Abstract
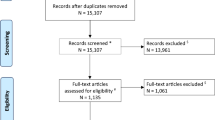
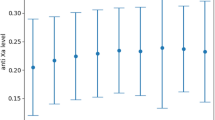
Multiple studies have addressed deep vein thrombosis chemoprophylaxis timing in traumatic brain injuries. However, a precise time for safe and effective chemoprophylaxis is uncertain according to experts. A comprehensive literature review on brain injuries was performed to delineate temporal proportions for 1) spontaneous intracranial hemorrhage (ICH) progression, 2) post-chemoprophylaxis ICH expansion, and 3) post-chemoprophylaxis deep vein thrombosis. Twenty-three publications were found including more than 5,000 patients. Spontaneous ICH expansion at 24 hours was 14.8% in 1,437 patients from chemoprophylaxis studies and 29.9% in 1,257 patients not in chemoprophylaxis studies (P < 0.0001). With low-risk ICH (n = 136), 99% of spontaneous ICH expansion occurred within 48 hours. In moderate or high-risk ICH (n = 109), 18% of spontaneous ICH expansion occurred after day 3. If patients with pre-chemoprophylaxis ICH expansion are included, the post-chemoprophylaxis ICH expansion proportion was 5.6% in 1,258 patients with chemoprophylaxis on days 1 to 3 and was 1.5% in 401 with chemoprophylaxis after day 3 (P = 0.0116). If patients with pre-chemoprophylaxis ICH expansion were excluded, the post-chemoprophylaxis ICH expansion proportion was 3.1% in 1,570 patients with chemoprophylaxis on days 1 to 3 and was 2.8% in 582 with chemoprophylaxis after day 3 (P = 0.7769). In diffuse axonal injury (n = 188), the post-chemoprophylaxis ICH expansion proportion was 1.6% with chemoprophylaxis after day 3. The deep vein thrombosis proportions were as follows: chemoprophylaxis on days 1 to 3, 2.6% in 2,384 patients; chemoprophylaxis on days 4 or 5, 2.2% in 831; and chemoprophylaxis on day 8, 14.1% in 99 (P < 0.0001). Spontaneous ICH expansion proportions at 24 hours substantially vary between chemoprophylaxis and non-chemoprophylaxis studies. Chemoprophylaxis should not be given within 3 days of injury for moderate-risk or high-risk ICH. Chemoprophylaxis is reasonable when low-risk patients have not developed ICH expansion within 48 hours post-injury. Chemoprophylaxis is also acceptable after day 3, when low-risk patients develop ICH expansion within 48 hours post-injury. In diffuse axonal injury patients who have not developed ICH within 72 hours, chemoprophylaxis is reasonable. Deep vein thrombosis proportions significantly increase when chemoprophylaxis is withheld for greater than 7 days.
Similar content being viewed by others
Abbreviations
- AIS:
-
Abbreviated injury score
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- DVT:
-
Deep vein thrombosis
- GCS:
-
Glasgow coma score
- ICH:
-
Intracranial hemorrhage
- LMWH:
-
Low molecular weight heparin
- MeSH:
-
Medical subject heading
- TBI:
-
Traumatic brain injury
References
Phelan HA. Pharmacologic venous thromboembolism prophylaxis after traumatic brain injury: a critical literature review. J Neurotrauma. 2012;29:1821–8.
Scales DC, Riva-Cambrin J, Wells D, Athaide V, Granton JT, Detsky AS. Prophylactic anticoagulation to prevent venous thromboembolism in traumatic intracranial hemorrhage: a decision analysis. Crit Care. 2010;14:R72.
Geerts WH, Code KI, Jay RM, Chen E, Szalai JP. A prospective study of venous thromboembolism after major trauma. N Engl J Med. 1994;331:1601–6.
Bee TK, Magnotti LJ, Croce MA, Maish GO, Minard G, Schroeppel TJ, et al. Necessity of repeat head CT and ICU monitoring in patients with minimal brain injury. J Trauma. 2009;66:1015–8.
