Abstract
Objective
Coronary artery ectasia (CAE) is a condition characterized by the localized or widespread dilation of one or more coronary arteries. The majority of CAE patients do not present with clinical symptoms, and the exact cause of CAE remains unclear. Therefore, a retrospective analysis was conducted to explore the potential causes of CAE.
Methods
This study was a retrospective analysis of patients who underwent coronary angiography at Guangdong Provincial People’s Hospital between January 2017 and July 2022, of whom 679 patients were ultimately enrolled in the study. Among them, 260 patients were diagnosed with CAE, whereas 419 patients with normal coronary results composed the control group. Remnant cholesterol (RC) was calculated as total cholesterol (TC) minus high-density lipoprotein cholesterol (HDL-C) minus low-density lipoprotein cholesterol (LDL-C). The association between RC levels and the risk of CAE was assessed via multivariable logistic models.
Results
Out of the 679 patients who participated in this study, with an average age of 59.9 years, 38.3% were diagnosed with CAE. Patients with CAE had higher RC levels than did those without CAE (P = 0.001). A significant positive association was observed between RC levels and the risk of CAE, with a multivariable adjusted odds ratio (OR) of 1.950 (95% confidence interval [CI]: 1.163–3.270). There was a significant positive association between RC levels and the risk of CAE in both single-vessel and multivessel dilation cases, as well as in isolated CAE and dilation secondary to coronary atherosclerosis. According to the subgroup analyses, RC levels were positively associated with the risk of CAE in participants with hypertension (OR, 1.065; 95% CI, 1.034–1.098).
Conclusion
RC levels are positively correlated with CAE, implying that a focus on RC could be beneficial in CAE research.
Similar content being viewed by others
Introduction
Coronary artery ectasia (CAE), also known as coronary artery aneurysm (CAA), is characterized by the abnormal dilation or widening of one or more coronary arteries, where the affected artery’s diameter exceeds 1.5 times that of the adjacent normal segment [1, 2]. CAE is often discovered incidentally during coronary angiography or computed tomography, with estimated incidence rates ranging from 0.3 to 5%. Clinical symptoms vary from incidental findings to acute coronary syndrome, which is associated with an increased risk of acute myocardial infarction [3,4,5]. Men are more commonly affected than women are, and the condition tends to be more prevalent in the proximal segments of the coronary bed than in the distal segments [2]. The cause of CAE remains unknown, but it is believed to be associated with a combination of genetic predisposition and various risk factors, including atherosclerosis, inflammation, connective tissue disorders, abnormal lipoprotein levels, and vasculitis [6,7,8,9].
Sudhir et al. reported that patients with CAE presented a significant decrease in HDL-C levels, an increase in LDL-C levels, and a significant increase in the LDL/HDL ratio. Research by Jafari and collaborators revealed that HDL-C levels were inversely associated with the progression of CAE, whereas an increase in hemoglobin significantly influences the onset of CAE [10,11,12]. Therefore, the occurrence of CAE is closely associated with lipid levels.
Remnant cholesterol (RC) is derived by deducting both high-density lipoprotein cholesterol (HDL-C) and low-density lipoprotein cholesterol (LDL-C) from total cholesterol (TC), including intermediate-density lipoprotein (IDL), very-low-density lipoprotein (VLDL), and chylomicron remnants [13,14,15]. RC circulates in the plasma and accumulates in the subendothelial space, leading to vascular inflammation, which might serve as a mechanism for vascular dilation [13]. No research has previously investigated the relationship between RC levels and CAE. In this study, the objective was to explore the correlation between RC levels and the occurrence of CAE.
Methods
Study population
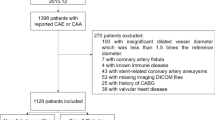
This study was a retrospective analysis of patients who underwent coronary angiography (CAG) at Guangdong Provincial People’s Hospital from January 2017 to July 2022. The Guangdong Provincial People’s Hospital performs approximately 5000 coronary angiography procedures annually, resulting in an estimated total of 30,000 CAG procedures performed from January 2017 to July 2022.
