Abstract
Background
Deep vein thrombosis (DVT) and pulmonary emboli (PE), known together as venous thromboembolic (VTE) disease remain major complications following elective hip and knee surgery. This study compares three chemoprophylactic regimens for VTE following elective primary unilateral hip or knee replacement, one of which was designed to minimize risk of post-operative bleeding.
Methods
Patients were randomized and stratified for hip vs. knee to receive A: variable dose warfarin (first dose on the night preceding surgery with subsequent target INR 2.0–2.5), B: 2.5 mg fondaparinux daily starting 6–18 h postoperatively, or C: fixed 1.0 mg dose warfarin daily starting 7 days preoperatively. All treatments continued until bilateral leg venous ultrasound day 28 ± 2 or earlier upon a VTE event. The study examined primary endpoints including leg DVT, PE or death due to VTE and secondary endpoints including effects on D-dimer, estimated blood loss (EBL) at surgery and hemorrhagic complications.
Results
Three hundred fifty-five patients were randomized. None was lost to follow-up. Taking 1.0 mg warfarin for seven days preoperatively did not prolong the prothrombin time (PT). Two patients in Arm C had asymptomatic distal DVT. One major bleed occurred in Arm B and one in Arm C (ischemic colitis). Elevated d-dimer did not predict delayed VTE for one year.
Conclusions
Fixed low dose warfarin started preoperatively is equivalent to two other standards of care under study (95 % CI: -0.0428, 0.0067 for both) as VTE prophylaxis for the patients having elective major joint replacement surgery.
Trial registration
ClinicalTrials.gov identifier # NCT00767559
FDA IND: 103,716
Similar content being viewed by others
Background
When initiated prior to elective surgery low dose warfarin has been demonstrated prophylactic capacity against VTE with low risk of hemorrhage [1–14]. Warfarin when given at 1 mg per day is known to increase serum under-gamma-carboxylated osteocalcin and plasma under-gamma-carboxylated prothrombin, without change of prothrombin times or factor VII activity [15]. It is critical in this pharmacologic format that low dose warfarin be initiated prior to the surgical trauma, thus allowing time for warfarin to partially suppress the carboxylation of glutamic acid residues attached to the cores of factors II, VII, IX and X [16]. This sequentially reduces their calcium ion dependent function [16–21] It is this mechanism which we believe reduces the efficiency of calcium binding, thus slowing the efficiency of clotting but not so much as to cause full anticoagulation.
This study is a continuum of studies predicated upon the concept that the clotting system can be kept in a homeostatic balance, making it possible to avoid added risk of bleeding while protecting patients from thromboembolism [1–14]. Among these studies was a prospective pilot study of 100 patients in which patients planning total hip replacement were randomized between two arms, one with warfarin starting with 5.0 mg the night prior to surgery followed by variable dose warfarin (target PT 1.3–1.5 x normal) and the other using 1.0 mg of warfarin beginning seven days prior to surgery, and both continuing for 30–45 days. There was no difference for incidence of venous thrombosis [8]. Another was a retrospective study of patients undergoing primary (n = 833) or revision (n = 170) hip replacement arthroplasty who received 1.0 mg of warfarin for seven days prior to surgery, variable dose warfarin while in hospital (target INR 1.5–2.0) followed by1.0 mg daily until follow-up at 30–45 days. Of 1,003 patients, only 3 (0.3 %) had symptomatic VTE [11].
This current investigator-initiated, single-institution, prospective, randomized, open-label assessor-blind study study compared fixed low dose of warfarin to two control arms as chemoprophylaxis against VTE among patients undergoing elective primary hip or knee replacement. Fixed low dose warfarin was initiated 7 days prior to surgery so as to allow the necessary time for its effects to be in place by the time of surgery. All patients received the same optimal non-pharmacologic support. We hypothesized that the three chemotherapeutic regimens would yield equivalent clinical findings for these patients. If confirmed as effective the fixed low dose regimen should have minimal hemorrhagic potential and would require less laboratory support, but with less cost than the modern novel oral anticoagulants that are also available [22].
Methods
Research design
This was a prospective, randomized three-arm study including two control arms (warfarin and fondaparinux in standard doses) and a third arm using warfarin at 1.0 mg per day starting seven days before surgery. Therapy was continued until a VTE event occurred or until 28 ± 2 days from day of surgery when bilateral leg ultrasounds were performed. (see Table 1) All patients were called 6 and 12 months following their surgery to detect any delayed complications or VTE events.
The primary endpoint was composite DVT, PE or death due to VTE. Secondary endpoints included frequency of proximal vs. distal DVT, estimated blood loss (EBL) at surgery, and hemorrhagic complications.
The hospital’s Institutional Review Board (IRB) approved this study. All patients gave signed informed consent.
