Abstract
Background
People living with HIV (PLWHIV) commencing antiretroviral therapy (ART) in sub-Saharan Africa experience significant mortality within the first year. Previously, identified risk factors for mortality may be biased towards these patients, as compared to those who experience late mortality.
Aim
To compare risk factors for early and late mortality in PLWHIV commencing ART.
Methods
A retrospective cohort study of ART-naïve patients aged ≥ 18 years from an outpatient HIV clinic in Zimbabwe. Data were collected between January 2010 and January 2019. Predictors for early (≤ 1 year) and late mortality (> 1 year) were determined by multivariable cox proportional hazards analyses, with patients censored at 1 year and landmark analysis after 1 year, respectively.
Results
Three thousand and thirty-nine PLWHIV were included in the analysis. Over a median follow-up of 4.6 years (IQR 2.5–6.9), there was a mortality rate of 8.8%, with 50.4% of deaths occurring within 1 year. Predictors of early mortality included CD4 count < 50 cells/µL (HR 1.84, 95% CI 1.24–2.72, p < 0.01), WHO Stage III (HR 2.05, 95% CI 1.28–3.27, p < 0.01) or IV (HR 2.83, 95% CI 1.67–4.81, p < 0.01), and eGFR < 90 mL/min/1.73 m2 (HR 2.48, 95% CI 1.56–3.96, p < 0.01). Other than age (p < 0.01), only proteinuria (HR 2.12, 95% CI 1.12–4.01, p = 0.02) and diabetes mellitus (HR 3.51, 95% CI 1.32–9.32, p = 0.01) were associated with increased risk of late mortality.
Conclusions
Traditional markers of mortality risk in patients commencing ART appear to be limited to early mortality. Proteinuria and diabetes are some of the few predictors of late mortality, and should be incorporated into routine screening of patients commencing ART.
Similar content being viewed by others

Introduction
In 2020, there were approximately 25 million people living with HIV (PLWHIV) in sub-Saharan Africa, accounting for more than two thirds of the global burden of HIV [1]. People living with HIV who commence antiretroviral therapy (ART) in the region have been shown to have mortality rates of 5–41%, across follow-up periods of up to 60 months, with the majority of deaths occurring within the first year [2, 3]. Similar high early mortality is not observed in resource-rich settings [4].
In cohorts of PLWHIV from sub-Saharan Africa, low baseline CD4 count, eGFR, and WHO disease stage have been identified as risk factors for mortality [2, 3, 5, 6]. What remains unclear, however, is whether these factors differ between those who succumb to early mortality (within the first year after commencing ART) and those who die later. Those who are at risk of late mortality may not be identified by established predictors, while potentially being more amenable to clinical intervention. There are limited available data at present to evaluate these assertions, however. Here we compare predictors of early and late mortality, in a large cohort of PLWHIV commencing ART, from an outpatient HIV clinic in Zimbabwe.
Methods
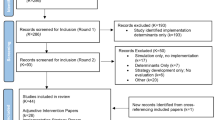
This was a retrospective cohort study of PLWHIV who commenced ART at the Newlands Clinic in Harare, Zimbabwe, a non-government organisation funded by charitable donors which provides free HIV care. Patients who attended the clinic between January 2010 and January 2019 were assessed for eligibility. Inclusion criteria included: age ≥ 18 years, ART-naïve, and having baseline (prior to the initiation of ART treatment) CD4 counts and serum creatinine measurements available. Ethical approval for this study was granted by the Medical Research Council of Zimbabwe (MRCZ/E/258). All research activities were conducted in accordance with the Declaration of Helsinki.
Data collection and analysis
Data were collected from patient electronic medical records. Variables of interest included baseline age, sex, BMI, WHO stage, serum creatinine and CD4 count. Additionally, a documented histories of proteinuria, diabetes mellitus and hypertension at baseline were recorded. Baseline serum creatinine was used to calculate eGFR utilizing the CKD-EPI formula [7]. Renal impairment was defined as a baseline eGFR < 90 mL/min/1.73 m2, severe immunodeficiency as a CD4 count < 50 cells/µL, and proteinuria as urine dipstick protein of ≥1 +.
