Abstract
Background
Extended reality (XR), including virtual reality, augmented reality (AR), and mixed reality, has been used to help achieve accurate acetabular cup placement in total hip arthroplasty (THA). This study aimed to compare the differences between XR-assisted and conventional THA.
Methods
In this systematic review and meta-analysis, electronic databases including PubMed, Embase, Web of Science, Cochrane Central Register of Controlled Trials (CENTRAL), and clinicaltrials.gov were searched for studies from inception to September 10, 2023. The outcomes were accuracy of inclination and anteversion, duration of surgery, and intraoperative blood loss. Meta-analysis was performed using Review Manager 5.4 software.
Results
A total of five studies with 396 patients were included in our study. The pooled results indicated AR-assisted THA had better accuracy of inclination and anteversion than conventional THA (SMD = − 0.51, 95% CI [− 0.96 to − 0.07], P = 0.02; SMD = − 0.96, 95% CI [− 1.19 to − 0.72], P < 0.00001), but duration of surgery and intraoperative blood loss were similar in the two groups.
Conclusion
This systematic review and meta-analysis found that AR-assisted THA had better accuracy of inclination and anteversion than conventional THA, but the duration of surgery and intraoperative blood loss were similar in the two groups. Based on the pooled results, we suggested that AR can provide more precise acetabular cup placement than conventional methods in THA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Total hip arthroplasty (THA) is the main and effective surgical method for the treatment of advanced hip osteoarthritis, osteonecrosis, and rheumatoid arthritis [1]. The acetabular cup position is very important for maximizing the hip range of motion and minimizing impingement, dislocation, liner fracture, and long-term wear [2,3,4]. Good acetabular anteversion and inclination angle is the key to the success of THA. Due to pelvic movement, complex anatomy, and varying surgeon experience, it is difficult and error-prone to use conventional surgical techniques to accurately and consistently locate the acetabular cup [5]. Cup malposition is associated with multiple postoperative complications, such as impingement, dislocation, liner fracture, and the need for revision surgery, burdening the patient [6,7,8]. Therefore, to minimize the risk of dislocation, the "safe zone" of the position of the acetabular prosthesis described by Lewinnek et al. has been used as a guide [9].
Many techniques can help achieve accurate component position, including intraoperative radiographs [10], fluoroscopy [11], computer-assisted navigation systems [12], and robotics [13]. However, these solutions proposed have substantial limitations, including X-ray exposure to the patient and personnel, lack of accuracy due to parallax or operator error with fluoroscopy, cost, or change in pelvis position during the operation. To resolve these issues, we are witnessing increasing use of augmented reality (AR), virtual reality (VR), and new mixed reality (MR), which include both AR and VR, to assist in THA. VR technology generally uses a headset, blocking out visual stimuli from the real world. AR allows users to see the real world but overlays virtual elements. MR combines the two, including aspects of both the real and virtual worlds [14, 15]. Extended reality (XR) is the umbrella term that refers to these three different types of technology [16]. Generally, XR-assisted THA provides accurate and reproducible component positioning and balancing of soft tissue. These benefits may contribute to longer implant survival and a reduced need for revision surgery [17,18,19]. However, some scholars do not agree with these results [20].
Both XR-assisted and conventional methods of THA have been compared in many clinical trials; however, most of these studies have small sample sizes. XR-assisted THA requires a larger operating space, wider exposure, and longer operation time, which may increase the probability of postoperative infection. The choice between XR-assisted and conventional approaches for THA remains controversial. To our knowledge, no systematic review and meta-analysis has compared the safety and efficacy between XR-assisted and conventional methods of THA. Thus, this systematic review and meta-analysis was designed to compare the differences between XR-assisted and conventional THA, to gain some theoretical insights that may guide clinical practice.
Methods
This systematic review and meta-analysis was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [21]. The protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42022364486).
Search strategy and selection criteria
We searched PubMed, Embase, Cochrane Central Register of Controlled Trials (CENTRAL), Web of Science, and clinicaltrials.gov electronic databases from inception to September 10, 2023, with restriction to the English language. We used the following search terms in each database: (virtual reality OR augmented reality OR mixed reality) AND total hip arthroplasty. To achieve the highest sensitivity, we used a combination of keywords and indexed terms (e.g., PubMed Medical Subject Headings). We also examined the reference lists of each comparative study and reviews to identify additional relevant studies. The detailed search strategy is available in the Supplement.