Randomization
Total randomized patient allocations were to be at 1:1:1 ratio for each arm at end of study. The randomization was stratified for hip vs. knee surgery. A member of the pharmacy department pulled randomized cards as prepared by the statisticians. The results were communicated to the Clinical Research Coordinator (CRC), who then shared the results with the patients. Notice of consent was place in the patient’s chart, along with pre-and postoperative orders. Study diaries were then given to all consenting patients.
Patient recruitment
Participants were recruited from among patients over 20 years of age planning elective primary unilateral total hip or knee replacement surgery at an orthopedic specialty hospital. Exclusion criteria are demonstrated in Table 2. There were no gender, ethnicity or race-based restrictions.
Surgical and postoperative care
Eleven orthopedic surgeons participated in this study. The surgical, anesthesia and postoperative procedures were according to the standardized procedures used in our hospital. Patients had early post-operative ambulation. All patients wore pneumatic compression stockings while in-patient. Elastic compression stockings were prescribed to be used after discharge until the follow-up ultrasounds. Hydroxyethyl starch (HES) 6 % was allowed intraoperatively for case specific reasons. Use of platelet function suppressive drugs, such a nonsteriodal anti-inflamatory drugs (NSAIDs), was discouraged but not prohibitied by the protool.
Laboratory monitoring
All patients receiving warfarin in hospital had PT measured daily. Thereafter, patients discharged on variable dose warfarin had PT measurements twice per week. Warfarin doses were prescribed by the hospital’s Coumadin Hotline personnel with target International Normalized Ratio (INR) 2.0–2.5. The patients on the 1 mg warfarin study arm had PT measured weekly. D-dimer was tested by flocculation and by quantitative assays upon admission and at the 28 ± 2 day follow-up visits with the results are reported as negative (0–500 μg/mL), indeterminate (500–1,000 μg/mL), or positive (>1,000 μg/mL). (Diagnostica Stago, American Bioproducts Co., Parsippany, New Jersey 07054).
Patient monitoring
Clinical Research Coordinators (CRCs) visited patients daily during inpatient hospitalization. After discharge the CRC’s called the patients weekly to monitor compliance and for any complications. The patients were met by the CRC’s again at the time of the follow-up ultrasound. Additionally, patients kept daily diaries of the doses and times of administration of their study drug along with any other drugs they were taking, and any complications and return visits to doctors or hospitals. Telephone interviews were conducted by the CRCs after 6 and 12 months to detect any delayed complications or VTE events.
Examination for deep vein thrombosis and pulmonary embolus
Patients underwent bilateral duplex sonography to evaluate any clinical suggestions of DVT or if asymptomatic on day 28 ± 2 following surgery. Gray scale, color, and spectral Doppler sonography with augmentation were performed of the bilateral common femoral veins, deep femoral veins, superficial femoral veins, popliteal veins, proximal greater saphenous veins, anterior and posterior tibial veins, and peroneal veins. Three highly trained technologists were involved in this study applied the Practice Guidelines and Technical Standards of the American College of Radiology, revised 2010. Ventilation/perfusion lung scan or computerized axial tomography angiogram was performed for evaluation of symptoms of pulmonary embolus. Radiology technicians and the radiologists were blinded to patient randomization.
Quality assurance
The Protocol Committee reviewed data weekly. The Data and Safety Monitoring Board (DSMB) examined blinded data every three months with authority to stop the study if deemed necessary.
Participant retention
Patients were removed from the study drug, but not from the study, if they reached a composite endpoint or if they elected to discontinue the study drug, including those patients who required change in their anticoagulation for ancillary medical reasons.
Protocol violations and adverse events
The Protocol Committee reviewed in blinded fashion all potential protocol violations and adverse events. The likelihood that there be a relationship between the reported events and the study drugs was assigned as being not related, unlikely related, possibly related, probably related or related. A major adverse event was defined as one that required medical or surgical intervention while in hospital, delayed discharge, or prompted return to office or hospital for reevaluation (whether or not intervention was required).
Hemorrhagic complications were classified as major or minor. A minor hemorrhage was one that was observed but required no intervention, such as epistaxis or venipuncture site hematoma. It may have been significant enough to warrant discharge delay or prompt a visit to the doctor or hospital, but with no intervention required. A major hemorrhage would include any fatal bleed or symptomatic bleed into critical area or organ requiring intervention.
Any major adverse event was reported to the IRB, DSMB and if required to the Federal Drug Administration.