Statistical analysis
Patients were grouped into those who experienced no mortality, early mortality (within one year of starting ART) and those who experienced late mortality (over one year of ART). Comparisons between groups were by unpaired t-tests, one-way ANOVA, and chi-square, as appropriate. Games Howell post-hoc test was applied to ANOVA where homogeneity of variance was not satisfied. To compare predictors for early and late mortality, two multivariable cox proportional hazards analyses were conducted. For early mortality risk factors, a regression was conducted where patients were censored after one year. For late mortality, a landmark regression analysis was performed, limited to patients with over one year of survival data. Potential predictors were included a priori and included sex, age, BMI, proteinuria, diabetes mellitus, hypertension, WHO stage, renal impairment, and severe immunodeficiency. Data are presented as median (IQR) or mean ± SD where appropriate.
Results
Between January 2010 and January 2019, 3039 patients at the Newlands Clinic met inclusion criteria for this study. The median age of the cohort was 36 years (IQR 30–43), with the majority of the cohort being female (62.1%). Over a median follow-up time of 4.6 years (IQR 2.5–6.9), there was a mortality rate of 8.8%. Approximately half of the patients who died (132/266, 50.4%) did so within one year of commencing ART.
Baseline characteristics by mortality status are presented in Table 1. Surviving patients had a higher BMI (24.6 ± 12.5 vs. 22.0 ± 5.4 kg/m2; p < 0.01) and a greater baseline CD4 count (290.2 ± 222.5 vs. 165.1 ± 172.9 cells/µL; p < 0.01) than those who died in the follow-up period, and a greater proportion of surviving patients were a lower WHO stage (p < 0.01). Amongst those who died, those who did so within the first year had a lower BMI (21.2 ± 4.7 vs. 23.4 ± 6.3 kg/m2; p = 0.02), baseline CD4 count (141.9 ± 161.3 vs. 188.9 ± 181.5 cells/µL; p = 0.03), and prevalence of hypertension (7% vs. 17%; p = 0.01) compared to those who experienced late mortality.
Multivariable proportional hazards analyses of potential predictors of early and late mortality are presented in Table 2. A reduced eGFR (< 90 mL/min/1.73 m2) was associated with more than doubling of early mortality risk (HR 2.48, 95% CI 1.56–3.96, p < 0.01), but was not associated with increased late mortality risk (p = 0.59). In contrast, proteinuria was associated with a similarly increased risk of both early mortality (HR 2.29, 95% CI 1.59–3.31, p < 0.01) and late mortality risk (HR 2.12, 95% CI 1.12–4.01, p = 0.02). Hypertension and BMI were associated with reduced early mortality (HR 0.56, 95% CI 0.33–0.94, p = 0.03 and HR 0.95, 95% CI 0.92, 0.99, p = 0.02 respectively), but not late mortality (p = 0.42 and p = 0.80, respectively). Diabetes mellitus predicted mortality in both the early (HR 2.33, 95% CI 1.10–4.91, p = 0.03) and the late mortality group (HR 3.51, 95% CI 1.32–9.32, p = 0.01). For early mortality, WHO stage III (HR 2.05, 95% CI 1.28–3.27, p < 0.01) and stage IV (HR 2.83, 95% CI 1.67–4.81, p < 0.01) were significant predictors, but were not for late mortality (p = 0.08 and p = 0.40, respectively). A CD4 count < 50 cells/µL was also associated with early (HR 1.84, 95% CI 1.24–2.72, p < 0.01) but not late mortality (p = 0.71).
Discussion
Our study compared risk factors for early and late mortality in PLWHIV commencing ART in sub-Saharan Africa. Our findings suggest that previously established risk factors for mortality, including low CD4 count, WHO stage III or IV, and reduced renal function, may not identify patients at risk of death after more than one year of ART.