The study population was categorized into three groups: isolated CAE, CAD with dilation, and control. The inclusion criteria were as follows: for patients who underwent coronary angiography, isolated CAE was defined as one or more coronary arteries that were ≥ 1.5 times larger than their adjacent normal counterparts. CAD with dilation was diagnosed in patients who had partial stenosis of more than 50% and partial dilation ≥ 1.5 times larger than the adjacent normal segments in the same vessel. The control group consisted of individuals who underwent coronary angiography with the same operator and during the same period as the CAE patients and who had negative results. The exclusion criteria were as follows: age < 18 years, previous coronary artery bypass grafting or stenting, severe valvular disease, malignancy, Kawasaki disease, and acute or chronic inflammatory disease.
According to the inclusion and exclusion criteria, 306 patients with coronary artery dilatation were included. Among these patients, 143 had isolated CAE, 21 of whom had missing data, and the remaining 163 had coronary artery disease (CAD) with dilation, 25 of whom had missing data. Thus, 260 patients were selected for inclusion in this study. The control group comprised 419 individuals with normal coronary angiograms.
The study was approved by the Guangdong Provincial People’s Hospital Ethics Committee. Since this retrospective study involved only chart review, the patient consent requirement was waived.
Data collection
The demographics, clinical characteristics and cardiovascular risk factors (age, sex, drinking or smoking status, and medication use) of patients were collected by a resident physician. Upon admission, blood was extracted from patients’ veins for the purpose of conducting biochemical and routine blood tests. The following blood biochemical parameters were measured: triglyceride (TG), total cholesterol (TC), HDL-C, LDL-C, apolipoprotein A1 (ApoA1), apolipoprotein B100 (ApoB100), lipoprotein a, glucose, high-sensitivity C-reactive protein (hsCRP), and creatinine. RC was calculated as TC minus HDL-C minus LDL-C, with the values for TC, HDL-C, and LDL-C measured by the laboratory department of Guangdong Provincial People’s Hospital. Smoking status was categorized as current (smoking more than one pack per day for more than six months), former, or never. Drinking status data were collected by experienced resident physicians and categorized as current (alcohol consumption once or more per week), former, or never. Diabetes mellitus was defined as a fasting glucose level ≥ 126 mg/dL, a nonfasting glucose level ≥ 200 mg/dL, a self-reported diagnosis of diabetes mellitus, or a history of using hypoglycemic medications [16]. Hypertension was defined as having 3 consecutive SBP readings ≥ 140 mm Hg or DBP ≥ 90 mm Hg, self-reported a diagnosis of hypertension or a history of using antihypertensive medications [17]. Hyperlipidemia was defined as a total serum cholesterol level ≥ 200 mg/dL, a self-reported diagnosis of hyperlipidemia or a history of use of lipid-lowering medications. The UHR is the uric acid/HDL ratio.
Statistical analysis
Categorical variables are presented as numbers (percentages). Continuous variables with a normal distribution are presented as the means ± SDs, whereas nonnormally distributed variables are presented as the medians (interquartile ranges). For continuous variables, either analysis of variance (ANOVA) or the Kruskal–Wallis h test was applied as appropriate. For categorical variables, differences between groups were assessed via the χ2 test. RC was categorized into four quartiles, with the lowest quartile serving as the reference group. The relationship between RC concentrations and the risk of CAE was assessed through forwards logistic regression analysis, yielding OR and 95% CI. Restricted cubic spline regression was also used to assess the association between RC levels and the risk of CAE. Statistical analyses were conducted via SPSS software (version 26.0).
Results
As shown in Fig. 1, the cohort study included 679 patients over 6 years. The CAE group consisted of 260 patients, whereas the control group comprised 419 patients without CAE (Fig. 1).