The criteria for inclusion were research articles studying VR-, AR-, or MR-assisted compared to conventional THA and reporting on the accuracy of inclination and anteversion, duration of surgery, and intraoperative blood loss. Two investigators (SS and RW) independently screened all identified articles and considered the potential eligibility of each of the titles and abstracts. Full-text articles were obtained unless both reviewers decided that an abstract was ineligible. Disagreements between reviewers were discussed and resolved by consensus.
Data extraction and quality assessment
Two investigators (SS and RW) independently extracted data from all included studies using a data extraction form. Any disagreements between them were solved by a discussion. The included studies were evaluated for authors, year of publication, country, study design, number of patients, age, sex, surgical approach, type of XR, the accuracy of inclination and anteversion, duration of surgery, and intraoperative blood loss. If data were not presented in the original article, corresponding authors were contacted to acquire the missing data, although no responses were received.
Two investigators (SS and RW) evaluated the quality of the included studies independently, utilizing the Risk of Bias tool of the Cochrane Library [22, 23]. Funnel plots were used to assess publication bias for any of the outcomes, and a publication bias was considered present if an asymmetry in the funnel plot was found. Any disagreements between the two reviewers were resolved by a discussion.
Statistical analysis
For continuous outcomes, including the accuracy of inclination and anteversion, duration of surgery, and intraoperative blood loss, the mean difference (MD) and associated 95% confidence interval (CI) were used to perform estimates for each study. If different measurement methods or units were used for the same index and the mean values were significantly different, standardized mean difference (SMD) with 95% CI was used. We utilized the random-effect or fixed-effect model to analyze the pooled results, respectively, when significant heterogeneity (P < 0.10; I2 > 50%) appeared or not. The sensitivity analysis was performed to evaluate the reliability of the pooled results by removing some studies from analyzed studies in each analysis, and subgroup analysis was conducted to obtain more specific conclusions. All statistical analyses were performed using the Review Manager software (version 5.4, Cochrane Collaboration, Oxford, UK). A P-value < 0.05 was considered significant.
Results
Study identification
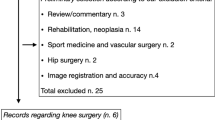
As shown in Fig. 1, there were 219 studies yielded from the five electronic databases. After removing 110 duplicates, 178 studies remained. After screening the titles and abstracts and reading full texts, 173 studies were excluded. Thus, five studies published from 2019 to 2023 were finally included in the study, including three randomized, controlled trials (RCTs) [20, 24, 25] and two retrospective cohort studies [26, 27].
Study characteristics and quality assessment
A total of five studies enrolled 396 patients with 200 undergoing AR-assisted THA and 196 undergoing conventional THA. The type of XR used only included AR, without VR and MR. The detailed data of the included studies are summarized in Table 1. The risk of bias was low for most of the domains. Two studies were rated to have high risk due to the absence of randomization [26, 27]. The result of the risk of bias is summarized in Fig. 2. There was no evidence of publication bias after the assessment of the funnel plots (Additional file 1: Figures S1, S2, S3, and S4 in the Supplement).
Accuracy of inclination
All five studies reported accuracy of inclination and were included in the meta-analysis [20, 24,25,26,27]. The results showed that AR-assisted THA had better accuracy of inclination than conventional THA (SMD = − 0.51, 95% CI [− 0.96 to − 0.07], P = 0.02) (Fig. 3). Because of the existence of heterogeneity (P = 00009, I2 = 78%), the sensitivity analysis was performed. However, we found that heterogeneity was still high after excluding studies one by one. We conducted subgroup analyses by dividing the studies into the RCTs subgroup and the retrospective cohort studies subgroup. In the RCTs subgroup, due to the significant heterogeneity (P = 0.002, I2 = 84%), the sensitivity analysis was performed and indicated that the heterogeneity came from one study [25]. Therefore, we performed analysis again after removing the study, and the results revealed that AR-assisted THA had better accuracy of inclination than conventional THA (SMD = − 0.93, 95% CI [− 1.32 to − 0.54], P < 0.00001) in the RCTs subgroup, while no significant difference in the retrospective cohort studies subgroup (SMD = − 0.45, 95% CI [− 1.23 to 0.33], P = 0.26) (Additional file 1: Figure S5). It is worth noting that after excluding this study [25], only two RCTs in the RCTs subgroup were included in the analysis.
