Abstract
Background
In the current NCCN guidelines, the prognosis and adjuvant chemotherapy of patients who underwent neoadjuvant chemoradiotherapy (nCRT) are based on pre-radiotherapy clinical TNM (cTNM) stage. However, the value of neoadjuvant pathologic TNM (ypTNM) stage is not clearly described.
Methods
This retrospective study investigated the prognosis and adjuvant chemotherapy which based on ypTNM stage compared to cTNM stage. Between 2010 and 2015, a total of 316 rectal cancer patients who underwent nCRT, followed by total mesorectal excision (TME), were included for analysis.
Results
Our findings revealed that cTNM stage was the only significant independent factor in the pCR group (HR = 6.917, 95% CI: 1.133–42.216, P = 0.038). In the non-pCR group, ypTNM stage was more important than cTNM stage in prognosis (HR = 2.704, 95% CI: 1.811–4.038, P < 0.001). In ypTNM III stage group, there was a statistically significant difference in prognosis between the patients with and without adjuvant chemotherapy (HR = 1.943, 95% CI: 1.015–3.722, P = 0.040), but there was no significant difference in cTNM III stage group (HR = 1.430, 95% CI: 0.728–2.806, P = 0.294).
Conclusions
We concluded that ypTNM stage, rather than cTNM stage, might be a more important factor in the prognosis and adjuvant chemotherapy of patients with rectal cancer who underwent nCRT.
Similar content being viewed by others
Background
The worldwide incidence of colorectal cancer (CRC) is high [1]. In recent years, the prevalence of CRC has been increasing in part because of an aging population. Among the different types of CRC, nearly 50% are rectal cancers [2]. Many studies have demonstrated that neoadjuvant chemoradiotherapy (nCRT) is effective in reducing local recurrence and preserving the anal sphincter [3, 4]. Therefore, nCRT has become the standard treatment for locally advanced rectal cancer, according to National Comprehensive Cancer Network (NCCN) guidelines [5]. However, the response to nCRT varies from pathological complete response (pCR) to disease progression. According to previous studies, approximately 30% of rectal cancer patients who underwent nCRT showed complete response and approximately 60% showed tumor size regression and N stage descension [6,7,8,9]. Due to individual differences in response to nCRT, the tumor stage of patients might vary greatly. In the current NCCN guidelines, the prognosis and adjuvant chemotherapy of patients with nCRT are based on pre-radiotherapy clinical TNM (cTNM) stage. However, the value of neoadjuvant pathologic TNM (ypTNM) stage is not clearly described. Therefore, the aim of this study was to investigate cTNM and ypTNM stages, which was a more important factor in the prognosis and adjuvant chemotherapy of patients with rectal cancer.
Methods
Patients
Between 2010 and 2015, we retrospectively analyzed 316 rectal cancer patients who received nCRT, followed by total mesorectal excision (TME) at the Liaoning Cancer Hospital and Institute. Before nCRT, all patients were histologically confirmed to have resectable rectal cancer of clinical T2-4aN0-2M0 stage, according to the 8th edition of the UICC/AJCC TNM classification system. Histological specimens for ypTNM stage were evaluated by two senior pathologists. Patients were excluded if they were diagnosed with unresectable cancer after nCRT, underwent nCRT at other hospitals, died during the peri-operative period, or had incomplete records.
All patients were followed-up for more than 5 years after the surgery. The preoperative staging evaluation included physical and laboratory examinations, enteroscopy with endoscopic ultrasound and pathological biopsy, chest and abdominal computed tomography (CT), and pelvic magnetic resonance imaging (MRI). Most patients were discussed by a multidisciplinary team (MDT) before starting treatment. This study was approved by the Ethics Committee of the Liaoning Cancer Hospital & Institute (NO: 202,204,117) and in accordance with its relevant guidelines and regulations.
