Abstract
Background
This study aimed to examine associations between haemoglobin A1c (HbA1c) levels over time and all-cause and cause-specific mortality in middle-aged and older Koreans.
Methods
Using 16 years of follow-up data from the Korean Genome and Epidemiology Study, we analysed 9294 individuals aged 40–69 years with no history of cardiovascular disease (CVD) or cancer. Participants were divided into a known diabetes group and five groups categorized by HbA1c levels (< 5.0%, 5.0–5.4%, 5.5–5.9%, 6.0–6.4%, and ≥ 6.5%). Hazard ratios (HRs) for all-cause and cause-specific mortality associated with HbA1c levels were calculated using a conventional and a time-dependent Cox proportional hazards model. Restricted cubic spline models were fitted to investigate the relationship between continuous HbA1c levels and mortality among people without known diabetes. Subgroup analyses were performed for age, sex, smoking, hypertension, liver diseases, and red blood cell counts.
Results
During a median follow-up period of 15.7 years, there were 944 deaths, including 185 deaths from CVD, 359 from cancer, and 125 from all external causes. Compared with participants with HbA1c levels of 5.5–5.9%, multivariate-adjusted HRs and 95% confidence intervals for all-cause death of participants with levels < 5.0%, 5.0–5.4%, 6.0–6.4%, and ≥ 6.5% and participants with known diabetes were 1.84 (1.35–2.51), 1.13 (0.95–1.34), 1.30 (1.04–1.62), 1.37 (0.97–1.93), and 2.03 (1.70–2.44), respectively. The risk of cancer mortality was significantly increased in HbA1c < 5.0% (HR, 2.21; 95% CI 1.42–3.44) and known diabetes (HR, 1.60; 95% CI 1.18–2.15). When we performed diverse subgroup analyses, low HbA1c levels at baseline were strongly associated with mortality in participants with liver diseases.
Conclusions
We found U-shaped associations between HbA1c levels at baseline and over time and all-cause mortality in middle-aged and older Koreans. Additionally, the risk of cancer mortality increased both in low and high HbA1c groups, but CVD mortality increased only in high HbA1c group. In particular, people with liver diseases and low HbA1c levels had a high risk of all-cause mortality. Therefore, more careful management of these groups is suggested to identify any deteriorating health conditions.
Graphical abstract

Similar content being viewed by others
Background
The prevalence of diabetes, a major cause of premature death and disability, is increasing worldwide, especially in Asia [1,2,3]. Glycated haemoglobin (HbA1c) represents the average glycemia for the preceding 2–3 months and is an established biomarker for monitoring glycaemic control in patients with diabetes [4]. Compared with fasting blood glucose, HbA1c has the advantages that it provides higher repeatability and can be assessed in the non-fasting state [4, 5]. In 2010, the American Diabetes Association and the World Health Organization added an HbA1c threshold of ≥ 6.5% as a standard criterion for the diagnosis of diabetes [6, 7].
In previous studies, the relationship between HbA1c levels and mortality was conflicting. Some cohort studies have observed a positive linear relationship between HbA1c levels and mortality [8,9,10,11], whereas others have reported U- or J-shaped associations, with increased mortality at both low and high HbA1c levels [12,13,14,15,16]. This inconsistency might be due to differences in the characteristics of the study populations, causes of death, control for important confounders, and analytic methods. Most of the studies on the association between HbA1c levels and mortality were conducted in western countries, with only a few exceptions targeting the Asian population [9, 17]. Since racial differences have also been reported that HbA1c levels in Asians are higher than in Whites among individuals without diabetes [18], patients with impaired glucose tolerance [19], and patients with type 2 diabetes [20], it is necessary to study the relationship between HbA1c levels and mortality in Asians. Moreover, most of the previous studies used a single HbA1c measurement; therefore, could not reflect the change in glycemic status during follow up. Therefore, we examined whether HbA1c was associated with all-cause and cause-specific mortality using repeated measures from 16 years of cohort follow up data in middle-aged and older Koreans.