Baseline characteristics
The clinical characteristics of the patients in the study group are shown in Table 1. The mean ± SD age of all the patients was 59.9 ± 10.8 years, 444 (65.4%) were men, 121 (17.8%) were current smokers, 67 (9.9%) were current drinkers, 307 (45.2%) had hypertension, 115 (16.9%) had diabetes, and 96 (14.1%) had hyperlipidemia. Compared with those without CAE, individuals with CAE were more likely to be male (P < 0.001), have a higher BMI (P = 0.009), and be smokers (P = 0.016). Additionally, they had a greater proportion of patients with hypertension (P < 0.001), diabetes (P = 0.003), and hyperlipidemia (P < 0.001), along with a greater use of antihypertensive medications (P < 0.001), hypoglycemic medication (P = 0.015), and lipid-lowering medication (P < 0.001). Moreover, no notable differences in age, SBP, DBP, or alcohol consumption status were observed between the two groups (Table 1).
Biochemical and hematological measurements
Table 2 shows the biochemical and hematological characteristics of the study population. RC was greater in the CAE group (P = 0.001), whereas the HDL-C and ApoA1 levels were greater in the control group (P < 0.001). Additionally, lipoprotein(a), triglyceride, and the LDL-C/HDL-C ratio were elevated in the CAE group (P = 0.044, P = 0.006, and P < 0.001, respectively). The serum creatinine level, hsCRP level, fibrinogen level, hemoglobin level, white blood cell count, uric acid level, and UHR were also greater in the CAE group (all P < 0.05). Total cholesterol, LDL-C, non-HDL-C, ApoB, and fasting glucose levels were similar among the groups.
Association between RC levels and CAE
Logistic regression analysis was performed to identify factors that independently predict the existence of ectatic arteries in the 4 different adjusted models (Table 3). The baseline characteristics of the participants stratified by RC quartiles are shown in Table S1. All the models demonstrated a statistically significant positive association between RC levels and the risk of CAE. According to the unadjusted model, the OR (95% CI) for the highest group compared with the lowest was 1.889 (1.219–2.929). Moreover, in Model 1, which was adjusted for RC quartiles, age, sex and body mass index, the OR (95% CI) for the highest group compared with the lowest was 1.675 (1.061–2.645). In Model 2, which was the fully adjusted model, further adjustments were made on the basis of Model 1. These adjustments included those for systolic blood pressure, fasting glucose, use of antihypertensive medication, use of lipid-lowering medication, smoking status, and drinking status. The OR (95% CI) for the highest group compared with the lowest was 1.950 (1.163–3.270). In Model 2, with RC levels included as a continuous variable, a one-unit increase in RC was correlated with a 3.4% higher risk of CAE (OR, 1.034; 95% CI, 1.015–1.054). The significant associations between RC levels and the risk of CAE remained after further adjustment for HDL-C levels (Model 3 in Table 3). When HDL-C, ApoA1, and triglyceride concentrations were considered continuous variables, in the fully adjusted Model 2, the significant associations of HDL-C and ApoA1 concentrations with the risk of CAE remained evident; however, the significant association between triglyceride concentrations and the risk of CAE was no longer evident (Table S2). Multivariable-adjusted spline regression models indicated that RC levels were linearly associated with the risk of CAE (Fig. 2).
Adjusted odds ratios of incident CAE by RC. The odds ratio was adjusted for age, body mass index, sex, systolic blood pressure, fasting glucose, antihypertensive medication use, lipid-lowering medication use, smoking status and drinking status. The red solid line represents the odds ratio of RC across the whole range. The red dotted line represents the 95% CI. The black dotted line is the reference line, with an odds ratio of 1. Histograms represent the frequency distributions of RC
Associations between RC concentrations and the risk of different types of CAE
The correlation between the number of dilated vessels and RC in individuals with CAE is shown in Table 4. RC levels were associated with the risk of CAE in both single-vessel dilation cases and multivessel dilation cases (all P < 0.05, Table 4). The analysis depicted in Table 5 revealed associations between RC levels and the risk of different types of CAE. The risk of both isolated CAE and dilation secondary to coronary atherosclerosis were associated with RC levels (all P < 0.05, Table 5).