Chang EF, Meeker M, Holland MC. Acute traumatic intraparenchymal hemorrhage: risk factors for progression in the early post-injury period. Neurosurgery. 2006;58:647–56. discussion 647-56.
Park HK, Joo WI, Chough CK, Cho CB, Lee KJ, Rha HK. The clinical efficacy of repeat brain computed tomography in patients with traumatic intracranial haemorrhage within 24 hours after blunt head injury. Br J Neurosurg. 2009;23:617–21.
Velmahos GC, Gervasini A, Petrovick L, Dorer DJ, Doran ME, Spaniolas K, et al. Routine repeat head CT for minimal head injury is unnecessary. J Trauma. 2006;60:494–9. discussion 499-501.
Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, et al. Guidelines for the management of severe traumatic brain injury. V. Deep vein thrombosis prophylaxis. J Neurotrauma. 2007;24:S32–6.
Sauaia A, Moore EE, Crebs JL, Maier RV, Hoyt DB, Shackford SR. Evidence level of individual studies: a proposed framework for surgical research. J Trauma Acute Care Surg. 2012;72:1484–90.
Kwiatt ME, Patel MS, Ross SE, Lachant MT, MacNew HG, Ochsner MG, et al. Is low-molecular-weight heparin safe for venous thromboembolism prophylaxis in patients with traumatic brain injury? A Western Trauma Association multicenter study. J Trauma Acute Care Surg. 2012;73:625–8.
Levy AS, Salottolo K, Bar-Or R, Offner P, Mains C, Sullivan M, et al. Pharmacologic thromboprophylaxis is a risk factor for hemorrhage progression in a subset of patients with traumatic brain injury. J Trauma. 2010;68:886–94.
Minshall CT, Eriksson EA, Leon SM, Doben AR, McKinzie BP, Fakhry SM. Safety and efficacy of heparin or enoxaparin prophylaxis in blunt trauma patients with a head abbreviated injury severity score >2. J Trauma. 2011;71:396–9. discussion 399-400.
Norwood SH, McAuley CE, Berne JD, Vallina VL, Kerns DB, Grahm TW, et al. Prospective evaluation of the safety of enoxaparin prophylaxis for venous thromboembolism in patients with intracranial hemorrhagic injuries. Arch Surg. 2002;137:696–701. discussion 701-2.
Norwood SH, Berne JD, Rowe SA, Villarreal DH, Ledlie JT. Early venous thromboembolism prophylaxis with enoxaparin in patients with blunt traumatic brain injury. J Trauma. 2008;65:1021–6. discussion 1026-7.
Saadeh Y, Gohil K, Bill C, Smith C, Morrison C, Mosher B, et al. Chemical venous thromboembolic prophylaxis is safe and effective for patients with traumatic brain injury when started 24 hours after the absence of hemorrhage progression on head CT. J Trauma Acute Care Surg. 2012;73:426–30.
Phelan HA, Eastman AL, Madden CJ, Aldy K, Berne JD, Norwood SH, et al. TBI risk stratification at presentation: a prospective study of the incidence and timing of radiographic worsening in the Parkland Protocol. J Trauma Acute Care Surg. 2012;73:S122–7.
Dudley RR, Aziz I, Bonnici A, Saluja RS, Lamoureux J, Kalmovitch B, et al. Early venous thromboembolic event prophylaxis in traumatic brain injury with low-molecular-weight heparin: risks and benefits. J Neurotrauma. 2010;27:2165–72.
Kim J, Gearhart MM, Zurick A, Zuccarello M, James L, Luchette FA. Preliminary report on the safety of heparin for deep venous thrombosis prophylaxis after severe head injury. J Trauma. 2002;53:38–42. discussion 43.
