Abstract
Background
Iron deficiency has deleterious effects in patients with cardiopulmonary disease, independent of anemia. Low ferritin has been associated with increased mortality in patients undergoing cardiac surgery, but modern indices of iron deficiency need to be explored in this population.
Methods
We conducted a retrospective single-centre observational study of 250 adults in a UK academic tertiary hospital undergoing median sternotomy for non-emergent isolated aortic valve replacement. We characterised preoperative iron status using measurement of both plasma ferritin and soluble transferrin receptor (sTfR), and examined associations with clinical outcomes.
Results
Measurement of plasma sTfR gave a prevalence of iron deficiency of 22%. Patients with non-anemic iron deficiency had clinically significant prolongation of total hospital stay (mean increase 2.2 days; 95% CI: 0.5–3.9; P = 0.011) and stay within the cardiac intensive care unit (mean increase 1.3 days; 95% CI: 0.1–2.5; P = 0.039). There were no deaths. Defining iron deficiency as a plasma ferritin < 100 µg/L identified 60% of patients as iron deficient and did not predict length of stay. No significant associations with transfusion requirements were evident using either definition of iron deficiency.
Conclusions
These findings indicate that when defined using sTfR rather than ferritin, non-anemic iron deficiency predicts prolonged hospitalisation following surgical aortic valve replacement. Further studies are required to clarify the role of contemporary laboratory indices in the identification of preoperative iron deficiency in patients undergoing cardiac surgery. An interventional study of intravenous iron targeted at preoperative non-anemic iron deficiency is warranted.
Similar content being viewed by others
Background
Anemia is a well-established risk factor for adverse outcomes in patients undergoing cardiac surgery [1, 2] and in those with chronic heart failure (CHF) [3]. However, it is now recognised that iron deficiency (ID) is deleterious in CHF independent of anemia [4], and it has been demonstrated that intravenous (IV) iron supplementation in patients with CHF brings about substantial benefits not mediated by an effect on hemoglobin concentration [5,6,7]. Iron deficiency has a range of deleterious effects in cardiovascular disease (CVD) more generally [8], including acute coronary syndrome [9], idiopathic pulmonary arterial hypertension [10] and cyanotic congenital heart disease [11].
In a study in which bone marrow was sampled intraoperatively, 48% of patients of patients undergoing elective median sternotomy were found to have ID using bone marrow staining for iron [12], which is the gold-standard approach [13]. Remarkably, iron-deficient patients were more than twice as likely to have a normal preoperative hemoglobin concentration as they were to be anemic, highlighting that adequacy of body iron stores cannot be inferred from a normal preoperative hemoglobin concentration.
Studies exploring IV iron supplementation prior to cardiac surgery have typically focused on a transfusion-sparing effect [14,15,16]. Systematic reviews published in 2015 [17] and 2022 [18] have concluded that perioperative administration of IV iron in this setting is of uncertain benefit, whilst a recent observational study reported that IV iron therapy increased hemoglobin but had no effect on postoperative outcomes [19].
Iron deficiency in patients undergoing cardiac surgery is heterogeneous [20]. Various ID states with differing etiologies exist [13], including iron-deficiency anemia (IDA), non-anemic iron deficiency (NAID), inflammation-driven iron sequestration, and anemia of chronic disease. In some situations, IV iron might be helpful; in others, it might be ineffective or deleterious. A prerequisite for determining whether iron supplementation is beneficial is proper characterisation of ID in cardiac surgery patients including measurements of modern indices of iron homeostasis. Accordingly, we sought to characterise ID in a cohort undergoing surgical aortic valve replacement, from the previously published MAVRIC trial [21]. We hypothesised that ID would show different associations with postoperative outcomes in this setting depending on the index of iron status used to define it.