Methods
Study population
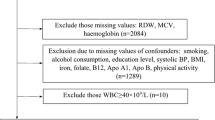
We used data from the Ansan–Ansung Cohort of the Korean Genome and Epidemiology Study (KoGES), which is an ongoing prospective community-based cohort study investigating the environmental and genetic factors affecting prevalent chronic diseases. The study design is described in detail elsewhere [21]. In brief, the Ansan–Ansung cohort study recruited 10,030 individuals aged 40–69 years in a rural (Ansung) and an urban (Ansan) area from 2001 to 2002. Participants were followed up biennially, and we used the follow-up data until 2016 for this study. The final analytical sample of the present study consisted of 9294 participants (4458 men and 4836 women) after excluding those without HbA1c data (n = 3), those with missing covariates (n = 224), those having a history of CVD or cancer (n = 367) at baseline, and those without linked mortality data (n = 142) (Fig. 1). All participants provided written informed consent, and the study protocol was approved by the Institutional Review Board of National Institute of Health, Korea.
Measurements
During each examination, information on socio-demographic and lifestyle characteristics, personal medical histories and medication usage were collected by trained interviewers using structured questionnaires.
Anthropometric measurements were obtained by trained research staff using standardized protocols and all measuring instruments were calibrated everyday before examination. Standing height was measured using a stadiometer (SECA 225; SECA, Germany) and body weight was measured using a digital scale (GL-60000-20; CAS Korea, Korea). Waist circumference was measured at the midpoint between the lower rib margin and the top of the iliac crest in the standing position. Blood pressure was measured by nurses in both arms in a sitting position with the arms supported at heart level after 5 min of rest using mercury sphygmomanometers (Baumanometer-Standby; W.A. Baum Co. Inc., USA). We used means of measurements from both arms for systolic blood pressure (SBP) and diastolic blood pressure (DBP).
Blood samples of all participants were collected from the antecubital vein after at least 8 h of fasting. HbA1c levels were measured using high performance liquid chromatography (Bio-Rad Variant II; Bio-Rad Laboratories, Inc., Japan) according to the National Glycohemoglobin Standardization Program. The total cholesterol, high-density lipoprotein (HDL) cholesterol, triglycerides, fasting blood glucose, total bilirubin, aspartate aminotransferase (AST), and alanine aminotransferase (ALT) levels were measured using enzymatic methods (HITACHI Automatic Analyzer 7600; Hitachi, Japan and ADVIA 1650 Auto Analyzer; Siemens, USA). The red blood cell (RBC), hemoglobin, and hematocrit levels were measured using optical methods by laser beam (ADVIA 120 Hematology System; BAYER, USA).
Known diabetes was defined as having a history of physician-diagnosed diabetes or under treatment with oral antidiabetic agents or insulin at each wave of examination. Hypertension was defined as SBP ≥ 140 mmHg or DBP ≥ 90 mmHg, having a history of physician-diagnosed hypertension, or under treatment for hypertension. Dyslipidemia was defined as total cholesterol ≥ 230 mg/dL, HDL cholesterol < 40 mg/dL, or triglycerides ≥ 200 mg/dL, having a history of physician-diagnosed dyslipidemia, or under treatment for dyslipidemia. Liver disease was defined as having a history of physician-diagnosed hepatitis or liver cirrhosis. Anaemia was defined as haemoglobin < 13 g/dL for men and haemoglobin < 12 g/dL for women.