Statistical methods
The study analysis was based upon intention to treat and thus all consented patients were included in the analysis. The primary analysis was based on a dichotomous outcome (i.e. VTE–yes/no) with VTE defined as the composite of DVT or PE or death. Estimates of how many patients were required in each arm to detect a difference were based on prior reported experiences in similar studies. With the goal to demonstrate equality for Arm C (upper one-sided 95 % confidence limit for treatment Arm C minus standard treatment arms A and B with the delta not to exceed 15 %), conservative estimates of DVT rates from prior studies and powered to 90 %, it was concluded that 110 patients were needed per group. As there were fewer endpoint events than expected in the three arms, the Odds Ratio was calculated for the composite endpoints using an exact logistic regression conditional analysis, a technique to be used when the outcomes variable have no observations. The non-inferiority analysis was completed using the Wald non-inferiority test.
A statistician analyzed the outcomes for differences between the study arms, differences within subsets (hip and knee arthroplasty), and differences within arms A, B and C for the primary and secondary endpoints. Multivariate analysis is reported for age, gender, body mass index (BMI), and use of hydroxyethyl starch or NSAIDs. Primary outcome data are stratified for hip vs. knee surgery, symptomatic vs. asymptomatic, and popliteal vein and above (proximal) vs. more distal veins. Secondary endpoints were analyzed for the patients as a total cohort. The p-values for all comparative results were calculated.
This was an open label, assessor-blinded study. All authors had access to the data.
Results
Patient recruitment, randomization and retention
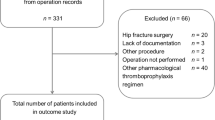
There were 3,860 patients were identified for this study by mailings. There was no response from 1,957 patients. Figure 1 demonstrates the flowchart for the remaining 1,903 patients.
Randomization was balanced between the three study arms for hip vs. knee surgery, and for gender, age, BMI and baseline blood studies. (see Tables 3, 4 and 5) Two patients had rheumatoid arthritis. Both were among the hip replacement patients. One of these had surgery for steroid induced avascular necrosis. All other patients had surgery for osteoarthritis.
Table 6 demonstrates the patients who withdrew completely from the study and those who withdrew from the study drug but completed the bilateral leg ultrasound as required by the protocol. All patients were included in the Intention to Treat analysis.
Prothrombin times reported as International Normalized Ratios (INR)
The INR’s on the day of surgery for patients in Arm C after taking 1.0 mg of warfarin for seven days were ≤ 1.3, with one exception to 1.5. (see Fig. 2) Fig. 3 demonstrates the INR results for patients in Arm A. Each was studied twice per week while on study and the warfarin dose was adjusted according to protocol guidelines. Fig. 4 demonstrates the weekly INR for all patients on Arm C. Five out of 322 INR results that were greater than 1.5.
Patients receiving HES or NSAIDs
Patients having hip replacement were more likely to be given HES compared to those having knee replacement. (p <0.05), but there were no differences among the three study arms. (see Table 7) There were no differences within the study groups relative to use of NSAID’s. (data available).
Protocol violations
There were 73 minor protocol violations and 24 major protocol violations, all equally distributed among the study arms (data available) No study violation was associated with an adverse event.
Composite endpoints
Complete bilateral leg ultrasounds were performed for 342 patients distributed equally in the study arms. (data available) There were no patients with VTE at time of discharge. Two patients in Arm C had delayed, asymptomatic, distal ultrasound-detected deep vein thrombosis. One of these patients had knee replacement surgery and the second had hip replacement surgery. They were discharged on days 4 and 5 post-operative respectively. There were no pulmonary emboli and no deaths. The p-values, the Exact Odds ratios with associated confidence limits, the non-inferiority analysis and the 95 % confidence limits are shown in Table 8.
Arm C was not to be different from Arms A and B. Because Arm C was non-inferior to Arms A or B, we analyzed equivalency between Arm C and the two arms using the Wald Method for the non-inferiority. Analysis of risk differences between the Arm C minus Arm A and Arm B showed that Arm C is also equivalent to both arm A and arm B, at an equivalency margin of 15 %. (p-value <0.0001; one-sided 95 % CI: -0.0428–0.0067) Thus, there are no statistical differences between Arm C and the other arms of the study.
Adverse events
There were no differences for the surgical estimated blood loss (EBL) or transfusions given among the three study groups. (data available) Patients taking NSAIDs did not have increased hemorrhagic complications. (data available) There were no surgery-related complications such as fracture, dislocation or infection.
More patients in Arm A reported a hemorrhagic event as compared to Arms B and C. The risk of reporting any hemorrhagic complication in Arm A was 1.29 times that of Arm B (95 % CI: 0.61–2.71), and was 1.54 times that of those in Arm C (95 % CI: 0.71–3.33). While there were differences for patients having knee replacement surgery these comparisons did not reach statistical significance for the study groups. (see Table 9) There were no differences of hemorrhagic complications using unadjusted and adjusted odds ratio related to study arm or related to hip vs. knee surgery, adjusted for effects of age, gender and use of HES and NSAID’s. (see Tables 10 and 11) One Arm C patient developed ischemic colitis complicated by gross hematochezia. Despite his taking only 1 mg warfarin daily the INR was prolonged. He was then found to have homozygous vitamin K epoxide reductase–1 (VKORC-1) genome disorder. The event was managed and he remained on study.