Methods
This was a retrospective, observational, cohort study. The MAVRIC trial recruited individuals undergoing median sternotomy for isolated AVR [21]. The trial explored whether manubrium-limited ministernotomy reduced blood transfusion requirements. Patients presenting with features requiring that they undergo surgery prior to discharge were classified as ‘urgent’; those admitted for a planned procedure were classified as ‘elective’. We measured indices of iron status using stored plasma samples. The primary objective was to determine the prevalence of preoperative ID in patients undergoing surgical AVR. The secondary objective was to examine associations with transfusion requirements and length of cardiac intensive care unit (CICU) and hospital length of stay (LoS).
Iron deficiency was defined according to two different criteria. First, using plasma ferritin < 100 µg/L (IDFer). Second, using plasma sTfR > 28.1 nmol/L (IDsTfR). The former was employed by an early study of IV iron supplementation in CHF [5], and has since been widely adopted in cardiopulmonary disease more generally [8]; the latter was derived from an early study of sTfR levels in healthy individuals [22]. sTfR has similarly been widely used in cardiopulmonary disease research [8]. Corresponding definitions for iron repletion (IR) were plasma ferritin ≥ 100 µg/L (IRFer), and plasma sTfR ≤ 28.1 nmol/L (IRsTfR). Anemia was defined according to World Health Organisation guidelines as [Hb] < 130 g/L in men and [Hb] < 120 g/L in women [23].
Aliquots of EDTA plasma, obtained by centrifugation and stored at − 80 °C, were assayed for C-reactive protein (CRP), ferritin and transferrin at a University Hospital clinical pathology laboratory. Serum samples were unavailable, so determination of transferrin saturation (TSat) was not possible. Plasma sTfR (Quantikine®, R&D Systems, Abingdon, UK), and hepcidin (Hepcidin 25 HS, DRG, Marburg, Germany) were analysed by enzyme-linked immunosorbent assay.
Data were analysed by an independent statistician. The mean and standard deviation were determined, and for non-normally distributed variables, the median and interquartile range. Fisher’s exact test was used to compare prevalences of ID and anemia. Logistic regression analysis of associations of ID dichotomised according to sTfR and ferritin was undertaken, including with LoS. All comparisons were 2-sided taking P < 0.05 to be statistically significant. Additionally, the data were explored using descriptive statistics. Analyses were performed using R 3.3.3 (The R Foundation) and SAS 9.4 (SAS Institute Inc).
Results
Preoperative blood samples were available for 250 patients, all of whom were included in the analysis. The mean (SD) age was 69.1 (8.9) years and 61% were male.
Prevalence of iron deficiency
The prevalence of IDFer and IDsTfR are shown in Table 1. The prevalence of ID was significantly higher using the ferritin-based definition compared with the sTfR-based definition (60% v. 22%, respectively; P < 0.0001, McNemar’s test). Most of this difference was accounted for by an excess of patients identified by a low plasma ferritin as having NAID.
Relationship between anemia and iron deficiency
Forty-seven patients (19%) were anemic. As shown in Table 2, the prevalence of ID was, as expected, significantly higher in anemic than non-anemic patients, irrespective of the definition used. Using sTfR to define ID identified 49% of anemic patients as iron deficient, but only 16% of non-anemic patients. Using ferritin to define ID identified 77% of anemic patients as iron deficient, as well as 56% of those who were non-anemic. Thus, ferritin identified the majority of both anemic and non-anemic patients as iron deficient.
The absolute difference in IDsTfR prevalence between anemic and non-anemic patients was 33% (49% minus 16%; 95% CI: 18–48; P < 0.0001); for IDFer the value was 21% (77% minus 56%; 95% CI: 7.0–35; P = 0.0084). However, using the IDFer definition identified a greater proportion of non-anemic patients as iron deficient than did IDsTfR. The absolute difference in prevalence of ID in non-anemic patients using the different definitions was 40% (56% minus 16%; 95% CI: 31–49; P < 0.0001). Thus, sTfR gave a considerably more conservative estimate of the prevalence of NAID than did ferritin.