Mortality outcomes
The cohort data were linked to death records (until 31 December 2017) provided by Statistics Korea using resident registration numbers, a unique identifier assigned to all citizens in the Republic of Korea. All death certificates in Koreans are registered to the government, and cause-of-death are ascertained by medical certificates supplemented by linkage to 21 administrative datasets (e.g. National Health Insurance data, National Cancer Registry, and Police Report) to enhance acccuracy of identifying the underlying causes by Statistic Korea (Statistics Korea, Annual report on the causes of death statistics, 2021). The present study investigated the all-cause mortality and cause-specific mortality from CVD (I00 to I99) and cancer (C00 to C97) as classified by the Korean Classification of Diseases, 6th Revision (the Korean version of the International Classification of Diseases, 10th Revision). We also examined mortality from all external causes (S00 toT98) as a negative control.
Statistical analyses
Participants were divided into a known diabetes group and five groups categorized by HbA1c levels (< 5.0%, 5.0–5.4%, 5.5–5.9%, 6.0–6.4%, and ≥ 6.5%) as previously described [9, 12, 22]. The baseline characteristics of participants across HbA1c groups are presented as means and standard deviations for normally distributed continuous variables and as medians and interquartile ranges for skewed continuous variables. Categorical variables are presented as numbers with percentages. Linear trends across HbA1c groups were tested using linear regression for continuous variables and the Cochran–Armitage test or the Mantel–Haenszel test for categorical variables. The Cox proportional hazards model was used to calculate hazard ratios (HRs) for all-cause and cause-specific mortality according to HbA1c category. The proportional hazards assumption was assessed by using log–log survival plots, and no violations were detected. The 5.5–5.9% HbA1c category was set as the reference group. Covariates consisted of factors affecting HbA1c levels and factors reported in the literature to be related to both HbA1c levels and mortality: age (years), sex, residential area (Ansung or Ansan), BMI (kg/m2), smoking (current, past, or never), alcohol use (current, past, or never), regular exercise (yes or no), education (above or below university), hypertension (yes or no), and dyslipidaemia (yes or no).
Models were constructed in the following two ways: (1) a standard Cox proportional hazards model using the baseline HbA1c levels and covariates and (2) a time-dependent Cox propotional hazards model considering HbA1c levels, age, BMI, smoking, alcohol use, regular exercise, hypertension, and dyslipidemia that change over time as time-dependent variables using information from follow-up examination. Missing data were replaced with the values measured in the previous examination. When estimating the risk of cause-specific mortality from CVD, cancer, and external causes, mortality from the other causes was considered competing risk using the Fine–Grey model. Person-years for each participant were calculated as the duration from the baseline examination date to the date of death or 31 December 2017 depending on which came first. Mortality rates per 1000 person-years were calculated for each HbA1c category.
To assess whether the association between HbA1c levels and the risk of mortality differed according to the characteristics of study participants, subgroup analyses were performed for age, sex, smoking status, hypertension, liver diseases, and RBC count. We also tested the interaction effect between HbA1c levels and the characteristics of study participants on mortality using interaction terms.
For sensitivity analysis, we additionally adjusted for RBC count, haemoglobin level, anaemia, and liver diseases which are known to affect HbA1c in our analytical models. We also adjusted for waist circumference instead of BMI. Furthermore, to rule out the effects of possible subclinical disease or underlying poor health condition, we excluded 77 people who died within the first 2 years of follow-up.
After excluding participants with known diabetes, restricted cubic spline regression analyses were performed to model the shape of the association between continuous HbA1c levels at baseline and mortality. Knots were set at the 5th, 25th, 75th, and 95th percentiles and reference was set at the median HbA1c level of 5.6%. The plot was truncated at the 1st and 99th percentiles.
Additionally, we compared the receiver-operating characteristic (ROC) curves and the area under the curve (AUC) for mortality of a conventional model and the model plus baseline HbA1c. The conventional model included age, sex, residential area, BMI, smoking, alcohol use, regular exercise, education, hypertension, and dyslipidemia.
SAS version 9.4 (SAS Institute, Cary, NC, USA) was used for all statistical analyses, and statistical significance was defined as two-tailed p values < 0.05.