Four major adverse events occurred. Table 12 demonstrates the distribution of these events as being possibly related, probably related or related to study drugs. The two “probably related” leg hematomas occurred while the patients were in the hospital. The other two events occurred following discharge from the hospital.
D-dimer
Patients having knee replacement were more likely to have elevated D-dimer at the completion of the study compared to those having hip surgery. (p <0.0001) (see Table 13) There were no differences relative to the arms of the study. There were no delayed onset VTE events after 6 and 12 months from completion of study.
Discussion
Patients given no anticoagulants after hip or knee arthroplasty experience high rates of postoperative VTE [23–28]. Heretofore, commonly used anticoagulants reduced the frequency of postoperative VTE to 4–6 %. A meta-analysis of modern low molecular weight heparins, oral Xa inhibitors or oral IIa inhibitors included 47 clinical trials and observational studies involving 44,844 patients demonstrated rates of symptomatic DVT prior to discharge of 1.09 % for patients having TKA and 0.53 % for patients having THA, with heterogeneity of results among the included reports [29]. The current study shows that our fixed low dose warfarin regimen approximates the same level of benefit.
The two agents used in this current study as controls can be considered as among the available standards-of-care agents available for DVT prophylaxis. Variable dose warfarin has been used for many years, and is effective with the current target range of INR [30, 31]. Fondaparinux, a synthesized pentasaccaride with anti-factor Xa activity, was among the newer agents with VTE prophylaxis activity when this study was designed [22, 32–35].
As in our previous orthopedic studies and as with other investigators we selected a preoperative lead-time of 7 days for the fixed low dose warfarin used in this study [8, 11, 36, 37]. In an earlier central venous catheter study we choose 3 days [6]. We would not expect this low dose warfarin therapy to succeed if started following surgery, even though in one series it did succeed even when therapy was begun after central venous catheter insertion [12, 38–41].
There were two previous smaller but similarly structured studies that derived negative results for low dose warfarin following major orthopedic surgery. Poller, et al., in a report of 68 evaluable patients randomized to receive either warfarin 1 mg daily starting 7 days preoperatively or 5,000 units heparin starting 2 h preoperatively, with venography as the diagnostic tool [36]. Fordyce, et al., studied 148 patients having primary hip replacement surgery were randomized to take 1 mg warfarin starting 7 days prior to surgery or to be non-treated controls. Iodine-125 labeled fibrinogen uptake (with venography confirmation for positive femoral vein uptake) was used for detection of DVT [37].
Differences in outcomes may be dependent upon the DVT detection techniques applied. Color Doppler ultrasound was used in this study to detect DVT. Ultrasound imaging is accepted for diagnosing DVT with sensitivity and specificity for detection of proximal deep vein thrombosis is over 95 %. In studies of asymptomatic patients, the sensitivity the test has been variable. Nevertheless, a single negative complete lower limb examination is considered sufficient to exclude clinically important DVT [42–44]. New symptoms always require further imaging. In the current study patients were called at 6 and 12 months to detect any delayed symptomatic VTE events in order to detect any false negative results.
On the other hand, venography, often considered the gold standard for DVT detection studies, is far from the ideal diagnostic procedure. Venography-dependent studies often have significant numbers of patients who never get the venogram, have unilateral studies instead of bilateral studies, or are rejected by the adjudicating committees as technically inadequate [24, 45–50]. Venography also involves added risks for patients with allergic and renal reactions, skin necrosis if contrast dye extravasates and post-injection phlebitis in up to 2 % of patients in whom conventional ionic contrast agents are used. Even with use of lower osmolar contrast agents, minor side effects occur in about 20 % of patients undergoing venography. Fibrinogen scanning may have been supersensitive.
Also, the current study was performed in a hospital with a high volume of joint replacement surgery, wherein optimal non-pharmacologic DVT prophylaxis is also applied along with chemoprophylaxis. Patients are told to discontinue smoking and estrogen supplements prior to surgery, to walk the day of surgery, and wear bilateral pneumatic compression stockings in hospital followed by elastic compression stockings after discharge until follow-up visits. Perhaps some of these elements may contribute to differences between the study outcomes.
There are clinically relevant elements within any study that cannot be stratified or controlled. In this study tourniquets were used for all patients having knee replacement, and it is assumed that the time the tourniquets were applied was equal for each study group [50]. Volume expansion by crystalloids can influence post-operative coagulation; it is assumed that the volume expansions were equivalent for each study group [51]. HES can have effects upon the clotting system [52, 53]. There were no differences for the use of HES among the three arms of this study. Also, as there are over 100 drugs, foods and supplements reported to interfere with platelet function, with unclear clinical significance for most, it would have been difficult to control for all of these agents [54]. It was decided by the protocol writing committee to track and analyze six of the more commonly used NSAIDs.