Characteristics of patients according to iron status
Table 3 shows the characteristics of patients when split by iron status using sTfR or ferritin. Neither definition revealed a significant association of iron status with age or urgency of operation. Both gave significant differences in anemia prevalence, mean [Hb], transferrin, and hepcidin according to iron status; in each case the associations were similar: iron-deficient patients had lower [Hb], higher transferrin and lower hepcidin. However, the IDFer and IDsTfR definitions differed with respect to sex and CRP. Using ferritin identified more female patients as iron deficient; an sTfR-based definition showed no such association with sex. Patients identified as IRFer had significantly elevated CRP levels–consistent with greater inflammation–whereas no difference was seen in CRP levels between ID and IR groups using iron status determined using sTfR.
Red blood cell transfusion requirements
As shown in Table 4, iron status, however defined, was not associated with increased risk of receiving one or more units of red blood cells.
Postoperative hospital stay
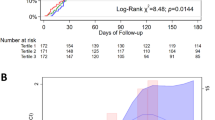
Iron deficiency identified by sTfR was associated with prolongation of hospital LoS from a mean (SD) of 6.3 (3.2) days in the IRsTfR group to 8.5 (10.4) days in the IDsTfR group (mean increase 2.2 days; 95% CI: 0.5–3.9; P = 0.011). IDsTfR patients also had a longer CICU LoS, a mean of 2.5 (8.6) days compared with 1.2 (0.9) days for IRsTfR patients (mean increase 1.3 days; 95% CI: 0.1–2.5; P = 0.039) (Table 5). Importantly, this association was not present in anemic patients and was absent when a ferritin-based definition of ID was used.
Discussion
In our cohort of patients undergoing surgical AVR, we found the prevalence of ID to be 60% using a conventional ferritin-based definition but only 22% using sTfR. Our main finding is that ID predicted significantly longer hospital and CICU stays. Interestingly, this was only true when using sTfR to identify ID; ferritin did not have this discriminatory value. Furthermore, the association with prolonged LoS in IDsTfR patients was unexpectedly confined to those who were not anemic, reinforcing that the absence of clinically significant ID cannot safely be inferred from the absence of anemia.
In a recent observational study of patients with severe aortic stenosis referred for AVR [24], the prevalence of ID using a ferritin and TSat-based definition was reported to be 53%, and the prevalence of anemia 20%, very similar figures to ours. Although sTfR was measured in that study, associations with LoS were not reported. Another study examined transcatheter aortic valve implantation [25] but iron indices were only assayed in anemic individuals, meaning that no conclusions can be drawn regarding NAID.
In a study that employed a complex algorithm for defining ID, including ferritin, TSat, CRP and sTfR, no association of preoperative ID with CICU LoS was seen, although iron-deficient patients did report significantly increased postoperative fatigue [14]. Conversely, a serum ferritin < 100 µg/L in isolation was associated with increased mortality, major cardiac and cerebrovascular events, transfusion, and prolonged hospital stay in one randomised controlled trial (RCT) [26].
That we were able to identify associations with sTfR but not ferritin in a smaller, more homogenous group might imply that sTfR is superior to ferritin at identifying clinically relevant ID, at least in part because sTfR is not influenced by inflammation [27]. Alternatively, it may be that patients undergoing surgical AVR differ from a mixed cardiac surgical population. None of our patients died, and none underwent simultaneous surgical revascularisation. Differing levels of subclinical inflammation in patients undergoing other cardiac surgical procedures–particularly coronary artery bypass grafting–may be important.
Our study has several limitations. First, it was not possible to measure TSat owing to the absence of serum samples. Second, we were limited to the outcome data originally collected in the MAVRIC trial. Third, because MAVRIC was a 270-patient single centre trial, the present work may have been underpowered to detect other clinically significant associations.