Results
Table 1 presents the baseline characteristics of the study population stratified by HbA1c levels. Participants with higher HbA1c levels were more likely to be older and had higher BMI, waist circumferences, RBC counts, haemoglobin levels, hypertension and dyslipidaemia prevalences, and proportion of current smokers; lower prevalence of anaemia, proportion of current alcohol drinkers, and education level. On the other hand, participants with lower HbA1c levels tended to have lower RBC counts and higher prevalence of anaemia and liver diseases.
During 139,960 person-years of follow-up (median 15.7 years), there were 944 deaths, including 185 deaths from CVD, 359 from cancer, and 125 from external causes. Compared with participants with baseline HbA1c levels of 5.5–5.9% as a reference, multivariate-adjusted HRs and 95% confidence intervals for all-cause mortality of participants with HbA1c levels < 5.0%, 5.0–5.4%, 6.0–6.4%, and ≥ 6.5% and participants with known diabetes were 1.74 (1.18–2.57), 1.20 (1.01–1.42), 1.50 (1.23–1.83), 1.62 (1.24–2.11), and 2.30 (1.88–2.81), respectively. When we considered changes in HbA1c levels and other covariates during follow-up, the U-shaped associations between HbA1c and all-cause mortality persisted. Specifically, significantly elevated risks of mortality were found in HbA1c < 5.0% (HR, 1.84; 95% CI 1.35–2.51), 6.0–6.4% (HR, 1.30; 95% CI 1.04–1.62), and known diabetes (HR, 2.03; 95% CI 1.70–2.44). We also found a U-shaped association for baseline HbA1c with cancer mortality. In a time-dependent Cox model, the association between HbA1c and cancer mortality was not clear except significantly elevated risk in HbA1c < 5.0% (HR, 2.21; 95% CI 1.42–3.44) and known diabetes (HR, 1.60; 95% CI 1.18–2.15). HbA1c levels at baseline examination were not significantly associated with CVD mortality, whereas HbA1c > 6.5% over time showed an elevated risk with HR 2.39 (95% CI 1.27–4.48). Known diabetes assessed at baseline and over time were associated with 130% increased risk of CVD mortality (Table 2).
The findings were not changed materially after we additionally adjusted for RBC count, haemoglobin level, anaemia, and liver diseases (Additional file 1); excluded 77 people who died within the first 2 years of follow-up (Additional file 2); and adjusted for waist circumference instead of BMI (data not shown).
In subgroup analysis, we observed broadly consistent results for risks of all-cause mortality by baseline HbA1c levels, whereas the risk of all-cause mortality was significantly associated with low HbA1c levels of < 5.0% only among people with liver diseases or below median RBC counts (4.72 Mil/µL for men and 4.15 Mil/µL for women). Interaction was significant only between HbA1c and liver diseases (Table 3).
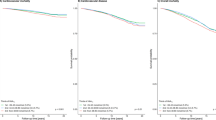
Restricted cubic spline regression models for individuals without known diabetes revealed a J-shaped association between continuous baseline HbA1c levels and all-cause mortality (p-nonlinearity = 0.032) (Fig. 2a). However, no pattern was observed in the associations between HbA1c and mortality from CVD and external causes (Fig. 2b, d). A slight J-shaped association was observed in cancer mortality, but it was not significant (Fig. 2c). When we analyzed the predictive value of HbA1c for mortality using ROC, the performance was slightly increased for cancer mortality compared with the conventional model (Additional file 3).
Discussion
In the present study of the general Korean population with neither a history of cancer nor CVD, non-diabetic adults with low HbA1c were at significantly higher risk of all-cause and cancer mortality compared with individuals with HbA1c of 5.5–5.9%. Higher HbA1c levels in the prediabetic and diabetic ranges were associated with an increased risk of all-cause mortality in a dose–response manner. HbA1c levels lower than diabetic range was not associated with increased risk of CVD mortality. Adults with known diabetes had higher risk of all-cause, CVD, and cancer mortality. Death from external causes, a negative control, was not associated with either low or high HbA1c. Furthermore, when stratified by the median RBC count or by having liver diseases, there was a strong association between low HbA1c levels and all-cause mortality among individuals with low RBC counts or liver diseases.