Treatment
All patients were treated with intensity-modulated radiation therapy (IMRT) and volumetric-modulated arc therapy (VMAT) with a minimal photon energy of 6 MV. As for standard dose, after 45 Gy a tumor bed boost with a 2 cm margin of 5.4 Gy in 3 fractions could be considered. Concurrent chemotherapy consisted oral capecitabine (825 mg/m2/d twice daily, 5 days a week) during the five weeks of radiotherapy. The mFOLFOX regimen was followed for 1–2 cycles of consolidation chemotherapy during the interval period after the chemoradiotherapy. TME would be performed 2–4 weeks after the end of consolidation chemotherapy. In general, the patients underwent TME after 6 to 8 weeks of nCRT. During the surgery, we tried to preserve the left colon vessels and made a preventive stoma as much as possible. According to NCCN guidelines, patients with cTNM III stage should be treated with mFOLFOX (oxaliplatin + 5-FU + calcium folinate) as adjuvant chemotherapy. However, due to various reasons, some patients did not receive chemotherapy. A pCR was defined as the absence of residual tumor in the entire rectal wall and local lymph nodes. Non-pCR was defined as the presence of residual tumor, either in the rectal wall or local lymph nodes.
Follow-up
All patients were followed up by telephone interviews or outpatient visits. Patients were followed-up every 3 to 6 months in the first two years and then once per year. At each follow-up, tests included anal examinations, tumor marker levels, abdomen and lung CT, and/or MRI and colonoscopy, if needed. The primary endpoint was overall survival (OS). OS was defined from the day of the surgery to the death of the patient for any reason.
Statistical analysis
SPSS 22.0 software (IBM, Armonk, NY, USA) was used for statistical analysis. The χ2 test or Fisher’s exact test was used to compare categorical variables. The Kaplan–Meier method was used to assess OS. The Cox proportional hazards regression model was used in forward stepwise multivariate survival analysis. To investigate which TNM stage (cTNM or ypTNM stage) was more important in predicting the prognosis, two-step multivariate survival analysis was used. In step 1 multivariate analysis, all statistically significant prognostic factors from the univariate analysis were included, except for ypTNM stage. In step 2 multivariate analysis, ypTNM stage was also considered, together with statistically significant prognostic factor in step 1. P < 0.05 was considered statistically significance.
Results
Patient characteristics and follow-up
Patient particulars and clinicopathological characteristics are provided in Table 1. A total of 316 patients with rectal cancer who met the criteria were included in the analysis. The median age was 58 years (range, 16–84 years). All patients underwent TME after nCRT. After histopathological examination, 70 patients (22.2%) achieved pCR, and the remaining patients with residual cancer were classified as the non-pCR group (n = 246). Patients with smaller primary tumors, exophytic type cancer and lower cTNM stage were more likely to achieve pCR after nCRT (P < 0.001 for all) (Table 1).
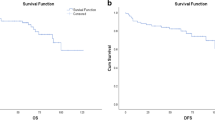
The median follow-up time was 47 months (range, 12–101 months) for the 316 rectal cancer patients. At the time of the last follow-up, 73 patients (23.1%) had died due to tumor progression and all patients experienced recurrence: five patients (1.6%) in the pCR group, including 2 cases of local recurrence and 3 cases of distant recurrence, and 68 patients (21.5%) in the non-pCR group, including 12 cases of local recurrence, 42 cases of distant recurrence and 14 cases of concurrent recurrence. One patient died due to an accident. The 5-year OS was 91.5% in the pCR group and 64.1% in the non-pCR group. The OS of the pCR group was better than that of the non-pCR group (HR = 5.083, 95% CI: 2.047–12.627, P < 0.001) (Fig. 1).
Prognostic features of nCRT patients
Univariate and/or multivariate analyses of the prognostic factors in pCR and non-pCR groups are provided in Tables 2 and 3, respectively. Univariate analyses showed that primary tumor diameter (P = 0.023) and cTNM stage (P = 0.015) entered into multivariate analysis in the pCR group. Moreover, multivariate analysis demonstrated that cTNM stage was the only significant independent factor (HR = 6.917, 95% CI: 1.133–42.216, P = 0.038). For the non-pCR group, histologic differentiation (P = 0.052), cTNM stage (P = 0.021), and ypTNM stage (P < 0.001) were associated with the prognosis of patients who underwent nCRT. To determine which factor (histologic differentiation, cTNM stage, or ypTNM stage) was the most important in predicting the prognosis, two-step multivariate analysis was applied (Table 4). In step 1, the significant factors (histologic grade and cTNM stage) from the univariate analysis were considered, except for ypTNM stage, and cTNM stage was confirmed to be an independent factor in predicting a better prognosis (HR = 1.811, 95% CI: 1.084–3.025, P = 0.023). In step 2, when ypTNM stage was considered, ypTNM stage rather than cTNM stage became the most important prognostic factor (HR = 2.704, 95% CI: 1.811–4.038, P < 0.001). In other words, ypTNM stage was a more important prognostic factor than cTNM stage.