WHO stage III and IV are well established predictors of mortality [2, 8,9,10]. While these stages were associated with more than a doubling of early mortality risk in our study, we did not find an increased risk after 1 year of ART. A similar trend was noted by Moore et al. [11] in a cohort from Uganda comparing patients who died before or after 3 months of ART. There, WHO stage III or IV was associated with a nine-fold increased risk of early mortality, but only a three-fold increase in mortality after 3 months. This apparent waning of the predictive value of WHO stage may relate in part to immune reconstitution inflammatory syndrome (IRIS), which is more common in patients with more advanced immunodeficiency on commencement of ART [12,13,14]. Haddow et al. [15] reported a cumulative incidence of IRIS of 22.9% in their cohort of adult PLWHIV initiating ART in South Africa, with IRIS accounting for nearly one quarter of total clinical events and deaths within the first six months of treatment. This suggests a meaningful contribution of IRIS to early mortality. However, other research in sub-Saharan Africa has shown that IRIS did not largely contribute to mortality in adult PLWHIV undergoing ART treatment—one study in Uganda demonstrated that 7% of total HIV-related deaths within the first three months of ART were related to IRIS [16], whereas another study in Johannesburg observed that among IRIS patients, there was a 4.5% IRIS-related mortality rate within 6 months of starting ART [17]. Therefore, the contribution of IRIS in the present study is unclear. Whether late mortality risk could be predicted by restaging patients after a period of ART remains a possibility, however, and is an important avenue for further research.
A baseline eGFR < 90 mL/min/1.73 m2 was associated with a 2.5-fold increase in mortality risk of early, but not late mortality. Reports of other cohorts from the region have also identified eGFR as a significant risk factor for mortality, with lower levels of renal function being associated with greater mortality risk [5, 6]. We were unable to determine if more severe renal impairment was associated with a late mortality risk as few patients in our cohort had a baseline eGFR < 60 mL/min/1.73 m2. As our study used a single measure of creatinine to determine baseline renal function, we were also unable to differentiate patients with acute kidney injury from those with chronic kidney disease.
The presence of proteinuria at baseline was associated with a doubling of both early and late mortality risk. As with serum creatinine, baseline proteinuria status was assessed by a single measure. It may be that dipstick proteinuria is less affected than serum creatinine by factors such as hydration status or muscle wasting and so provides a more reliable assessment than a single measure of serum creatinine. Proteinuria status is also important to identify patients with potential HIV-associated nephropathy, which presents as proteinuria with rapidly progressive renal failure [18].
The apparent protective effect of hypertension in the early mortality group was likely artefactual, a consequence of normotensive and hypotensive patients being grouped together. Hypotension has previously been shown to increase mortality risk in a cohort of PLWHIV from Kenya, with increasing severity of hypotension linked to increasing mortality risk. However, this association was not observed in the subset of patients with advanced HIV disease [19]. While hypertension was not associated with late mortality risk in our cohort, this may have been due to a median follow-up time of only 2.9 years. However, deleterious changes from hypertension have been shown to occur within this timeframe. In previously published data from this same cohort, hypertension predicted renal function loss over a period of only six months [20]. These findings suggest the clinical importance of identifying those with hypotension, as this may contribute to elevated early mortality risk.
A higher body mass index was a protective factor for early mortality, as noted in other cohorts of PLWHIV commencing ART in sub-Saharan Africa [2, 3]. A lower baseline BMI has also been associated with increased mortality within the first 3 months [21,22,23]. Zachariah et al. [22] observed a linear trend between increased mortality risk within the first 3 months and reductions in BMI below 18.5–16 kg/m2, with a marked increase in mortality risk once BMI falls below 16 kg/m2. This is likely a result of those with lower BMI representing a complex interaction between undernourishment in addition to HIV-associated wasting, as sub-Saharan Africa is disproportionately affected by both food scarcity and HIV infection [24]. Together, these factors increase disease progression, likely contributing to the exaggerated early mortality observed in PLWHIV with low BMI initiating ART in sub-Saharan Africa [21,22,23]. One study from Zambia indicated a significant prevalence of wasting in a cohort of people with severe HIV initiating ART, with 34% of the cohort having a BMI of < 18.5 kg/m2 at baseline [25]. The increased early mortality observed in sub-Saharan PLWHIV initiating ART is believed to be a culmination of immune dysfunction secondary to malnutrition, metabolic derangements resulting from an increased basal metabolic rate and/or selective skeletal muscle atrophy, as well as increased burden of opportunistic infections [26].
The main limitation of this study is that it examined ambulatory patients at a single clinic in Zimbabwe, and so may not be generalizable to other populations in sub-Saharan Africa. Reports of other cohorts have found similar protective benefits of a higher BMI, as well as increased risk of mortality associated with reduced eGFR, CD4 count, and WHO Stage III and IV [2, 3, 27]. These studies also had similar baseline BMI, mean CD4 count and eGFR compared to the present study. Therefore, it is likely that the present findings are generalizable to the larger sub-Saharan African PLWHIV population.