Accuracy of anteversion
All five studies reported accuracy of anteversion and were included in the meta-analysis [20, 24,25,26,27]. The pooled results showed that AR-assisted THA had better accuracy of anteversion than conventional THA (SMD = − 0.72, 95% CI [− 1.19 to − 0.25], P = 0.003) (Fig. 4A). Due to the heterogeneity (P = 0.0005, I2 = 80%), the sensitivity analysis was performed and indicated that the heterogeneity came from one study [26]. Therefore, we performed analysis again after removing the study, and the results also revealed that AR-assisted THA had better accuracy of anteversion than conventional THA (SMD = − 0.96, 95% CI [− 1.19 to − 0.72], P < 0.00001) (Fig. 4B). The subgroup analyses showed that AR-assisted THA had better accuracy of anteversion than conventional THA (SMD = − 0.82, 95% CI [− 1.12 to − 0.51], P < 0.00001) in the RCTs subgroup, while no significant difference in the retrospective cohort studies subgroup (SMD = − 0.64, 95% CI [− 2.00 to 0.71], P = 0.35) (Additional file 1: Figure S6).
Duration of surgery
All five studies reported duration of surgery and were included in the meta-analysis [20, 24,25,26,27]. The results showed that no significant differences were found between the two groups (MD = 0.21, 95% CI [− 1.37 to 1.79], P = 0.79) (Fig. 5). The subgroup analyses also showed that there were no significant differences between the two groups in the RCTs subgroup and in the retrospective cohort studies subgroup (Additional file 1: Figure S7).
Intraoperative blood loss
There were three studies reporting intraoperative blood loss and included in the meta-analysis [20, 25, 27]. The pooled results showed that no significant differences were found between the two groups (MD = − 6.72, 95% CI [− 27.47 to 14.02], P = 0.53) (Fig. 6).
Discussion
This systematic review and meta-analysis included five studies that assessed 396 patients and compared the accuracy of inclination and anteversion, duration of surgery, and intraoperative blood loss between AR-assisted and conventional THA groups. The pooled results revealed that AR-assisted THA had better accuracy of inclination and anteversion, but the duration of surgery and intraoperative blood loss were similar in the two groups. Our study included three RCTs and two retrospective cohort studies, and the analysis showed that the heterogeneity was high. Therefore, we carried out sensitivity analysis and subgroup analysis and confirmed the reliability of the results. To our best knowledge, this is the first systematic review and meta-analysis to show the differences between AR-assisted and conventional THA.
Accurate and appropriate acetabular cup position is one of the key factors for successful THA [2,3,4]. At present, the acetabular cup is mainly placed at a fixed angle, such as inclination of 40 degrees, anteversion of 15 or 20 degrees, or in the Lewinnek safe zone [28]. However, some scholars believe that the ideal cup positioning angle of each patient is different [28, 29], and it is necessary to develop a specific cup location for each patient to avoid complications after THA. This view is gradually recognized. However, there are challenges in conventional THA to achieve this goal of personalized and precise treatment. Therefore, XR-assisted THA, including AR, has been developed and received people's attention [19]. A systematic review and meta-analysis showed that XR training had better accuracy of inclination and shorter surgical duration than conventional methods in THA on the models or cadavers [30]. At present, several human clinical trials of AR-assisted THA have been published, but the reported results are controversial. So, we carried out this systematic review and meta-analysis and found that AR-assisted THA had better accuracy of inclination and anteversion than conventional THA in human trials. Since XR-assisted THA needs to expose fixed anatomical landmarks to register during surgery, people are worried that this process will lead to an increase in the duration of surgery and intraoperative blood loss. Our study found that there was no difference between AR-assisted and conventional THA in terms of duration of surgery and intraoperative blood loss. However, these studies mainly reported data on the accuracy of acetabular cup position, with little data on long-term postoperative clinical function and postoperative complications. Only one study [24] reported the Hip Disability and Osteoarthritis Outcome Scores and complications at 6 months after operation, and there was no difference between the two groups. Therefore, it is unknown whether the improvement in imaging data observed at present will bring benefits to the medium- and long-term clinical outcomes of patients after operation. High-quality long-term follow-up RCTs are also needed to verify.