Our results are consistent with previous findings of U-shaped or J-shaped associations between HbA1c levels and mortality [12,13,14,15,16]. In the Atherosclerosis Risk in Communities (ARIC) study, non-diabetic participants with HbA1c levels < 5.0% (HR, 1.48; 95% CI 1.21–1.81), as well as those with HbA1c levels ≥ 5.5%, were at a significantly increased risk of death from any cause compared with those with HbA1c 5.0 to < 5.5% [15]. In the general German population without known diabetes, restricted cubic spline models showed a U-shaped association between HbA1c levels and all-cause mortality: the lowest risk was at HbA1c levels of 5.4–5.6% and a significantly increased risk were observed both at ≤ 5.0% and ≥ 6.4% [16]. The association between extremely low HbA1c level and mortality was assessed among US National Health and Nutrition Study III participants without diabetes. Compared with HbA1c levels of 5.0–5.4%, HbA1c levels < 4.0% were associated with significantly increased risk of all-cause mortality in a fully adjusted model (HR, 2.90; 95% CI 1.25–6.76) [12]. In the general New Zealand population, the HR for all-cause mortality among individuals with HbA1c levels < 4.0% versus 4.0–4.9% was higher with marginal statistical significance (HR, 2.90; 95% CI 0.91–9.19) [13]. In the current study, we were unable to examine extremely low HbA1c levels < 4.0% because the number of participants in that group was very small (n = 2).
On the other hand, several prospective cohort studies have reported that only high HbA1c levels increase mortality [9,10,11, 17]. In the general Japanese population, compared with HbA1c levels < 5.0%, high HbA1c levels (> 6.0%) in individuals without treatment for diabetes were significantly associated with an increased risk of all-cause and CVD mortality [9]. In Singaporean Chinese adults without diagnosed diabetes, compared with HbA1c levels of 5.4–5.6%, only HbA1c levels ≥ 6.5% were significantly associated with all-cause (HR, 1.96; 95% CI 1.56–2.46), CVD (HR, 2.63; 95% CI 1.77–3.90), and cancer (HR, 1.51; 95% CI 1.04–2.18) mortality [17]. In Australian adults (aged ≥ 25 years) without diagnosed diabetes, HbA1c levels exhibited a linear relationship with all-cause and CVD mortality [11].
Biological mechanisms between hyperglycaemia and an increased risk of mortality may be due to the vascular damage caused by increased oxidative stress and endothelial dysfunction in individuals with impaired fasting glucose or impaired glucose tolerance [23, 24]. Moreover, elevated HbA1c levels influences cancer progression through an increase in the levels of insulin, insulin-like growth factor-1 (IGF-1), and inflammatory cytokines in circulation [25, 26]. However, the potential mechanism underlying the association between low HbA1c levels and increased mortality remains unclear. Low HbA1c levels have been correlated with impaired RBC related indices and increased liver function indices [12, 22]. These factors, in turn, were shown to correlate with inflammatory processes and increased morbidity and mortality [27, 28]. In other words, low HbA1c levels are considered a marker of deteriorated health condition. Thus, the association between low HbA1c levels and higher mortality may be explained by a result of reverse causation due to comorbid conditions [12, 22]. In our study sample, participants with HbA1c levels < 5% had lower RBC, haemoglobin, and haematocrit levels and higher total bilirubin levels and prevalence of liver diseases than did those with HbA1c levels of 5.5–5.9%, the reference group. Moreover, HbA1c levels < 5% were associated with an increased risk of all-cause mortality only among people with pre-existing liver disease or less than median RBC counts. These results suggest potential roles of RBC and liver function in the association between low HbA1c levels and increased mortality.
