04534-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-023-04534-2