A major challenge when investigating the interplay between iron homeostasis and CVD is the manner in which ID is defined. Whilst the definition based on ferritin and TSat that has generally been adopted in CVD [5] certainly identifies a group in whom there is a net benefit from IV iron therapy [6], it must be noted that it is arbitrary and does not have a firm pathobiological basis. Consequently, this definition may miss a group of patients who would benefit from IV iron therapy, whilst simultaneously including some individuals who derive no benefit or may be harmed.
Our data suggest that the use of sTfR avoids misclassifying patients as iron replete who in fact have inflammation-driven elevation of ferritin [27], whilst simultaneously not falsely labelling as iron deficient those healthy individuals with a ferritin < 100 µg/L, which may still be consistent with healthy iron stores and biologically available iron [28]. In support of this possibility, levels of the master iron-regulatory hormone hepcidin were similar in our iron-deficient patients whether identified as such by a low ferritin or high sTfR. Hepcidin is ordinarily heavily suppressed by absolute ID, leading to increased iron uptake from the gut and its liberation from reticuloendothelial stores. Elevated levels of hepcidin seen with infection and inflammation reflect a mechanism to sequester iron and reduce its bioavailability to pathogens [29]. Patients in the present study identified as iron replete based on ferritin ≥ 100 µg/L had hepcidin levels ~ 50% higher than those identified as iron replete based on sTfR, arguing against any great additional diagnostic value of hepcidin measurement in this setting.
Conclusion
We have found a novel association between NAID and prolonged hospital and CICU LoS in patients undergoing surgical AVR. Whilst it is not possible from the present study to determine the underlying mechanisms, our findings clearly identify elevated sTfR in non-anemic cardiac surgery patients as a treatable trait that might improve postoperative recovery and shorten hospital stay. They also support a future RCT of iron supplementation as a targeted therapy in this group, rather than an indiscriminate intervention aimed primarily at reducing perioperative blood transfusion requirements.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AVR:
-
Aortic valve replacement
- CHF:
-
Chronic heart failure
- CICU:
-
Cardiac intensive care unit
- CRP:
-
C-reactive protein
- CVD:
-
Cardiovascular disease
- ID:
-
Iron deficiency
- IDA:
-
Iron-deficiency anemia
- IR:
-
Iron repletion
- IV:
-
Intravenous
- LoS:
-
Length of stay
- NAID:
-
Non-anemic iron deficiency
- NHS:
-
National health service
- RCT:
-
Randomised controlled trial
- SD:
-
Standard deviation
- sTfR:
-
Soluble transferrin receptor
- TSat:
-
Transferrin saturation
References
Miceli A, Romeo F, Glauber M, de Siena PM, Caputo M, Angelini GD. Preoperative anemia increases mortality and postoperative morbidity after cardiac surgery. J Cardiothorac Surg. 2014;9:137.
Padmanabhan H, Siau K, Curtis J, Ng A, Menon S, Luckraz H, et al. Preoperative anemia and outcomes in cardiovascular surgery: systematic review and meta-analysis. Ann Thorac Surg. 2019;108(6):1840–8.
Groenveld HF, Januzzi JL, Damman K, van Wijngaarden J, Hillege HL, van Veldhuisen DJ, et al. Anemia and mortality in heart failure patients a systematic review and meta-analysis. J Am Coll Cardiol. 2008;52(10):818–27.
Klip IT, Comin-Colet J, Voors AA, Ponikowski P, Enjuanes C, Banasiak W, et al. Iron deficiency in chronic heart failure: an international pooled analysis. Am Heart J. 2013;165(4):575–82.
Okonko DO, Grzeslo A, Witkowski T, Mandal AK, Slater RM, Roughton M, et al. Effect of intravenous iron sucrose on exercise tolerance in anemic and nonanemic patients with symptomatic chronic heart failure and iron deficiency FERRIC-HF: a randomized, controlled, observer-blinded trial. J Am Coll Cardiol. 2008;51(2):103–12.