Subgroup analyses
Further subgroup analysis was conducted, and the results are presented in Fig. 3. The participants were stratified by age, sex, body mass index, and diabetes status, and the association between RC levels and the risk of CAE remained evident (Fig. 3). However, a differential association was observed if the subgroups were divided by hypertension, indicating that the relationship was stronger in those with prevalent hypertension (interaction P = 0.002; Fig. 3).
Subgroup analyses of the association between RC concentrations and the risk of CAE. Adjusted for age, body mass index, sex, systolic blood pressure, fasting glucose, antihypertensive medication use, lipid-lowering medication use, smoking status, drinking status, hypertension, and diabetes, except for the stratification factor itself
Discussion
This research demonstrated a connection between RC concentrations and the risk of CAE for the first time, independent of conventional cardiovascular risk factors. Higher RC levels were positively associated with the occurrence of CAE. Additionally, an association between RC levels and the risk of CAE was discovered in both single-vessel and multivessel dilation cases. Moreover, the risk of both isolated CAE and dilation secondary to coronary atherosclerosis were correlated with RC levels. Subgroup analysis revealed a stronger association between RC levels and the risk of CAE among participants with hypertension. Additionally, individuals with CAE presented lower HDL-C levels and a greater LDL-C/HDL-C ratio than did the control individuals. These findings are consistent with cases of familial hypercholesterolemia and the findings reported in the study by Jafari et al. [10, 11]. Furthermore, ApoA1 levels were decreased in patients with CAE, whereas triglyceride levels were increased. After full adjustment, the significant associations of HDL-C and ApoA1 concentrations with the risk of CAE remained evident, whereas the significant association between triglyceride concentrations and the risk of CAE disappeared. Patients with CAE had a higher prevalence of hypertension. Moreover, in the subgroup analysis, the relationship between RC levels and the risk of CAE was stronger in those with hypertension. Hypertension might lead to turbulent blood flow and increased shear stress, resulting in enhanced remodelling and dilation of the coronary arteries [18]. In this study, consistent with the findings of Sincer et al., elevated hsCRP levels and an increased white blood cell count were observed in the CAE group [19]. Moreover, several studies have posited that inflammation is a key mechanism underlying CAE [18, 20]. The present study also revealed that uric acid concentrations and the UHR were greater in the CAE group than in the control group, which is consistent with the findings of Mansiroglu et al. [21].
Increasing evidence indicates that triglycerides, or RC, which are predominantly carried in plasma by TGRL, might play an important role in CVD risk. RC, a crucial cholesterol component, constitutes one-third of total cholesterol and contributes to 50% of the cholesterol found in atherosclerotic plaques. As the main protein constituent of HDL-C particles, both ApoA1 and HDL-C are generally considered to offer protection against atherosclerosis [22, 23]. CAE, a relatively rare cardiovascular condition, has been noted in various other conditions, such as Kawasaki disease; autoimmune diseases (including scleroderma, lupus erythematosus, and polyarteritis nodosa); connective tissue disorders (such as Marfan and Ehlers–Danlos syndrome); bacterial infections (such as Lyme disease and syphilis); and infrequent cases related to trauma, cocaine, or congenital factors [24]. Indeed, there is debate over whether CAE should be viewed as a subset of atherosclerosis or as a distinct condition [7, 25]. While increasing evidence suggests that lipoproteins play a significant role in atherosclerosis development, their impact on CAE remains unclear. These results indicate that RC could be a potential therapeutic target for reducing CAE risk. Consequently, further research is needed to uncover new mechanisms that elucidate the relationship between RC levels and the risk of CAE.
Strengths and limitations
This study has several strengths. This is the first study to demonstrate the association between RC concentrations and the risk of CAE. Additionally, RC concentrations were independently associated with an increased CAE risk, even after adjusting for various confounders. However, there are several limitations to this study. First, the number of enrolled patients was relatively small due to the low incidence of CAE. Second, this was a cross-sectional study, which allowed for the description of the condition but did not allow for the determination of causality. Third, the patients included in this study were exclusively inpatients at Guangdong Provincial People’s Hospital, which may have resulted in selection bias. Finally, although adjustments for relevant covariates were made as much as possible, the results may still have been influenced by multiple confounding factors. Hence, further studies are needed to validate these findings.