A positive D-dimer assay after conclusion of therapy for acute DVT or PE has been previously reported to be predictive of relapse of VTE. In one such study following one month of therapy for DVT, 39 % of patients had elevated D-dimer and seven of these patients went on to have recurrent VTE [55]. There is also increasing recognition that longer prophylactic therapy is beneficial in the post-operative setting [56–62]. The current study prescribed that all study patients have measurements of D-dimer at the end of the treatment. No patient had delayed onset VTE when called 6 months and 12 months following completion of one month of therapy. Thus, in this study a positive D-dimer at the conclusion of therapy had no predictive value for delayed onset VTE after prolonger therapy of one month.
This proof of concept study builds upon prior studies examining low dose schedules for postoperative VTE chemoprophylaxis with warfarin. Trail limitations include that this is a single institution, open label but assessor-blind study study. A similar multi-institutional study with a larger number of patients would be welcomed. Perhaps it would also be useful to attempt the next such study with combined Doppler ultrasound and venography detection for DVT to confirm adequacy of Doppler ultrasound.
In conclusion, the three regimens in this study offer effective prophylaxis against thromboembolic disease following elective arthroplasty of hips and knees. It appears that fixed low dose warfarin when used as described is equivalent to two of the more intense regimens. By extending postoperative anticoagulation to four weeks there appears to be less chance for delayed VTE, even if there is a positive D-dimer at conclusion of treatment. Each regimen carries some risk and some inconvenience for the patient. The fixed low dose warfarin regimen herein described saves the patients the inconvenience of multiple blood draws, but does not eliminate that need completely, as demonstrated in our patient with vitamin K epoxide reductase genome disorder. Nevertheless, it should carry minimal hemorrhagic potential and require reduced laboratory support. It should be less expensive and easier to administer than other protocols using anti-Xa and anti-IIa agents, which has implications for health care costs.
References
Baptiste G, Bern MM, Bothe Jr A, Bistrian BR, Blackburn G. Low Antithrombin III in morbid obesity: improved levels following weight loss. J Parenter Enteral Nutr. 1983;7:447–9.
Bern MM, Bothe Jr A, Bistrian B, Batiste G, Haywood E, Blackburn G. Effects of low-dose warfarin on antithrombin III levels in morbidly obese patients. Surgery. 1983;94:78–83.
Francis CW, Marder VJ, Evarts CM, Yaukoolbodi S. Two-step warfarin therapy. Prevention of postoperative venous thrombosis without excessive bleeding. JAMA. 1983;249:374–8.
Bern MM, Bothe A, Bistrian B, Champagne CD, Keane MS, Blackburn G. Prophylaxis against central vein thrombosis with low-dose warfarin. Surgery. 1986;99:216–21.
Poller L, McKernan A, Thomson JM, Elstein M, Hirsh PJ, Jones JB. Fixed minidose warfarin: a new approach to prophylaxis against venous thrombosis after major surgery. Br Med J (Clin Res Ed). 1987;295:1309–12.
Bern MM, Lokich JJ, Wallach SR, Bothe Jr A, Benotti PN, Arkin CF, Greco FA, Huberman M, Moore C. Very low doses of warfarin can prevent thrombosis in central venous catheters. Ann Int Med. 1990;112:423–8.
MacCallum PK, Thomson JM, Poller L. Effects of fixed minidose warfarin on coagulation and fibrinolysis following major gynaecological surgery. Thromb Haemost. 1990;64:511–5.
Bern MM, Bierbaum B, Wetzner S, Brennan W, McAlister S. Very low dose warfarin as prophylaxis against ultrasound detected deep vein thrombosis following primary hip replacement. Am J Hemat. 2002;7:69–74.
Mismetti P, Mille D, Laporte S, for the CIP Study Group. Low-molecular weight heparin (nadroparin) and very low doses of warfarin in the prevention of upper extremity thrombosis in cancer patients with indwelling long-term central venous catheters: A pilot randomized trial. Haematologica. 2003;88:67–74.
Vives MJ, Hozack WJ, Sharkey PF, Moriarty L, Sokoloff B, Rothman RH. Fixed minidose versus adjusted low-dose warfarin after total joint arthroplasty: a randomized prospective study. J Arthroplasty. 2001;16:1030–7.
Bern MM, Deshmukh RV, Nelson R, Bierbaum BE, Sevier N, Howie N, Losina E, Katz JN. Low-dose warfarin coupled with lower leg compression is effective prophylaxis against thromboembolic disease after hip arthroplasty. J Arthroplasty. 2007;22:644–50.