Currently, surgical robots, fluoroscopy, and intraoperative computer navigation are increasingly used to improve the accuracy of THA [10,11,12,13]. However, intraoperative X-ray imaging during fluoroscopy cannot provide three-dimensional images, consumes operating room space, and increases radiation exposure to patients and surgeons. Moreover, computer navigation and surgical robots may distract surgeons from the surgical site through computer screens [31]. In addition, fluoroscopy, computer-assisted navigation, and surgical robots usually need to be equipped with large equipment and additional personnel in the operating room, which will also bring corresponding problems. XR can visually integrate data into diagnosis and surgery through a pair of glasses, such as HoloLens, without the need for additional imaging and equipment [31]. In the study, we only found AR-assisted THA, and there was no intraoperative navigation based on MR. MR is a new digital holographic imaging technology that combines the advantages of VR and AR. By introducing the real scene information into the virtual environment, the interactive feedback information cycle is established among the virtual world, the real world, and the users to enhance the authenticity of the user experience. Its key is to interact with the real world, to obtain information in time, and to interact seamlessly with the users of the real world and virtual models [14, 15]. Perhaps in the near future, the development of a portable navigation system based on MR can provide us with a more practical surgical navigation system.
Some deficiencies should be considered when generalizing the conclusion of this study. Firstly, the sample size of our study is small, and both RCTs and non-RCTs were included due to a lack of data, which adds to potential bias to this study. Secondly, because all the included studies were published in English, the language bias was difficult to avoid. Thirdly, although we have performed sensitivity and subgroup analyses, significant heterogeneity remained between studies. Further research is needed to minimize heterogeneity and improve statistical power.
Conclusion
This systematic review and meta-analysis found that AR-assisted THA had better accuracy of inclination and anteversion than conventional THA, but the duration of surgery and intraoperative blood loss were similar in the two groups. Based on the pooled results, we suggested that AR can provide more precise acetabular cup placement than conventional methods in THA.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- THA:
-
Total hip arthroplasty
- AR:
-
Augmented reality
- VR:
-
Virtual reality
- MR:
-
Mixed reality
- XR:
-
Extended reality
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROSPERO:
-
International Prospective Register of Systematic Reviews
- CENTRAL:
-
Cochrane Central Register of Controlled Trials
- MD:
-
Mean difference
- CI:
-
Confidence interval
- SMD:
-
Standardized mean difference
- RCTs:
-
Randomized, controlled trials
References
Konan S, Duncan CP. Total hip arthroplasty in patients with neuromuscular imbalance. Bone Joint J. 2018;100B(1 Supple A):17–21.
D’Lima DD, Urquhart AG, Buehler KO, Walker RH, Colwell CW Jr. The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am. 2000;82(3):315–21.
Murayama T, Ohnishi H, Mori T, Okazaki Y, Sujita K, Sakai A. A novel non-invasive mechanical technique of cup and stem placement and leg length adjustment in total hip arthroplasty for dysplastic hips. Int Orthop. 2015;39(6):1057–64.
Yamaguchi M, Akisue T, Bauer TW, Hashimoto Y. The spatial location of impingement in total hip arthroplasty. J Arthroplasty. 2000;15(3):305–13.
Gonzalez Della Valle A, Shanaghan K, Benson JR, Carroll K, Cross M, Mclawhorn A, et al. Pelvic pitch and roll during total hip arthroplasty performed through a posterolateral approach. A potential source of error in free-hand cup positioning. Int Orthop 2019; 43(8): 1823–9.
Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplast. 1998;13(5):530–4.
Migliorini F, Eschweiler J, Trivellas A, Rath B, Driessen A, Tingart M, et al. Implant positioning among the surgical approaches for total hip arthroplasty: a Bayesian network meta-analysis. Arch Orthop Trauma Surg. 2020;140(8):1115–24.
Widmer KH, Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22(4):815–21.
Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60(2):217–20.
Ezzet KA, McCauley JC. Use of intraoperative X-rays to optimize component position and leg length during total hip arthroplasty. J Arthroplast. 2014;29(3):580–5.
James CR, Peterson BE, Crim JR, Cook JL, Crist BD. The use of fluoroscopy during direct anterior hip arthroplasty: powerful or misleading? J Arthroplast. 2018;33(6):1775–9.
Wasterlain AS, Buza JA, Thakkar SC, Schwarzkopf R, Vigdorchik J. Navigation and robotics in total hip arthroplasty. JBJS Rev. 2017;5(3):e2.
Singh V, Realyvasquez J, Simcox T, Rozell JC, Schwarzkopf R, Davidovitch RI. Robotics versus navigation versus conventional total hip arthroplasty: does the use of technology yield superior outcomes? J Arthroplast. 2021;36(8):2801–7.
Lei PF, Su SL, Kong LY, Wang CG, Zhong D, Hu YH. Mixed reality combined with three-dimensional printing technology in total hip arthroplasty: an updated review with a preliminary case presentation. Orthop Surg. 2019;11(5):914–20.