The strength of this study lies in the long-term population-based cohort design (16-year follow-up) and the consideration of changes of HbA1c levels and other clinical and lifestyle variables during the follow-up period. Most of the previous studies used the time-fixed method with the baseline HbA1c levels and did not reflect the change of HbA1c during the follow-up period [9,10,11,12,13,14,15,16,17]. However, we used the time-dependent method considering the change of HbA1c over time which is more reflective of clinical practice. To the best of our knowledge, this is the first study to evaluate the association between HbA1c levels and mortality in the general Korean population and to find an increased risk of mortality at low HbA1c levels in the Asian population.
Despite its strengths, the current study had some limitations. First, the participants were aged 40–70 years at the baseline examination and were enrolled from two communities. Therefore, the findings of this study may not be directly generalizable to younger adults or the entire Korean population. However, general characteristics and HbA1c level distribution were similar when we compared our study population with the Korea National Health and Nutrition Examination Survey (KNHANES) participants, who are a representative sample. Specifically, among the KNHANES participants aged 40–70 in 2019, 44% were men, the mean age was 55.0 years, and the mean HbA1c level was 5.9% [29]. Second, among the 9294 participants who met the inclusion criteria at baseline, 14.5% did not attend any follow-up examination until 2016. However, the major variables, such as HbA1c levels, age, sex, and comorbidities, were similar between participants and nonparticipants in the follow-up examinations (data not shown). Therefore, it is unlikely that the association between HbA1c levels and mortality found in the time-dependent analysis using follow-up data is severely underestimated or overestimated. Third, a small number of participants with extremely low HbA1c levels in our study sample hindered more detailed analysis. Fourth, information on the diagnosis and treatment of diabetes, hypertension, dyslipidaemia, and liver diseases was obtained from questionnaires. Participants omitting to report existing diseases or having undiagnosed health conditions could have limited our ability to classify people with diabetes or other existing diseases. However, we collected data on the disease history using a structured questionnaire with questions about each disease asked separately by trained interviewers. Moreover, missing rates of related variables were very low (0.04%). Finally, although we adjusted for several potential confounders in our analysis, residual confounding may remain due to unmeasured or uncontrolled confounders such as statins use that might affect blood glucose control [30].
Conclusions
In summary, there was a U-shaped association between HbA1c levels at baseline and over time and all-cause mortality in middle-aged and older Koreans. Additionally, we found increase risk of cancer mortality both in low and high HbA1c groups, but the risk of CVD mortality was increased only in the high HbA1c group over time. These findings suggest that people with low HbA1c levels, as well as those with high HbA1c levels, have an increased risk of mortality. HbA1c testing may improve the identification of individuals with a high risk of mortality. In particular, for people with liver diseases and low HbA1c levels, more careful management is suggested to identify any deteriorating health conditions. Causal mechanisms underlying the increased cause-specific mortality risk in the lower HbA1c range warrant investigation. Thus, further studies with a large number of individuals with very low HbA1c levels and a detailed assessment of morbid conditions are needed. In addition, further studies to identify the usefulness and appropriate cut-off HbA1c level for predicting mortality are needed.
Availability of data and materials
The KoGES data and biospecimens are available for research purposes from https://www.nih.go.kr/ on reasonable request.
Abbreviations
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CVD:
-
Cardiovascular disease
- DBP:
-
Diastolic blood pressure
- HbA1c :
-
Haemoglobin A1C
- HDL:
-
High-density lipoprotein
- HR:
-
Hazard ratio
- KoGES:
-
Korean Genome and Epidemiology Study
- RBC:
-
Red blood cell
- SBP:
-
Systolic blood pressure
References
World Health Organization. Global report on diabetes. Geneva: World Health Organization; 2016.
Danaei G, Finucane MM, Lu Y, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2· 7 million participants. Lancet. 2011;378(9785):31–40.