Lavau-Denes S, Lacroix P, Maubon A, Preux PM, Genet D, Vénat-Bouvet L, Labourey JL, Martin J, Slaouti P, Tubiana-Mathieu N. Prophylaxis of catheter-related deep vein thrombosis in cancer patients with low-dose warfarin, low molecular weight heparin, or control: a randomized, controlled, phase III study. Cancer Chemother Pharmacol. 2013;72:65–73.
Holm J, Berntorp E, Carlsson R, Erhardt L. Low-dose warfarin decreases coagulability without affecting prothrombin complex activity. J Intern Med. 1993;234:303–8.
Boraks P, Seale J, Price J, Bass G, Ethell M, Keeling D, Mahendra P, Baglin T, Marcus R. Prevention of central venous catheter associated thrombosis using minidose warfarin in patients with haematological malignancies. Br J Haematol. 1998;101:483–6.
Bach AU, Anderson SA, Foley AL, Williams EC, Suttie JW. Assessment of vitamin K status in human subjects administered “minidose” warfarin. Am J Clin Nutr. 1996;64:894–902.
Uehara S, Gotoh K, Handa H, Honjo K, Hirayama A. Process of carboxylation of glutamic acid residues in th Gla domain of human des-gamma-carboxyprothrombin. Clin Chim Acta. 1999;289:33–44.
Stenflo J, Fernlurd P, Egon W, Roepstorff P. Vitamin K-dependent modification of glutamic acid residues in prothrombin. Proc Natl Acad Sci U S A. 1974;71:2730–3.
Tuhy PM, Bloom JW, Mann KG. Decarboxylation of bovine prothrombin fragment 1 and prothrombin. Biochemistry. 1979;18:5842–8.
Furie B, Furie BC. The molecular basis of blood coagulation. Cell. 1988;53:505–18.
Colpitts TL, Prorok M, Castellino FJ. Binding of calcium to individual gamma-carboxyglutamic acid residues of human protein C. Biochemistry. 1995;34:2424–30.
Ratcliffe JV, Furie B, Furie BC. The importance of specific gamma-carboxyglutamic acid residues in prothrombin. J Biol Chem. 1993;268:24339–45.
Rachidi S, Aldin ES, Greenberg C, Sachs B, Streiff M, Zeidan AM. The use of novel oral anticoagulants for thromboprophylaxis after elective major orthopedic surgery. Expert Rev Hematol. 2013;6:677–95. doi:10.1586/1747408.
Anderson Jr FA, Wheeler HB, Goldberg RJ, Hosmer DW, Patwardhan NA, Jovanovic B, Forcier ADalen JE. A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism. The Worcester DVT Study. Arch Intern Med. 1991;151:933–8.
Piovella F, Wang CJ, Lu H, Lee K, Lee LH, Turpie AGG, Gallus AS, Planes A, Passera R Rouillon A for the AIDA Investigators. Deep-vein thrombosis rates after major orthopedic surgery in Asia. An epidemiological study based on postoperative screening with centrally adjudicated bilateral venography. J Thromb Haemost. 2005;3:2664–70.
Turpie AG, Levin MN, Hirsh J, Carter CJ, Jay RM, Powers PJ, Andrew M, Hull RD, Gent M. A randomized controlled trial of low molecular–weight heparin (enoxaparin) to prevent deep vein thrombosis in patients undergoing elective hip surgery. N Eng J Med. 1986;315:925–9.
Hoek JA, Nurmohamed MT, Hamelyck KJ, Marti RK, Knipscheer HC, ten Cate H, Büller HR, Magnani HN, ten Cate JW. Prevention of deep vein thrombosis following total hip replacement by low molecular weight heparinoid. Thrombo Haemost. 1992;67:28–32.
McKenna K, Bachmann F, Kaushal SP, Galante JO. Thromboembolic disease in patients undergoing knee replacement. J Bone Joint Surg Am. 1976;58:928–32.
Stulberg BN, Insal JN, Willaims GW, Ghelman B. Deep-vein thrombosis following total knee replacement. An analysis of six hundred and thirty-eight arthroplasties. J Bone Joint Surg Am. 1984;66:194–201.
Januel JM, Chen G, Ruffieux C, Quan H, Douketis JD, Crowther MA, Colin C, Ghali WA, Burnand B; IMECCHI Group. Symptomatic in-hospital deep vein thrombosis and pulmonary embolism following hip and knee arthroplasty among patients receiving recommended prophylaxis: a systematic review. JAMA. 2012;307:294–303.
Enyart JJ, Jones RJ. Low-dose warfarin for prevention of symptomatic thromboembolism after orthopedic surgery. Ann Pharmacother. 2005;39:1002–7.