Adjuvant chemotherapy for nCRT patients
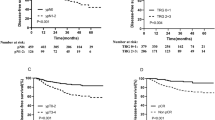
Due to adjuvant chemotherapy is mostly performed in patients with TNM III stage, we performed prognostic analysis in cTNM III and ypTNM III stage group, respectively.
In cTNM III stage group, 115 patients (79.9%) received adjuvant chemotherapy and 29 patients (20.1%) received no chemotherapy, including 18 patients with ypTNM III stage. Patients with adjuvant chemotherapy had a trend of better prognosis than without adjuvant chemotherapy with 5-year OS rates of 60.1% versus 52.8%, but there was no significant statistical difference (HR = 1.430, 95% CI: 0.728–2.806, P = 0.294) (Fig. 2). Furthermore, in ypTNM III stage group, 5-year OS rates of patients with adjuvant chemotherapy had better than patients without adjuvant chemotherapy (54.6% versus 30.5%, and HR = 1.943, 95% CI: 1.015–3.722, P = 0.040) (Fig. 3).
Discussion
According to the current NCCN guidelines, the adjuvant treatment and prognosis of rectal cancer after surgery are based on pre-radiotherapy cTNM stage [10]. In this study, we found that ypTNM stage might be a more accurate factor to reflect the prognosis and guiding adjuvant therapy of rectal cancer patients who underwent nCRT. Many studies have also reported the importance of the neoadjuvant pathological stage in the prognosis of patients. Sun et al. [11] investigated 317 rectal cancer patients who underwent radical surgical resection following nCRT and observed that ypTNM stage was the only independent risk factor in these patients. Similarly, Kim et al. [12] reported that ypTNM stage was an important prognostic factor in the prediction of local recurrence and distant metastasis in rectal cancer patients. Since the TNM stage of patients might vary greatly after nCRT, there might be significant variations in prognosis based on cTNM stage. Therefore, we concluded that ypTNM stage might better reflect the prognosis of patients than cTNM stage.
NCCN guidelines recommend adjuvant treatment for patients with cT3-4N0 and cT1-3N1-2 stage after nCRT. Is it suitable? We all known that the response to nCRT varies from pCR to disease progression due to individual differences in response to nCRT. Whether ypTNM stage after nCRT is more accurate in guiding adjuvant therapy than cTNM stage is worth studying. A multicenter randomized controlled clinical study confirmed that oxaliplatin + 5-FU combination chemotherapy can significantly improve the 3-year disease-free survival of patients with ypTNM stage III rectal cancer compared with 5-FU chemotherapy alone, but it had no effect on the prognosis of patients with ypTNM stage II rectal cancer [13]. You et al. [14] performed a retrospective study of 160 rectal cancer patients and observed that adjuvant chemotherapy might not improve the survival of ypT0-2N0 patients but might be meaningful for ypT3-4N0 patients in terms of the 5-year OS. These studies indicated that ypTNM stage had important value in guiding adjuvant therapy. In our study, the patients with adjuvant chemotherapy had a better prognosis than the patients without adjuvant chemotherapy in ypTNM III stage group, but there was no statistical difference in cTNM III stage. Therefore, we concluded that adjuvant therapy based on ypTNM stage might be more accurate.
The main advantage of our study was that we investigate the value of ypTNM stage from both treatment and prognosis. However, there were several limitations in the current study. First, the sample size was relatively small, which contributed to the low statistical power of the prognostic comparisons. Second, because of the nature of retrospective studies, selectivity bias was inevitable. Therefore, further studies should be carried out to confirm our results.
In conclusion, our study showed that ypTNM stage might be a more accurate factor to reflect the prognosis and guiding adjuvant therapy of patients with rectal cancer who underwent nCRT, which was not clearly pointed out in the current NCCN guidelines.
This study provides evidence of more accurate therapy and prognosis after nCRT. For further research, we are currently conducting a large multicenter retrospective study.
Availability of data and materials
Not applicable.