Conclusions
Traditional risk factors for mortality including CD4 count, WHO stage, and renal impairment did not identify patients at increased mortality risk after one year from ART commencement in the present study. Late mortality risk was increased by the presence of proteinuria and having diabetes mellitus, however, and screening for these risk factors should form part of routine clinical assessment.
Availability of data and materials
The datasets used in the current study are available from the corresponding author on reasonable request.
Abbreviations
- ART:
-
Antiretroviral therapy
- BMI:
-
Body mass index
- eGFR:
-
Estimated glomerular filtration rate
- HIV:
-
Human immunodeficiency virus
- HR:
-
Hazard ratio
- IQR:
-
Interquartile range
- IRIS:
-
Immune reconstitution inflammatory syndrome
- PLWHIV:
-
People living with HIV
- WHO:
-
World Health Organization
References
UNAIDS. HIV estimates with uncertainty bounds 1990–2020. Global AIDS Update 2020. Geneva: UNAIDS; 2020.
Lawn SD, Harries AD, Anglaret X, Myer L, Wood R. Early mortality among adults accessing antiretroviral treatment programmes in sub-Saharan Africa. AIDS. 2008;22(15):1897–908.
Biset Ayalew M. Mortality and its predictors among HIV infected patients taking antiretroviral treatment in Ethiopia: a systematic review. AIDS Res Treat. 2017;2017:5415298.
Braitstein P, Brinkhof MW, Dabis F, Schechter M, Boulle A, Miotti P, et al. Mortality of HIV-1-infected patients in the first year of antiretroviral therapy: comparison between low-income and high-income countries. Lancet. 2006;367(9513):817–24.
Sarfo FS, Keegan R, Appiah L, Shakoor S, Phillips R, Norman B, et al. High prevalence of renal dysfunction and association with risk of death amongst HIV-infected Ghanaians. J Infect. 2013;67(1):43–50.
Mulenga LB, Kruse G, Lakhi S, Cantrell RA, Reid SE, Zulu I, et al. Baseline renal insufficiency and risk of death among HIV-infected adults on antiretroviral therapy in Lusaka, Zambia. AIDS. 2008;22(14):1821–7.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12.
Sieleunou I, Souleymanou M, Schonenberger AM, Menten J, Boelaert M. Determinants of survival in AIDS patients on antiretroviral therapy in a rural centre in the Far-North Province, Cameroon. Trop Med Int Health. 2009;14(1):36–43.
Poka-Mayap V, Pefura-Yone EW, Kengne AP, Kuaban C. Mortality and its determinants among patients infected with HIV-1 on antiretroviral therapy in a referral centre in Yaounde, Cameroon: a retrospective cohort study. BMJ Open. 2013. https://doi.org/10.1136/bmjopen-2013-003210.
Chalamilla G, Hawkins C, Okuma J, Spiegelman D, Aveika A, Christian B, et al. Mortality and treatment failure among HIV-infected adults in Dar Es Salaam, Tanzania. J Int Assoc Physicians AIDS Care. 2012;11(5):296–304.
Moore DM, Yiannoutsos CT, Musick BS, Tappero J, Degerman R, Campbell J, et al. Determinants of early and late mortality among HIV-infected individuals receiving home-based antiretroviral therapy in rural Uganda. J Acquir Immune Defic Syndr. 2011;58(3):289–96.
French MA, Price P, Stone SF. Immune restoration disease after antiretroviral therapy. AIDS. 2004;18(12):1615–27.
Shelburne SA, Hamill RJ. The immune reconstitution inflammatory syndrome. AIDS Rev. 2003;5(2):67–79.
Ratnam I, Chiu C, Kandala NB, Easterbrook PJ. Incidence and risk factors for immune reconstitution inflammatory syndrome in an ethnically diverse HIV type 1-infected cohort. Clin Infect Dis. 2006;42(3):418–27.
Haddow LJ, Moosa MY, Mosam A, Moodley P, Parboosing R, Easterbrook PJ. Incidence, clinical spectrum, risk factors and impact of HIV-associated immune reconstitution inflammatory syndrome in South Africa. PLoS One. 2012;7(11):e40623.