Yuan H, Li X, Wan G, et al. Type 2 diabetes epidemic in East Asia: a 35-year systematic trend analysis. Oncotarget. 2018;9(6):6718.
Sacks DB, Bruns DE, Goldstein DE, Maclaren NK, McDonald JM, Parrott M. Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Clin Chem. 2002;48(3):436–72.
Nathan D, Turgeon H, Regan S. Relationship between glycated haemoglobin levels and mean glucose levels over time. Diabetologia. 2007;50(11):2239–44.
Association AD. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Supplement 1):S62–9.
World Health Organization. Use of glycated hemoglobin (HbA1c) in the diagnosis of diabetes mellitus. Abbreviated report of a WHO consultation. Geneva: World Health Organization; 2011.
Khaw K-T, Wareham N, Bingham S, Luben R, Welch A, Day N. Association of hemoglobin A1c with cardiovascular disease and mortality in adults: the European prospective investigation into cancer in Norfolk. Ann Intern Med. 2004;141(6):413–20.
Sakurai M, Saitoh S, Miura K, et al. HbA1c and the risks for all-cause and cardiovascular mortality in the general Japanese population: NIPPON DATA90. Diabetes Care. 2013;36(11):3759–65.
Levitan E, Liu S, Stampfer M, et al. HbA 1c measured in stored erythrocytes and mortality rate among middle-aged and older women. Diabetologia. 2008;51(2):267–75.
Barr E, Boyko E, Zimmet P, Wolfe R, Tonkin A, Shaw J. Continuous relationships between non-diabetic hyperglycaemia and both cardiovascular disease and all-cause mortality: the Australian Diabetes, Obesity, and Lifestyle (AusDiab) study. Diabetologia. 2009;52(3):415–24.
Carson AP, Fox CS, McGuire DK, et al. Low hemoglobin A1c and risk of all-cause mortality among US adults without diabetes. Circ Cardiovasc Qual Outcomes. 2010;3(6):661–7.
Brewer N, Wright CS, Travier N, et al. A New Zealand linkage study examining the associations between A1C concentration and mortality. Diabetes Care. 2008;31(6):1144–9.
Li F-R, Zhang X-R, Zhong W-F, et al. Glycated hemoglobin and all-cause and cause-specific mortality among adults with and without diabetes. J Clin Endocrinol Metab. 2019;104(8):3345–54.
Selvin E, Steffes MW, Zhu H, et al. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med. 2010;362(9):800–11.
Paprott R, Rosario AS, Busch MA, et al. Association between hemoglobin A1c and all-cause mortality: results of the mortality follow-up of the German National Health Interview and Examination Survey 1998. Diabetes Care. 2015;38(2):249–56.
Bancks MP, Odegaard AO, Pankow JS, et al. Glycated hemoglobin and all-cause and cause-specific mortality in Singaporean Chinese without diagnosed diabetes: the Singapore Chinese Health Study. Diabetes Care. 2014;37(12):3180–7.
Cavagnolli G, Pimentel AL, Freitas PAC, Gross JL, Camargo JL. Effect of ethnicity on HbA1c levels in individuals without diabetes: systematic review and meta-analysis. PLoS ONE. 2017;12(2):e0171315.
Herman WH, Ma Y, Uwaifo G, et al. Differences in A1C by race and ethnicity among patients with impaired glucose tolerance in the Diabetes Prevention Program. Diabetes Care. 2007;30(10):2453–7.
Herman WH, Dungan KM, Wolffenbuttel BH, et al. Racial and ethnic differences in mean plasma glucose, hemoglobin A1c, and 1, 5-anhydroglucitol in over 2000 patients with type 2 diabetes. J Clin Endocrinol Metab. 2009;94(5):1689–94.
Kim Y, Han B-G, Group K. Cohort profile: the Korean genome and epidemiology study (KoGES) consortium. Int J Epidemiol. 2016;46(2):e20.