Abbreviations
- nCRT:
-
Neoadjuvant chemoradiotherapy
- cTNM:
-
Clinical TNM
- ypTNM:
-
Neoadjuvant pathologic TNM
- CRC:
-
Colorectal cancer
- NCCN:
-
National Comprehensive Cancer Network
- pCR:
-
Pathological complete response
- TME:
-
Total mesorectal excision
- CT :
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- MDT:
-
Multidisciplinary team
- IMRT:
-
Intensity-modulated Radiation Therapy
- VMAT:
-
Volumetric-modulated Arc Therapy
- OS:
-
Overall survival
References
Provenzale D, Jasperson K, Ahnen DJ, et al. Colorectal Cancer Screening, Version 1. J Natl Compr Canc Netw. 2015;13(8):959–68.
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Sauer R, Becker H, Hohenberger W, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004;351(17):1731–40.
Rosa C, Di Tommaso M, Caravatta L, et al. Assessment of bowel and anal sphincter function after neoadjuvant chemoradiotherapy in locally advanced rectal cancer. Tumori. 2018;104:121–7.
Benson AB, Venook AP, Al-Hawary MM, et al. Rectal cancer, version 2. NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2018;16:874–901.
Yamashita K, Matsuda T, Hasegawa H, et al. Recent advances of neoadjuvant chemoradiotherapy in rectal cancer: Future treatment perspectives. Ann Gastroenterol Surg. 2019;3:24–33.
Goffredo P, Khan A, Mott SL, et al. Total neoadjuvant therapy versus standard neoadjuvant chemoradiation in patients with locally advanced rectal cancer: a comparison of short- and long-term oncologic outcomes. Ann Surg. 2021;276:e819–24.
Sun Z, Adam MA, Kim J, Shenoi M, Migaly J, Mantyh CR. Optimal timing to surgery after neoadjuvant chemoradiotherapy for locally advanced rectal cancer. J Am Coll Surg. 2016;222:367–74.
Ryan JE, Warrier SK, Lynch AC, Ramsay RG, Phillips WA, Heriot AG. Predicting pathological complete response to neoadjuvant chemoradiotherapy in locally advanced rectal cancer: a systematic review. Colorectal Dis. 2016;18:234–46.
Benson AB, Venook AP, Al-Hawary MM, Azad N, Chen YJ, Ciombor KK, et al. Rectal cancer, version 2. NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2022;20:1139–67.
Sun Y, Chi P, Lin H, et al. Analysis of risk factors of distant metastasis in rectal cancer patients who received total mesorectal excision following neoadjuvant chemoradiotherapy. Zhonghua Wei Chang Wai Ke Za Zhi. 2016;19(4):436–41.
Kim CH, Lee SY, Kim HR, Kim YJ. Pathologic stage following preoperative chemoradiotherapy underestimates the risk of developing distant metastasis in rectal cancer: A comparison to staging without preoperative chemoradiotherapy. J Surg Oncol. 2016;113(6):692–9.
Hong YS, Nam BH, Kim KP, et al. Oxaliplatin, fluorouracil, and leucovorin versus fluorouracil and leucovorin as adjuvant chemotherapy for locally advanced rectal cancer after preoperative chemoradiotherapy (ADORE): an open-label, multicentre, phase 2, randomised controlled trial. Lancet Oncol. 2014;15(11):1245–53.
You KY, Huang R, Ding PR, et al. Selective use of adjuvant chemotherapy for rectal cancer patients with ypN0. Int J Colorectal Dis. 2014;29(4):529–38.
Acknowledgements
We would like to thank Dr. Rui Zhang for critical revision.
Funding
This work was supported by Shenyang Young and Middle-aged Scientific and Technological Innovation Talents Support Project (RC190487); Health Development Promotion Project (BJHA-CRP-019).
Author information
Authors and Affiliations
Contributions
Yue Chen collected documents and wrote the paper. Deyu Sun managed the design and modified the paper. Jiayu Sun and Xinxin Dong collected documents and assisted in writing discussion section. Yanli Qu modified the paper.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the local ethics committee of Liaoning Cancer Hospital & Institute.
Consent for publication
All presentations had consent for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, Y., Sun, J., Dong, X. et al. Significance of ypTNM stage in determining the prognosis and therapy after surgery for locally advanced rectal cancer. World J Surg Onc 21, 174 (2023). https://doi.org/10.1186/s12957-023-03059-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-023-03059-w