Conclusion
This cross-sectional analysis revealed a positive correlation between fasting RC levels and the risk of CAE. These findings suggest that lowering RC levels might be beneficial for preventing and managing CAE in patients. Further research is needed to confirm these results, elucidate the mechanisms linking RC to CAE, and explore the benefits of long-term RC-lowering treatments for CAE patients.
Data availability
The data that support the findings of this study are available from Guangdong Provincial People’s Hospital but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Guangdong Provincial People’s Hospital. No datasets were generated or analysed during the current study.
Abbreviations
- CAE:
-
Coronary Artery Ectasia
- RC:
-
Remnant cholesterol
- TC:
-
Total cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- IDL:
-
Intermediate-density lipoprotein
- VLDL:
-
Very-low-density lipoprotein
- CAG:
-
Coronary angiography
- CAD:
-
Coronary artery disease
- TG:
-
triglyceride
- ApoA1:
-
Apolipoprotein A1
- ApoB100:
-
Apolipoprotein B100
- hsCRP:
-
high-sensitivity C-reactive protein
- UHR:
-
Uric acid/HDL ratio
- BMI:
-
Body mass index
References
Fukamachi D, Okumura Y. Growing giant coronary artery aneurysm. Eur Heart J. 2022;43(48):5065.
Kawsara A, Nunez GI, Alqahtani F, Moreland J, Rihal CS, Alkhouli M. Management of coronary artery aneurysms. JACC Cardiovasc Intervent. 2018;11(13):1211–23.
Manginas A, Cokkinos DV. Coronary artery ectasias: imaging, functional assessment and clinical implications. Eur Heart J. 2006;27(9):1026–31.
Cai Z, Li L, Wang H, Yuan S, Yin D, Song W, Dou K. Effect of type 2 diabetes on coronary artery ectasia: smaller lesion diameter and shorter lesion length but similar adverse cardiovascular events. Cardiovasc Diabetol. 2022;21(1):9.
Fukamachi D, Okumura Y. Giant coronary-artery aneurysm. N Engl J Med. 2022;387(11):e23.
Eid MM, Mostafa MR, Alabdouh A, AbdelQadir YH, Mohamed S, Abdelazeem B, Ismayl M, Abusnina W, Alweis R, Corteville D, et al. Long-term outcomes of Acute myocardial infarction in pre-existing coronary artery ectasia: a systematic review and Meta-analysis. Curr Probl Cardiol. 2023;48(5):101626.
Dahhan A. Coronary artery ectasia in atherosclerotic coronary artery disease, inflammatory disorders, and sickle cell disease. Cardiovasc Ther. 2015;33(2):79–88.
Doi T, Kataoka Y, Noguchi T, Shibata T, Nakashima T, Kawakami S, Nakao K, Fujino M, Nagai T, Kanaya T, et al. Coronary artery Ectasia predicts future cardiac events in patients with Acute myocardial infarction. Arterioscler Thromb Vasc Biol. 2017;37(12):2350–5.
Antoniadis AP, Chatzizisis YS, Giannoglou GD. Pathogenetic mechanisms of coronary ectasia. Int J Cardiol. 2008;130(3):335–43.
Sudhir K, Ports TA, Amidon TM, Goldberger JJ, Bhushan V, Kane JP, Yock P, Malloy MJ. Increased prevalence of coronary ectasia in heterozygous familial hypercholesterolemia. Circulation. 1995;91(5):1375–80.
Jafari J, Daum A, Hamed JA, Osherov A, Orlov Y, Yosefy C, Gallego-Colon E. Low high-density lipoprotein cholesterol predisposes to coronary artery Ectasia. Biomedicines. 2019;7(4).