Anker SD, Comin-Colet J, Filippatos G, Willenheimer R, Dickstein K, Drexler H, et al. Ferric carboxymaltose in patients with heart failure and iron deficiency. N Engl J Med. 2009;361(25):2436–48.
Ponikowski P, van Veldhuisen DJ, Comin-Colet J, Ertl G, Komajda M, Mareev V, et al. Beneficial effects of long-term intravenous iron therapy with ferric carboxymaltose in patients with symptomatic heart failure and iron deficiency. Eur Heart J. 2015;36(11):657–68.
von Haehling S, Jankowska EA, van Veldhuisen DJ, Ponikowski P, Anker SD. Iron deficiency and cardiovascular disease. Nat Rev Cardiol. 2015;12(11):659–69.
Reinhold J, Papadopoulou C, Baral R, Vassiliou VS. Iron deficiency for prognosis in acute coronary syndrome - A systematic review and meta-analysis. Int J Cardiol. 2021;328:46–54.
Viethen T, Gerhardt F, Dumitrescu D, Knoop-Busch S, Ten Freyhaus H, Rudolph TK, et al. Ferric carboxymaltose improves exercise capacity and quality of life in patients with pulmonary arterial hypertension and iron deficiency: A pilot study. Int J Cardiol. 2014;175(2):233–9.
Tay EL, Peset A, Papaphylactou M, Inuzuka R, Alonso-Gonzalez R, Giannakoulas G, et al. Replacement therapy for iron deficiency improves exercise capacity and quality of life in patients with cyanotic congenital heart disease and/or the Eisenmenger syndrome. Int J Cardiol. 2011;151(3):307–12.
Jankowska EA, Wojtas K, Kasztura M, Mazur G, Butrym A, Kalicinska E, et al. Bone marrow iron depletion is common in patients with coronary artery disease. Int J Cardiol. 2014;182C:517–22.
Pasricha SR, Tye-Din J, Muckenthaler MU, Swinkels DW. Iron deficiency. Lancet (London, England). 2021;397(10270):233–48.
Piednoir P, Allou N, Driss F, Longrois D, Philip I, Beaumont C, et al. Preoperative iron deficiency increases transfusion requirements and fatigue in cardiac surgery patients: a prospective observational study. Eur J Anaesthesiol. 2011;28(11):796–801.
Cladellas M, Farre N, Comin-Colet J, Gomez M, Merono O, Bosch MA, et al. Effects of preoperative intravenous erythropoietin plus iron on outcome in anemic patients after cardiac valve replacement. Am J Cardiol. 2012;110(7):1021–6.
Padmanabhan H, Siau K, Nevill AM, Morgan I, Cotton J, Ng A, et al. Intravenous iron does not effectively correct preoperative anaemia in cardiac surgery: a pilot randomized controlled trial. Interact Cardiovasc Thorac Surg. 2019;28(3):447–54.
Hogan M, Klein AA, Richards T. The impact of anaemia and intravenous iron replacement therapy on outcomes in cardiac surgery. European J Cardio-Thoracic Surg: Off J European Assoc Cardio-Thoracic Surg. 2015;47(2):218–26.
Yang SS, Al Kharusi L, Gosselin A, Chirico A, Baradari PG, Cameron MJ. Iron supplementation for patients undergoing cardiac surgery: a systematic review and meta-analysis of randomized controlled trials. Can J Anaesth. 2022;69(1):129–39.
Klein AA, Chau M, Yeates JA, Collier T, Evans C, Agarwal S, et al. Preoperative intravenous iron before cardiac surgery: a prospective multicentre feasibility study. Br J Anaesth. 2020;124(3):243–50.
Hung M, Ortmann E, Besser M, Martin-Cabrera P, Richards T, Ghosh M, et al. A prospective observational cohort study to identify the causes of anaemia and association with outcome in cardiac surgical patients. Heart (British Cardiac Society). 2015;101(2):107–12.