Kwong LM. Comparative safety and efficacy of antithrombotics in the management of venous thromboembolism after knee and hip replacement surgery: focus on rivaroxaban. Clin Pharmacol. 2013;5:143–8.
Turpie AG, Bauer KA, Eriksson BI, Lassen MR. Fondaparinux vs enoxaparin for prevention of venous thromboembolism in major orthopaedic surgery: a meta-analysis of 4 randomized double-blind studies. Arch Intern Med. 2002;162:1833–40.
Eriksson BI, Bauer KA, Lassen MR, Turpie AG, Steering Committee for of the Pentasaccaride in Hip-Fracture Study Group. Fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after hip fracture surgery. N Engl J Med. 2001;345:1298–304.
Bauer KA, Eriksson BI, Lassen MR, Turpie AG, Steering Committee for of the Pentasaccaride in Hip-Fracture Study Group. Fondaparinux compared to enoxaparin for the prevention of venous thromboembolism after elective knee surgery. N Engl J Med. 2001;345:1305–10.
Tran AH, Lee G. Fondaparinux for prevention of venous thromboembolism in major orthopedic surgery. Ann Pharmacother. 2003;37:1632–43.
Poller L, Thomson JM, MacCallum PK, Nicholson DA, Weighill FJ, Lemon JG. Minidose warfarin and failure to prevent deep vein thrombosis after joint replacement surgery despite inhibiting the postoperative rise in plasminogen activator inhibitor activity. Clin Appl Throm Hemost. 1995;1:267–73.
Fordyce MJ, Baker AS, Staddon GE. Efficacy of fixed minidose warfarin prophylaxis in total hip replacement. BMJ. 1991;303:219–20.
Heaton DC, Han DY, Inder A. Minidose (1mg) warfarin as prophylaxis for central vein catheter thrombosis. Int Med J. 2002;3:84–8.
Couban D, Goodyear M, Burnell M, Dolan D, Wasi P, Barnes D, Macleod D, Burton E, Andreou P, Anderson DR. Randomized placebo-controlled study of low-dose warfarin for the prevention of central venous catheter-associated thrombosis in patients with cancer. J Clin Oncol. 2005;23:4063–9.
Young AM, Billingham LJ, Begum G, Kerr DJ, Hughes AI, Rea DW, Shepherd S, Stanley A, Sweeney A, Wilde J, Wheatley K, WARP Collaborative Group, UK. Warfarin thromboprophylaxis in caner patient with central venous catheters (WARP): an open-label randomized trial. Lancet. 2009;373:567–74. doi:10.1016/S0140-6736(09)60205-1.
Ruud E, Holmstrøm H, De Lange C, Hogstad EM, Wesenberg F. Low-dose warfarin for the prevention of central line-associated thrombosis in children with malignancies—a randomized, controlled study. Acta Paediatr. 2006;95:1053–9.
Wells PS, Anderson DR, Bormanis J, Guy F, Mitchell M, Gray L, Clement C, Robinson KS, Lewandorski B. Value of assessment of pretest probability of deep-vein thrombosis in clinical management. Lancet. 1997;350:1795–8.
Fraser JD, Anderson DR. Deep vein thrombosis: recent advances and optimal investigation with US. Radiology. 1999;211:9–14.
Subramaniam RM, Heath R, Chou T, Cox K, Davis G, Swarbrick M. Deep venous thrombosis: withholding anticoagulation therapy after negative complete lower limb US findings. Radiology. 2005;237:348–52.
Bergqvist D, Benoni G, Björgell O, Fredin H, Hedlundh U, Nicolas S, Nisson P, Nylander G. Low-molecular-weight heparin (enoxaparin) as prophylaxis against venous thromboembolism after total hip replacement. N Engl J Med. 1996;335:696–700.
Planes A, Vochelle N, Fagola M, Bellaud M. Comparison of two low-molecular-weight heparins for the prevention of postoperative venous thromboembolism after elective hip surgery. Reviparin Study Group. Blood Coagul Fibrinolysis. 1998;9:499–505.
Eriksson BI, Ekman S, Kalebo P, Zachrisson B, Bach D, Close P. Prevention of deep-vein thrombosis after total hip replacement: direct thrombin inhibition with recombinant hirudin, CGP 39393. Lancet. 1996;347:635–9.
Hull RD, Pineo GF, Francis C, Bergqvist D, Fellenius C, Soderberg K, Holmqvist A, Mant M, Dear R, Baylis B, Mah A, Brant R. Low-molecular-weight heparin prophylaxis using dalteparin in close proximity to surgery vs. warfarin in hip arthroplasty patients: a double- blind, randomized comparison. The North American Fragmin Trial Investigators. Arch Int Med. 2000;160:2199–207.