Koehler DM, Shipman J, Davidson MA, Guillamondegui O. Is early venous thromboembolism prophylaxis safe in trauma patients with intracranial hemorrhage. J Trauma. 2011;70:324–9.
Kurtoglu M, Yanar H, Bilsel Y, Guloglu R, Kizilirmak S, Buyukkurt D, et al. Venous thromboembolism prophylaxis after head and spinal trauma: intermittent pneumatic compression devices versus low molecular weight heparin. World J Surg. 2004;28:807–11.
Cothren CC, Smith WR, Moore EE, Morgan SJ. Utility of once-daily dose of low-molecular-weight heparin to prevent venous thromboembolism in multisystem trauma patients. World J Surg. 2007;31:98–104.
Depew AJ, Hu CK, Nguyen AC, Driessen N. Thromboembolic prophylaxis in blunt traumatic intracranial hemorrhage: a retrospective review. Am Surg. 2008;74:906–11.
Kleindienst A, Harvey HB, Mater E, Bronst J, Flack J, Herenz K, et al. Early antithrombotic prophylaxis with low molecular weight heparin in neurosurgery. Acta Neurochirurgica. 2003;145:1085–90. discussion 1090-1.
Norwood SH, McAuley CE, Berne JD, Vallina VL, Kerns DB, Grahm TW, et al. A potentially expanded role for enoxaparin in preventing venous thromboembolism in high risk blunt trauma patients. J Am College Surg. 2001;192:161–7.
Pahatouridis D, Alexiou GA, Zigouris A, Mihos E, Drosos D, Voulgaris S. Coagulopathy in moderate head injury. The role of early administration of low molecular weight heparin. Brain Injury. 2010;24:1189–92.
Phelan HA, Wolf SE, Norwood SH, Aldy K, Brakenridge SC, Eastman AL, et al. A randomized, double-blinded, placebo-controlled pilot trial of anticoagulation in low-risk traumatic brain injury: The Delayed Versus Early Enoxaparin Prophylaxis I (DEEP I) study. J Trauma Acute Care Surg. 2012;73:1434–41.
Salottolo K, Offner P, Levy AS, Mains CW, Slone DS, Bar-Or D. Interrupted pharmocologic thromboprophylaxis increases venous thromboembolism in traumatic brain injury. J Trauma. 2011;70:19–24. discussion 25-6.
Arnold JD, Dart BW, Barker DE, Maxwell RA, Burkholder HC, Mejia VA, et al. Gold Medal Forum Winner. Unfractionated heparin three times a day versus enoxaparin in the prevention of deep vein thrombosis in trauma patients. Am Surg. 2010;76:563–70.
Scudday T, Brasel K, Webb T, Codner P, Somberg L, Weigelt J, et al. Safety and efficacy of prophylactic anticoagulation in patients with traumatic brain injury. J Am College Surg. 2011;213:148–53. discussion 153-4.
Chelladurai Y, Stevens KA, Haut ER, Brotman DJ, Sharma R, Shermock KM, et al. Venous thromboembolism prophylaxis in patients with traumatic brain injury: a systematic review. F1000 Res. 2013;2:132.
Acknowledgements
The authors want to thank Ms Marina Hanes for copyediting the manuscript and Terry Lisko, librarian at St Elizabeth Health Center Jeghers Medical Index, for her assistance in obtaining hard copies and PDF versions of the relevant literature. No internal or external sources were obtained to write this manuscript.
International presentation
Accepted for presentation at the 73rd Annual Meeting of the American Association for the Surgery of Trauma and Clinical Congress of Acute Care Surgery in Philadelphia, PA, September, 2014.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Abdel-Aziz, H., Dunham, C.M., Malik, R.J. et al. Timing for deep vein thrombosis chemoprophylaxis in traumatic brain injury: an evidence-based review. Crit Care 19, 96 (2015). https://doi.org/10.1186/s13054-015-0814-z
Published:
DOI: https://doi.org/10.1186/s13054-015-0814-z