Castelnuovo B, Manabe YC, Kiragga A, Kamya M, Easterbrook P, Kambugu A. Cause-specific mortality and the contribution of immune reconstitution inflammatory syndrome in the first 3 years after antiretroviral therapy initiation in an urban African cohort. Clin Infect Dis. 2009;49(6):965–72.
Murdoch DM, Venter WD, Feldman C, Van Rie A. Incidence and risk factors for the immune reconstitution inflammatory syndrome in HIV patients in South Africa: a prospective study. AIDS. 2008;22(5):601–10.
Wyatt CM, Klotman PE, D’Agati VD. HIV-associated nephropathy: clinical presentation, pathology, and epidemiology in the era of antiretroviral therapy. Semin Nephrol. 2008;28(6):513–22.
Bloomfield GS, Hogan JW, Keter A, Holland TL, Sang E, Kimaiyo S, et al. Blood pressure level impacts risk of death among HIV seropositive adults in Kenya: a retrospective analysis of electronic health records. BMC Infect Dis. 2014;14:284.
Bleasel JM, Heron JE, Shamu T, Chimbetete C, Dahwa R, Gracey DM. Body mass index and noninfectious comorbidity in HIV-positive patients commencing antiretroviral therapy in Zimbabwe. HIV Med. 2020;21(10):674–9.
Stringer JS, Zulu I, Levy J, Stringer EM, Mwango A, Chi BH, et al. Rapid scale-up of antiretroviral therapy at primary care sites in Zambia: feasibility and early outcomes. JAMA. 2006;296(7):782–93.
Zachariah R, Fitzgerald M, Massaquoi M, Pasulani O, Arnould L, Makombe S, et al. Risk factors for high early mortality in patients on antiretroviral treatment in a rural district of Malawi. AIDS. 2006;20(18):2355–60.
Johannessen A, Naman E, Ngowi BJ, Sandvik L, Matee MI, Aglen HE, et al. Predictors of mortality in HIV-infected patients starting antiretroviral therapy in a rural hospital in Tanzania. BMC Infect Dis. 2008;8:52.
Food and Agriculture Organization of the United Nations. The state of food insecurity in the world. Rome: FAO; 2021.
Koethe JR, Lukusa A, Giganti MJ, Chi BH, Nyirenda CK, Limbada MI, et al. Association between weight gain and clinical outcomes among malnourished adults initiating antiretroviral therapy in Lusaka, Zambia. J Acquir Immune Defic Syndr. 2010;53(4):507–13.
Koethe JR, Heimburger DC. Nutritional aspects of HIV-associated wasting in sub-Saharan Africa. Am J Clin Nutr. 2010;91(4):1138S-42S.
Silverman RA, John-Stewart GC, Beck IA, Milne R, Kiptinness C, McGrath CJ, et al. Predictors of mortality within the first year of initiating antiretroviral therapy in urban and rural Kenya: A prospective cohort study. PLoS ONE. 2019;14(10):e0223411.
Acknowledgements
The authors wish to thank the patients and staff of the Newlands Clinic as well as Dr. Valerie Gracey for her expert statistical advice, which was invaluable in preparing this manuscript.
Funding
There was no specific funding for this study, although research activities in the clinic are supported in part by the International Society of Nephrology’s Sister Renal Centre program.
Author information
Authors and Affiliations
Contributions
BB was involved in the design of the study, analysis and interpretation of data, and development of the manuscript. DD was involved in the design of the study, analysis and interpretation of data, and development of the manuscript. TS was involved in interpretation of data and development of the manuscript. CC was involved in interpretation of data and development of the manuscript. RD was involved in interpretation of data and development of the manuscript. DG was involved in the design of the study, interpretation of data, and development of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for this study was granted by the Medical Research Council of Zimbabwe (MRCZ/E/258). All research activities were conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Byers, B.W., Drak, D., Shamu, T. et al. Comparison of predictors for early and late mortality in adults commencing HIV antiretroviral therapy in Zimbabwe: a retrospective cohort study. AIDS Res Ther 19, 23 (2022). https://doi.org/10.1186/s12981-022-00445-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12981-022-00445-4