Jiang L, Wei W, Kang S, Li XL, Luo Y. Insights into lipid metabolism and immune-inflammatory responses in the pathogenesis of coronary artery ectasia. Front Physiol. 2023;14:1096991.
Varbo A, Nordestgaard BG. Remnant cholesterol and Triglyceride-Rich Lipoproteins in atherosclerosis progression and Cardiovascular Disease. Arterioscler Thromb Vasc Biol. 2016;36(11):2133–5.
Wu X, Qiu W, He H, Zhao G, Liu J. Associations of the triglyceride-glucose index and remnant cholesterol with coronary artery disease: a retrospective study. Lipids Health Dis. 2024;23(1):45.
Burnett JR, Hooper AJ, Hegele RA. Remnant cholesterol and atherosclerotic Cardiovascular Disease Risk. J Am Coll Cardiol. 2020;76(23):2736–9.
American Diabetes Association Professional Practice Committee. 2. Diagnosis and Classification of Diabetes: Standards of Care in Diabetes-2024. Diabetes Care. 2024;47:S20–42.
Brouwers S, Sudano I, Kokubo Y, Sulaica EM. Arterial hypertension. Lancet. 2021;398(10296):249–61.
Jeudy J, White CS, Kligerman SJ, Killam JL, Burke AP, Sechrist JW, Shah AB, Hossain R, Frazier AA. Spectrum of coronary artery aneurysms: from the radiologic pathology archives. Radiographics. 2018;38(1):11–36.
Sincer I, Akturk E, Acikgoz N, Ermis N, Kosar MF. Evaluation of the relationship between serum high sensitive C-reactive protein and the elasticity properties of the aorta in patients with coronary artery ectasia. Anadolu Kardiyol Derg. 2011;11(5):414–20.
Ozturk S, Yetkin E, Waltenberger J. Molecular and cellular insights into the pathogenesis of coronary artery ectasia. Cardiovasc Pathol. 2018;35:37–47.
Asli Kurtar M, Mehmet C, Isa S, Yilmaz G. A promising marker in patients with coronary artery ectasia: uric acid / HDL ratio. Ann Med Res. 2021;2(28):312–5.
Balling M, Langsted A, Afzal S, Varbo A, Davey SG, Nordestgaard BG. A third of nonfasting plasma cholesterol is in remnant lipoproteins: lipoprotein subclass profiling in 9293 individuals. Atherosclerosis. 2019;286:97–104.
Chistiakov DA, Orekhov AN, Bobryshev YV. ApoA1 and ApoA1-specific self-antibodies in cardiovascular disease. Lab Invest. 2016;96(7):708–18.
Baman TS, Cole JH, Devireddy CM, Sperling LS. Risk factors and outcomes in patients with coronary artery aneurysms. Am J Cardiol. 2004;93(12):1549–51.
Aksu T, Uygur B, Durukan KM, Guray U, Arat N, Korkmaz S, Colak A. Coronary artery ectasia: its frequency and relationship with atherosclerotic risk factors in patients undergoing cardiac catheterization. Anadolu Kardiyol Derg. 2011;11(4):280–4.
Acknowledgements
Not applicable.
Funding
This research was funded by Guangzhou Municipal Science and Technology Bureau, Guangzhou Key Research and Development Program, grant number 2024B03J1340, and the Natural Science Foundation of Guangdong Province, grant number 2022A1515012598.
Author information
Authors and Affiliations
Contributions
These should be presented as follows: JM participated in data collection, data analysis and article writing. YW participated in data collection and data analysis. ZX and JX participated in data collection. YH and XH participated in data analysis. HY participated in design of study, supervision and project administration. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Research Ethics Committee of Guangdong Provincial People’s Hospital (KY2023-699-01).
Consent for publication
Before participating in the study, all participants signed up with informed permission.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mu, J., Weng, Y., Xiao, J. et al. Association of remnant cholesterol with coronary artery ectasia: a cross-sectional study. Lipids Health Dis 23, 240 (2024). https://doi.org/10.1186/s12944-024-02225-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-024-02225-7