Christman AL, Lazo M, Clark JM, Selvin E. Low glycated hemoglobin and liver disease in the US population. Diabetes Care. 2011;34(12):2548–50.
Ceriello A. Cardiovascular effects of acute hyperglycaemia: pathophysiological underpinnings. Diabetes Vasc Dis Res. 2008;5(4):260–8.
Schisano B, Tripathi G, McGee K, McTernan P, Ceriello A. Glucose oscillations, more than constant high glucose, induce p53 activation and a metabolic memory in human endothelial cells. Diabetologia. 2011;54(5):1219–26.
Johnson J, Carstensen B, Witte D, et al. Diabetes and cancer (1): evaluating the temporal relationship between type 2 diabetes and cancer incidence. Diabetologia. 2012;55(6):1607–18.
Ryu TY, Park J, Scherer PE. Hyperglycemia as a risk factor for cancer progression. Diabetes Metab J. 2014;38(5):330–6.
Montagnana M, Cervellin G, Meschi T, Lippi G. The role of red blood cell distribution width in cardiovascular and thrombotic disorders. Clin Chem Lab Med. 2012;50(4):635–41.
Lioudaki E, Ganotakis ES, Mikhailidis DP. Liver enzymes: potential cardiovascular risk markers? Curr Pharm Des. 2011;17(33):3632–43.
The Korea National Health and Nutrition Examination Survey Database. Available from https://knhanes.kdca.go.kr/knhanes/sub03/sub03_02_05.do. Accessed April 7 2022
Sunjaya AP, Sunjaya AF, Halim S, Ferdinal F. Risk and benefits of statins in glucose control management of type II diabetes. Int J Angiol. 2018;27(03):121–31.
Acknowledgements
The data in this study were from the Korean Genome and Epidemiology Study (KoGES 4851-302), National Institute of Health, Korea Disease Control and Prevention Agency, Republic of Korea. The authors thank the participants and staff of the KoGES.
Funding
This research received no specific grant.
Author information
Authors and Affiliations
Contributions
BMS analysed the data and wrote the paper under the supervision of SSK. JHL, HDW, MJC, and SSK aided in the interpretation of the data and provided critical revision of the manuscript for important intellectual content. SSK had primary responsibility for the final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants provided written informed consent, and the study protocol was approved by the Institutional Review Board of National Institute of Health, Korea.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Risk of death according to HbA1c levels at baseline or over time when further adjusted for covariates. Model 1: Adjusted for age, sex, residential area, body mass index, smoking, alcohol use, regular exercise, education, hypertension, dyslipidaemia, and RBC count. Model 2: Adjusted for age, sex, residential area, body mass index, smoking, alcohol use, regular exercise, education, hypertension, dyslipidaemia, and haemoglobin. Model 3: Adjusted for age, sex, residential area, body mass index, smoking, alcohol use, regular exercise, education, hypertension, dyslipidaemia, and anaemia. Model 4: Adjusted for age, sex, residential area, body mass index, smoking, alcohol use, regular exercise, education, hypertension, dyslipidaemia, and liver diseases. RBC red blood cell.
Additional file 2.
Mortality rate and risk of death according to HbA1c levels at baseline or over time after excluding those who died within the first 2 years of follow-up (N = 9217). *Adjusted for age, sex, residential area, body mass index, smoking, alcohol use, regular exercise, education, hypertension, and dyslipidaemia.
Additional file 3.
Comparison of ROC curves and AUC areas of the conventional model* and the model plus HbA1c. *Model with age, sex, residential area, body mass index, smoking, alcohol use, regular exercise, education, hypertension, and dyslipidemia.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Song, B.M., Lee, J.H., Woo, H.D. et al. Association between haemoglobin A1c and all-cause and cause-specific mortality in middle-aged and older Koreans: a prospective cohort study. Nutr Metab (Lond) 19, 46 (2022). https://doi.org/10.1186/s12986-022-00682-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12986-022-00682-4