Hancock HC, Maier RH, Kasim AS, Mason JM, Murphy GJ, Goodwin AT, et al. Mini-sternotomy versus conventional sternotomy for aortic valve replacement. J Am Coll Cardiol. 2019;73(19):2491–2.
Allen J, Backstrom KR, Cooper JA, Cooper MC, Detwiler TC, Essex DW, et al. Measurement of soluble transferrin receptor in serum of healthy adults. Clin Chem. 1998;44(1):35–9.
WHO (2011) Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and mineral nutrition information system. (WHO/NMH/NHD/MNM/11.1). Geneva: World Health Organization.
Kvaslerud AB, Hussain AI, Auensen A, Ueland T, Michelsen AE, Pettersen KI, et al. Prevalence and prognostic implication of iron deficiency and anaemia in patients with severe aortic stenosis. Open heart. 2018;5(2): e000901.
Rheude T, Pellegrini C, Michel J, Trenkwalder T, Mayr NP, Kessler T, et al. Prognostic impact of anemia and iron-deficiency anemia in a contemporary cohort of patients undergoing transcatheter aortic valve implantation. Int J Cardiol. 2017;244:93–9.
Rossler J, Schoenrath F, Seifert B, Kaserer A, Spahn GH, Falk V, et al. Iron deficiency is associated with higher mortality in patients undergoing cardiac surgery: a prospective study. Br J Anaesth. 2020;124(1):25–34.
Skikne BS, Punnonen K, Caldron PH, Bennett MT, Rehu M, Gasior GH, et al. Improved differential diagnosis of anemia of chronic disease and iron deficiency anemia: a prospective multicenter evaluation of soluble transferrin receptor and the sTfR/log ferritin index. Am J Hematol. 2011;86(11):923–7.
Finch CA, Bellotti V, Stray S, Lipschitz DA, Cook JD, Pippard MJ, et al. Plasma ferritin determination as a diagnostic tool. West J Med. 1986;145(5):657–63.
Ganz T, Nemeth E. Iron homeostasis in host defence and inflammation. Nat Rev Immunol. 2015;15(8):500–10.
Acknowledgements
Not applicable.
Funding
MCF was supported by a British Heart Foundation Clinical Research Training Fellowship (FS/14/48/30828); KLD by the Dunhill Medical Trust (R178/1110); and MSS by the South Cleveland Cardiothoracic Charity. Manubrium-limited ministernotomy versus conventional sternotomy for aortic valve replacement: A randomised controlled trial (MAVRIC), was funded by the Research for Patient Benefit Programme of the National Institute for Health Research (PB-PG-1112–29035). The funding sources had no role in the design of the study, collection of data, its analysis or interpretation, nor in the decision to publish the final manuscript.
Author information
Authors and Affiliations
Contributions
Conception and design: EFA, KLD, MCF, DAH, HCH, RHM, AJM, PAR, MSS; collected Data: EFA, MCF, DAH, MSS; performed assays: MCF, DAH, MSS; analysed data: EFA, ASK, RHM, MSS; interpreted data: All authors; wrote first draft: MCF; All authors revised and approved final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was given by the NHS East of Scotland Research Ethics Service (17/ES/0151). The study was sponsored by South Tees Hospitals NHS Foundation Trust and conducted in accordance with the principles of the declaration of Helsinki. All participants gave written informed consent.
Consent for publication
Not applicable.
Competing interests
PAR has received grant funding from Vifor Pharma for basic science studies of iron biology. MSS has received a travel grant from Pharmacosmos. The remaining authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Frise, M.C., Holdsworth, D.A., Sandhu, M.S. et al. Non-anemic iron deficiency predicts prolonged hospitalisation following surgical aortic valve replacement: a single-centre retrospective study. J Cardiothorac Surg 17, 157 (2022). https://doi.org/10.1186/s13019-022-01897-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-022-01897-5