Su S, Lei P, Wang C, Gao F, Zhong D, Hu Y. Mixed reality technology in total knee arthroplasty: an updated review with a preliminary case report. Front Surg. 2022;9:804029.
Kaplan AD, Cruit J, Endsley M, Beers SM, Sawyer BD, Hancock PA. The effects of virtual reality, augmented reality, and mixed reality as training enhancement methods: a meta-analysis. Hum Factors. 2021;63(4):706–26.
Alexander C, Loeb AE, Fotouhi J, Navab N, Armand M, Khanuja HS. Augmented reality for acetabular component placement in direct anterior total hip arthroplasty. J Arthroplast. 2020;35(6):1636-41.e3.
Logishetty K, Western L, Morgan R, Iranpour F, Cobb JP, Auvinet E. Can an augmented reality headset improve accuracy of acetabular cup orientation in simulated THA? A randomized trial. Clin Orthop Relat Res. 2019;477(5):1190–9.
Ogawa H, Hasegawa S, Tsukada S, Matsubara M. A pilot study of augmented reality technology applied to the acetabular cup placement during total hip arthroplasty. J Arthroplast. 2018;33(6):1833–7.
Ogawa H, Kurosaka K, Sato A, Hirasawa N, Matsubara M, Tsukada S. Does an augmented reality-based portable navigation system improve the accuracy of acetabular component orientation during THA? A randomized controlled trial. Clin Orthop Relat Res. 2020;478(5):935–43.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev 2019;10: ED000142.
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Tanino H, Mitsutake R, Takagi K, Ito H. Does a commercially available augmented reality-based portable hip navigation system improve cup positioning during THA compared with the conventional technique? A randomized controlled study. Clin Orthop Relat Res. 2023;10:17.
Kurosaka K, Ogawa H, Hirasawa N, Saito M, Nakayama T, Tsukada S. Does augmented reality-based portable navigation improve the accuracy of cup placement in THA compared with accelerometer-based portable navigation? A randomized controlled trial. Clin Orthop Relat Res. 2023;481(8):1515–23.
Fujita M, Hayashi S, Kuroda Y, Nakano N, Maeda T, Matsushita T, et al. Accuracy comparison of cup positioning during total hip arthroplasty using hip align and AR-hip in the supine position. Arch Orthop Trauma Surg. 2023;21:1–7.
Tsukada S, Ogawa H, Hirasawa N, Nishino M, Aoyama H, Kurosaka K. Augmented reality- vs accelerometer-based portable navigation system to improve the accuracy of acetabular cup placement during total hip arthroplasty in the lateral decubitus position. J Arthroplast. 2022;37(3):488–94.
Abdel MP, von Roth P, Jennings MT, Hanssen AD, Pagnano MW. What safe zone? The vast majority of dislocated THAs are within the Lewinnek safe zone for acetabular component position. Clin Orthop Relat Res. 2016;474(2):386–91.
Vigdorchik J, Eftekhary N, Elbuluk A, Abdel MP, Buckland AJ, Schwarzkopf RS, et al. Evaluation of the spine is critical in the workup of recurrent instability after total hip arthroplasty. Bone Joint J. 2019;101-B(7):817–23.
Su S, Wang R, Zhou R, Chen Z, Zhou F. The effectiveness of virtual reality, augmented reality, and mixed reality training in total hip arthroplasty: a systematic review and meta-analysis. J Orthop Surg Res. 2023;18(1):121.
Shaikh HJF, Hasan SS, Woo JJ, Lavoie-Gagne O, Long WJ, Ramkumar PN. Exposure to extended reality and artificial intelligence-based manifestations: a primer on the future of hip and knee arthroplasty. J Arthroplasty. 2023;38(10):2096–104.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81971160) and the Peking University Third Hospital Clinical Key Project Fund (No. BYSYZHKC2021106).
Author information
Authors and Affiliations
Contributions
FZ and SS conceived the original ideas of this manuscript. SS and YZ screened out eligible studies separately. SS, YZ, RW, ZC, and FZ discussed the controversial parts of the literature screening and quality evaluation. SS and YZ completed data collection, analysis, and finished the manuscript. FZ and YZ supervised the entire process and revised the manuscript. All authors have read and approved the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors report no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Database search algorithms, funnel plots to assess publication bias, and forest plots of the subgroup analyses.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Su, S., Wang, R., Chen, Z. et al. Augmented reality-assisted versus conventional total hip arthroplasty: a systematic review and meta-analysis. J Orthop Surg Res 18, 920 (2023). https://doi.org/10.1186/s13018-023-04421-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-04421-0