Leclerc JR, Geerts WH, Desjardins L, Laflamme GH, L’Espérance B, Demers C, Kassis J, Cruickshank M, Whitman L, Delorme F. Prevention of venous thromboembolism after knee arthroplasty. A randomized, double-blind trial comparing enoxaparin with warfarin. Ann Int Med. 1996;124:619–26.
Aglietti P, Baldini A, Vena LM, Abbate R, Fedi S, Falciani M. Effect of tourniquet use on activation of coagulation in total knee replacement. Clin Orthop Relat Res. 2000;169–177.
Weiss G, Lison S, Spannagl M, Heindl B. Expressiveness of global coagulation parameters in dilutional coagulopathy. Br J Anaesth. 2010;105:429–36.
Schramko A, Suojaranta-Ylinen R, Kuitunen A, Raivio P, Kukkonen S, Niemi T. Hydroxyethylstarch and gelatin solutions impair blood coagulation after cardiac surgery: a prospective randomized trial. Br J Anaesth. 2010;104:691–7.
Haisch G, Boldt J, Krebs C, Suttner S, Lehmann A, Isgro F. Influence of a new hydroxyethylstarch preparation (HES 130/0.4) on coagulation in cardiac surgical patients. J Cardiothorac Vasc Anesth. 2011;25:755–7.
Konkle B. Acquired disorders of platelet function. American Society of Hematology: Hematology; 2011. p. 391–6.
Kuruvilla J, Wells PS, Morrow B, MacKinnon K, Keeney M, Kovacs MJ. Prospective assessment of the natural history of positive D-dimer results in persons with acute venous thromboembolism (DVT or PE). Thromb Haemost. 2003;89:284–7.
Prandoni P, Bruchi O, Sabbion P, Tanduro C, Scudeller A, Sardella C, Errigo G, Pietobelli F, Maso G, Girolami A. Prolonged thromboprophylaxis with oral anticoagulants after total hip arthroplasty: a prospective controlled randomized study. Arch Intern Med. 2002;162:1966–71.
Eriksson BI, Lassen MR, for the PENTasaccharide in Hip-Fracture Surgery Investigators. Duration of prophylaxis against venous thromboembolism with fondaparinux after hip fracture surgery. Arch Intern Med. 2003;163:1337–42.
Cohen AT, Bailey CS, Alikhan R, Cooper DJ. Extended thromboprophylaxis with low molecular weight heparin reduces symptomatic venous thromboembolism following lower limb arthroplasty-a meta-analysis. Thromb Haemost. 2001;85:940–1.
Sobieraj DM, Lee S, Coleman CI, Tongbram V, Chen W, Colby J, Makanji S, Ashaye AO. Prolonged versus standard-duration venous thromboprophylaxis in major orthopedic surgery. Ann Intern Med. 2012;156:720–7.
Eriksson BI. Improvements in the prevention of postoperative venous thromboembolism in hip fracture patients. Orthopedics. 2003;26 suppl 8:s851–8.
Turpie AG. Fondaparinux: a factor Xa inhibitor for antithrombotic therapy. Expert Opin Pharmacother. 2004;5:1373–84.
Cohen AT, Khushal A. Extended thromboprophylaxis following lower limb arthroplasty: what do the clinical trials mean? Haemostasis. 2000;30 suppl 2:88–94.
Acknowledgements
We acknowledge the additional statistical analysis by John Griffith, PhD and Ling Li, MPH. Elizabeth Stroch provided editorial review, supported by the Department of Orthopedic Surgery, New England Baptist Hospital. Funding sources for this study included the New England Baptist Hospital and its Elizabeth Alexander Stent Fund, The Cancer Center Research Foundation and The Foundation for Hematology Research. These organizations had no input into the design and conduct of this study; collection, management, analysis and interpretation of the data; or preparation, review or approval of this manuscript. Material support for this study came from the supplier of fondaparinux, GlaxoSmithKline, which was aware of the study, but had no input into the study conception, design, conduct, analysis, or interpretation of the study data; nor preparation, statistical analysis, review or approval of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
There are no conflicts of interest for any author regarding any part of this work.
Authors’ contributions
Each co-author made substantial contributions to this study. Each co-author participated in the design of the protocol. MMB, DMW, DH, ED, DJS and RHB participated in the acquisition, analysis and interpretation of the data. DAM, JVB and DMW participated in the recruiting of patients. LH conducted the statistical analysis. Drafting and revising the manuscript for intellectual content was shared by all co-authors. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Bern, M.M., Hazel, D., Deeran, E. et al. Low dose compared to variable dose Warfarin and to Fondaparinux as prophylaxis for thromboembolism after elective hip or knee replacement surgery; a randomized, prospective study. Thrombosis J 13, 32 (2015). https://doi.org/10.1186/s12959-015-0062-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12959-015-0062-0